Abstract
Purpose
To evaluate the feasibility of the interferon-gamma release assay (IGRA) as a supplementary diagnostic tool for the diagnosis of genitourinary tuberculosis (GUTB).
Materials and Methods
Fifty-seven patients who were tested with the IGRA to diagnose GUTB were included. All patients had clinical or radiologic features suspicious for GUTB. Signs and symptoms included chronic dysuria with long-standing sterile pyuria, renal calcification with distorted renal calyces and contracted renal pelvis, and chronic epididymitis. Patients who had a history of tuberculosis in other organs were excluded. Tests including IGRA, urine acid-fast bacilli (AFB) stain and culture, urine tuberculosis polymerase chain reaction (UT-PCR), and radiological examinations were performed to confirm GUTB. The medical records of the patients were reviewed retrospectively.
Results
The IGRA result was positive in 30 patients (52.6%). The results of the urine AFB stain and culture were positive in 5 patients (8.8%) and 7 patients (12.2%), respectively. The results of UT-PCR were positive in 9 patients (15.8%). The 7 patients who showed positive results in the urine AFB stain and culture also had positive results on the IGRA. A UT-PCR-negative patient was diagnosed with GUTB by positive results on both the IGRA and AFB stain and culture.
In developing countries, tuberculosis is a major public health issue. Because Korea is an area endemic for tuberculosis, preventive immunization for tuberculosis is currently performed for infants. Even in endemic areas, genitourinary tuberculosis (GUTB) is very rare compared with pulmonary tuberculosis. The number of new patients with tuberculosis in Korea was 32,010 (67.2 in 100,000) in 2002 and 30,687 (64 in 100,000) in 2003. In 2008, the number of new patients with extrapulmonary tuberculosis (EPTB) was 5,813, which accounted for 17.0% of all new patients with tuberculosis. Finally, 123 patients (0.4%) were diagnosed with GUTB [1].
Repeated acid-fast bacilli (AFB) stains and cultures of the first urine sample in the morning have been used as conventional and standard tests to confirm urological tuberculosis. Because a single sampling of concentrated urine has a sensitivity as low as 30% to 40% [2], repeated sampling (3 to 6 times) could increase sensitivity up to 80% to 90% and should be mandatory. Frequently, intravenous pyelogram (IVP), ultrasonography, computed tomography (CT), and magnetic resonance imaging are needed as ancillary studies. In 2000, the interferon-gamma release assay (IGRA) was developed as a diagnostic tool for tuberculosis [3]. In this method, the amount of interferon-gamma released from T-lymphocytes is measured after the lymphocytes are stimulated with tuberculosis antigen. The Quantiferon-TB gold in-tube kit (Cellestis, Victoria, Australia) and T-SPOT.TB (Oxford Immunotec Ltd., Oxford, UK) are the currently available commercial kits. The clinical sensitivity and specificity of these methods have not been evaluated in urological tuberculosis, however. Thus, we investigated their feasibility for the diagnosis of urological tuberculosis.
Fifty-seven patients from a single urology clinic with symptoms or radiologic findings suggestive of GUTB between March 2009 and August 2011 were evaluated retrospectively. The symptoms suggestive of GUTB included dysuria, frequency, urgency or hematuria with sterile pyuria, recurrent or chronic scrotal pain with beaded palpable nodules in the epididymis, and intermittent flank discomfort with radiologically chronic inflammation in the renal pelvis and ureter. The radiological findings suggestive of GUTB included renal calcification with chronic inflammatory changes in the kidney, a small contracted bladder and calyceal dilation or destruction with a contracted renal pelvis, and others. Patient profiles, clinical presentations, involved organs, and the results of diagnostic tests were reviewed. The evaluation of the patients included detailed medical histories and physical examinations followed by a complete blood count, chemical battery, routine urinalysis, and urine cultures. Urine AFB stains and mycobacterial cultures sampled in the early morning were obtained either 1 or 2 times. Radiologic evaluations included IVP or CT scans of the kidney, ureter, and bladder regions in all patients. The scans were interpreted by a panel of radiologists. This study was approved by the institutional review board of Hallym University Sacred Heart Hospital (Institutional Review Board approval number: 2012-I065).
Patients who had a history of tuberculosis in other organs, including the lung and lymph nodes, were excluded from this study. The patients were tested by use of the urine AFB stain, urine AFB culture, urine tuberculosis polymerase chain reaction (UT-PCR), and IGRA. The commercially available Quantiferon-TB gold in-tube kit (Cellestis) was used for the IGRA.
For the Quantiferon-TB gold in-tube assay, 1 mL of whole blood was added to each of the three QFT-TB tubes: the TB antigen tube (ESAT-6, CEP-10, and TB 7.7), the mitogen-positive control tube (phytohemagglutinin), and the negative control tube. The tubes were treated according to the recommendations of the manufacturer (Cellestis), and the interferon (IFN)-gamma concentrations (IU/mL) of the plasma were measured by use of an enzyme-linked immunosorbent assay reader. An IFN-gamma concentration ≥0.35 IU/mL (TB antigen minus negative control) was considered a positive test result. When the mitogen-positive control concentration was not higher than 0.5 IU/mL, an "indeterminate test result" was reported. The results of urine AFB and culture, radiological studies, UT-PCR, and IGRA were compared descriptively.
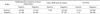
Among the 57 patients, 36 (63.1%) were male and the others (36.9%) were female. The mean age of the patients was 52.0 years. For the chief complaint, 22 patients had flank pain, 11 had dysuria, 11 had gross hematuria, 5 had fever, and 5 had scrotal pain. Three patients complained of nonspecific symptoms such as general myalgia, fatigue, or weight loss. The organs involved that were suspicious for tuberculosis clinically or radiologically were the upper urinary tract in 38 patients, the bladder in 5 patients, and other genital organs in 14 patients. Multiple organs were not involved in our study (Table 1).
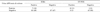
Radiologically, 30 patients (52.6%) had findings suspicious of urologic tuberculosis, and 19 of these patients showed a positive result on the IGRA (Table 2). The result of the urine AFB stain was positive only in 5 patients (8.8%), and urine culture was positive in 7 patients (12.2%). All the patients who showed positive results in the urine AFB stain also had a positive urine culture (Table 2).
The result of the IGRA test was positive in 30 patients (52.6%). All patients who showed positive results on the urine AFB stain and culture also had positive results on the IGRA (Table 3). Nine patients had a positive result for tuberculosis in the urine UT-PCR. Among these UT-PCR-positive patients, the AFB stain and culture were positive in 6 patients (66.6%); however, a UT-PCR-negative patient was reported as having a positive result for the AFB stain and culture for tuberculosis (Table 3).
GUTB was first described by Willbolz et al. (quoted from [4]), and it represents tuberculosis that has spread to the kidney, ureter, testis, and epididymis via a blood-borne infection. Recently, as a subtype of EPTB, it was reported to account for <1.5% of patients with pulmonary tuberculosis [5]. In Korean reports, 0.4% of all patients with tuberculosis were found to have GUTB [1]. Compared with pulmonary tuberculosis, it is relatively difficult to diagnose EPTB. Moreover, official reports are fewer than the actual number of diagnoses. Therefore, the incidence of EPTB, as well as of GUTB, might be underestimated. Early diagnosis could allow for the administration of antitubercular treatment at a curative stage. Unfortunately, the treatment is usually delayed because of delayed symptom presentation and delayed definitive diagnosis. Consequently, a number of patients present with nonfunctioning kidneys, ureteral strictures, and contracted bladders. These situations can be avoided by early diagnosis and effective treatment. Because the clinical symptoms of GUTB are nonspecific and the diagnostic procedure for GUTB is somewhat complicated for patients, clinicians may miss the diagnosis of GUTB, and proper treatment may be delayed in order to undergo surgery. Accordingly, simpler and more efficacious diagnostic tools are necessary for early diagnosis.
The nonspecific symptoms of GUTB make it difficult to define inclusion criteria for patients for the evaluation of new diagnostic tools. Investigators should always consider the diagnosis of GUTB in a patient presenting with vague, long-standing urinary symptoms (dysuria, hesitancy, and frequency) for which there is no obvious cause. The symptoms and signs of GUTB vary in both intensity and duration. In the published literature, the most common presenting symptoms in patients with GUTB are irritative voiding symptoms, flank pain, and hematuria, which are reported around 60% and 50% of the time [6]. The patients in the current study also complained of similar nonspecific symptoms: flank pain was reported in 22 patients (38.5%), dysuria was reported in 11 patients (19.3%), and hematuria was reported in 11 patients (19.3%). Radiologic abnormalities suggesting GUTB are found in 63% to 95% of patients in the literature [7,8], and in the present study, such evidence was found in 52.6% of the patients.
The urine AFB stain and culture are the reference standards for the diagnosis of tuberculosis. A definite diagnosis of GUTB is confirmed by isolation of Mycobacterium tuberculosis (MTb) in the urine AFB stain and culture. However, these tests have their own limitations for use in clinical circumstances, because the discharge of organisms into the urine is sporadic, and few organisms are involved [9]. Direct smears often show negative findings and often cannot differentiate tuberculous from nontuberculous mycobacteria. Although culture is a more sensitive diagnostic tool, it takes 6 to 8 weeks to get the results because of the slow growth rate of mycobacteria [10]. In the current series, the MTb culture result was positive in only 12.2% of cases. In previously published reports, the positive rates varied from 10.7% to 90% [7,11,12].
Although it cannot yet replace AFB stain and culture, because tuberculosis PCR is more specific, more sensitive, simpler, and faster than an AFB stain of a direct smear, it is currently used as a useful supplementary tool [2]. The sensitivity of PCR for pulmonary TB is 97% and the specificity is 76% [13]. However, the efficacy of PCR for the diagnosis of EPTB, including GUTB, is not conclusive. A PCR test of a specimen excised from the organs suspicious for EPTB would be very helpful for the diagnosis; however, because of the low sensitivity of UT-PCR, GUTB cannot be excluded from the differential diagnosis [14].
When pulmonary tuberculosis is suspected on the basis of clinical symptoms but the results of AFB stain and culture are negative, the IGRA for tuberculosis can be helpful. It is especially useful as a diagnostic tool in developed countries, in which the tuberculosis incidence is less than 1%. It is also useful in endemic areas like Korea. Although, in such endemic areas where BCG vaccination is a nationwide prevention policy, a meta-analysis of the pooled sensitivity of IGRA for tuberculosis was 70% to 78% and the specificity was 99% among patients who did not receive BCG vaccination and 96% among BCG-vaccinated persons [15]. Another merit of the IGRA is that only one test is required to obtain high sensitivity. In a previous Korean study, Song et al. [16] reported that the sensitivity and specificity of the IGRA for EPTB were 69% and 82%, respectively. Among the enrolled patients, there were only two GUTB cases.
In the current study, 30 patients had a positive result on the IGRA for tuberculosis; however, only 7 patients had positive results on the AFB stain and culture tests. If we assume that the AFB stain and culture tests are standard diagnostic methods, the 23 IGRA-positive patients might be considered to be false-positives. Otherwise, when we propose that the specificity of the IGRA is around 95% on the basis of the pulmonary tuberculosis study [15], these patients would get the benefit of timely treatment. The low sensitivity values of the AFB stain and culture tests are a very strong limitation. A potential bias of this study may result from the fact that it was a retrospective review. For the proper diagnosis of GUTB, 3 to 6 urine samplings are required to reach a sensitivity of around 90% [2]. In this retrospective review, however, only 1 or 2 urine samplings were obtained. Therefore, on the basis of the results of this study, it is not reasonable to determine that IGRA is superior to AFB stain and culture for the diagnosis of GUTB. On the other hand, when the results from other tests are not reliable in a clinical situation, the IGRA can be helpful for diagnosis. Interestingly, a UT-PCR-negative patient was diagnosed with GUTB by AFB stain and culture and IGRA results. Even though this is just one case, clinicians can consider using the IGRA as a supplementary test for the diagnosis of GUTB, either in combination with UT-PCR or alone.
In conclusion, the IGRA is a simple test, and it is feasible as a supplementary and screening diagnostic tool for GUTB. Because the current retrospective study has several biases and limitations, the authors are planning to perform a prospective study by using the same sampling protocols with clear inclusion criteria.
The IGRA for tuberculosis is a fast and simple serum test that might feasibly be used as a supplementary or screening tool for the diagnosis of GUTB in addition to urine AFB stain and culture. Further studies for statistical evaluation of its sensitivity, specificity, and efficacy are needed.
Figures and Tables
TABLE 1
Characteristics of patients with clinical presentations suspicious for genitourinary tuberculosis

References
1. Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea 2008. 2009. Cheongwon: Korea Centers for Disease Control and Prevention.
2. Long R, Ellis E. Canada Tuberculosis Prevention and Control. Public Health Agency of Canada. Canadian Lung Association. Canadian Thoracic Society. Canadian tuberculosis standards. 2007. 6th ed. Ottawa: Canadian Lung Association/Public Health Agency of Canada.
3. Mazurek GH, LoBue PA, Daley CL, Bernardo J, Lardizabal AA, Bishai WR, et al. Comparison of a whole-blood interferon gamma assay with tuberculin skin testing for detecting latent Mycobacterium tuberculosis infection. JAMA. 2001. 286:1740–1747.
4. Lattimer JK, Uson AC, Melicow MM. Campbell MF, Harrison H, editors. Tuberculous infections and inflammations of the urinary tract. Urology. 1970. 3rd ed. Philadelphia: WB Saunders Company;443–479.
5. Jacob JT, Nguyen TM, Ray SM. Male genital tuberculosis. Lancet Infect Dis. 2008. 8:335–342.
6. Dosanjh DP, Hinks TS, Innes JA, Deeks JJ, Pasvol G, Hackforth S, et al. Improved diagnostic evaluation of suspected tuberculosis. Ann Intern Med. 2008. 148:325–336.
7. Narayana A. Overview of renal tuberculosis. Urology. 1982. 19:231–237.
8. Kollins SA, Hartman GW, Carr DT, Segura JW, Hattery RR. Roentgenographic findings in urinary tract tuberculosis: a 10 year review. Am J Roentgenol Radium Ther Nucl Med. 1974. 121:487–499.
9. Gow JG. Walsh PC, Retik AB, Stamey TA, Vaughan ED, editors. Genito urinary tuberculosis. Campbell's urology. 1992. 6th ed. Philadelphia: WB Saunders;951–981.
10. Manjunath N, Shankar P, Rajan L, Bhargava A, Saluja S, Shriniwas . Evaluation of a polymerase chain reaction for the diagnosis of tuberculosis. Tubercle. 1991. 72:21–27.
11. Colabawalla SN. Reflections on urogenital tuberculosis. Indian J Urol. 1990. 6:51–59.
12. Gow JG, Barbosa S. Genitourinary tuberculosis: a study of 1117 cases over a period of 34 years. Br J Urol. 1984. 56:449–455.
13. Cousins DV, Wilton SD, Francis BR, Gow BL. Use of polymerase chain reaction for rapid diagnosis of tuberculosis. J Clin Microbiol. 1992. 30:255–258.
14. British National Institute for Health and Clinical Excellence. Clinical diagnosis and management of tuberculosis, and measures for its prevention and control. 2006. London: National Institute for Health and Clinical Excellence.
15. Pai M, Zwerling A, Menzies D. Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann Intern Med. 2008. 149:177–184.
16. Song KH, Jeon JH, Park WB, Kim SH, Park KU, Kim NJ, et al. Usefulness of the whole-blood interferon-gamma release assay for diagnosis of extrapulmonary tuberculosis. Diagn Microbiol Infect Dis. 2009. 63:182–187.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download