Abstract
Purpose
Prostatic abscess is an uncommon urologic disease but has a high mortality rate if not treated properly. Furthermore, diagnosis and proper treatment of prostatic abscesses remains a challenge for physicians. Therefore, we compared data on conservative treatments, transurethral resection of prostatic abscess, and transrectal ultrasound (TRUS)-guided needle aspiration in 52 cases over a 10-year period.
Materials and Methods
The records of 52 patients diagnosed with prostatic abscess by computed tomography at Gangnam Severance Hospital between January 2000 and September 2010 were retrospectively reviewed. All patients were discharged when their leukocytosis had normalized and they had been free of fever for 2 days. Multivariate regression analysis was done to determine independent risk factors for the length of hospitalization.
Results
At the time of diagnosis, the average age of the 52 patients was 61.3 years (range, 33 to 81 years), the average volume of the prostate was 56.3 ml (range, 21 to 223 ml), the average prostate-specific antigen was 18.54 ng/ml (range, 2.0 to 57.0 ng/ml), and the average abscess size was 3.8 cm (range, 2.1 to 5.5 cm). All patients were treated with parenteral antibiotics during their hospital stay with intravenous antibiotics (fluoroquinolone monotherapy or 3rd-generation cephalosporin in combination with an aminoglycoside). Of 52 patients, 22 had diabetes mellitus (42.3%), 19 had hypertension (36.5%), and 7 (13.5%) had paraplegia due to spinal cord injury. The most common symptoms were fever (47, 90.4%), perineal discomfort (43, 82.7%), dysuria (40, 76.9%), and urinary retention (29, 55.8%). Prostatic abscesses were treated by conservative treatment (11 cases), transurethral resection of prostatic abscess (23 cases), and TRUS-guided needle aspiration (18 cases). The average hospitalization stay was 17.5 days (range, 6 to 39 days); that of conservative treatment patients was 19.1 days (range, 9 to 39 days). Patients treated by transurethral resection of prostatic abscess and TRUS-guided needle aspiration stayed 10.2 days (range, 6 to 15 days) and 23.25 days (range, 18 to 34 days), respectively. Of the 18 cases who underwent needle aspiration, prostatic abscesses recurred in 4 cases (22.2%) within 1 month after patient discharge. The 2 patients subjected to conservative treatment died due to sepsis. We found no independent factors that affected the average hospitalization period.
Prostatic abscess is a rare clinical occurrence in the antibiotic era and is difficult to diagnose because clinical presentations may mimic several other diseases of the lower urinary tract, such as dysuria, urgency, and frequency. In particular, differential diagnosis between acute bacterial prostatitis and prostatic abscess is difficult on the basis of clinical symptoms and examinations [1,2]. Prostatic abscess has a high mortality rate if adequate and proper treatment does not take place. It may result in severe complications and even urosepsis and death [3]. Therefore, diagnosis and proper treatment of prostatic abscess remains a challenge for physicians.
Once clinical suspicion of prostatic abscess is established, parenteral or oral administration of antibiotics and a surgical drain are needed to diminish severe complications [4]. Traditionally, an open perineal drain or transurethral resection of the prostatic abscess is used [5-7]; nowadays, a minimally invasive procedure like transrectal ultrasound (TRUS)-guided needle aspiration is preferable [8-10].
There are few reports about which treatment is more effective for prostatic abscess. In this study, we compared three groups of data on conservative treatment, transurethral resection of prostatic abscess, and TRUS-guided needle aspiration at the point of hospitalization stay and the recurrence rate in 52 cases over a 10-year period.
Our retrospective study covered a period of 10 years between January 2000 and September 2010. During this period, 52 patients at our hospital were diagnosed with prostatic abscesses by use of computed tomography (CT). Patients with clinically suspicious prostatic abscesses who were not evaluated by CT were excluded. The data were collected retrospectively from the medical records.
All cases included a medical history, physical examination, several blood tests with culture, and urine analysis with culture. Prostatic abscesses were diagnosed with CT. All patients were initially treated with parenteral antibiotics during their hospital stay: either intravenous fluoroquinolone monotherapy or third-generation cephalosporin in combination with an aminoglycoside. A suprapubic Foley catheter was left indwelling if patients experienced urinary retention. All patients were treated in the hospital until their leukocytosis was normalized and they had been free of fever for 2 days. Transurethral resection of prostatic abscess was performed under general anesthesia and needle aspiration was performed transperineally under local anesthesia with TRUS guidance by a radiologist.
Statistical analysis was performed by using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) software. The significance of differences in age, prostate volume, and prostate-specific antigen (PSA) concentration among groups on the basis of treatment methods was examined by using the Kruskal-Wallis test with the Dunn post hoc test. Fisher's exact test was used to compare categorical variables (e.g., clinical symptoms). The data are expressed as the mean±standard deviation or median and range. Multiple linear regression analysis was done to determine independent risk factors for the length of hospitalization in patients with prostatic abscesses. All p-values less than 0.05 were considered statistically significant.
The demographic and clinical features of the 54 patients with prostatic abscesses according to treatment method are shown in Table 1. At the time of diagnosis, the mean age of the patients was 61.34 years (range, 33 to 81 years). Of 52 patients, 22 (42.3%) had diabetes mellitus, 19 (36.5%) had hypertension, and 7 (13.5%) had paraplegia due to spinal cord injury. There were no significant differences in the distribution of ages or the history of hypertension and diabetes mellitus between the three treatment groups of conservative treatment, transrectal resection of the prostate, and TRUS-guided needle aspiration. The most common symptoms were fever (47, 90.4%), perineal discomfort (43, 82.7%), dysuria (40, 76.9%), and urinary retention (29, 55.8%). Some patients experienced myalgia (18, 34.6%) and gross hematuria (9, 17.3%).
Prostatic abscess characteristics and microbiological data are shown in Table 1. The average volume of the prostate was 56.3 ml (range, 21 to 223 ml), the average PSA was 18.54 ng/ml (range, 2.0 to 57.0 ng/ml), and the average abscess size was 3.88 cm (range, 2.0 to 6.0 cm). The results of the urine culture tests showed that the most common pathogens were Escherichia coli (21, 40.4%) followed by Klebsiella pneumoniae (9, 17.3%), Pseudomonas aeruginosa (8, 15.4%), Staphylococcus aureus (4, 7.7%), and Streptococcus agalactiae (2, 3.8%).
Prostatic abscesses were treated by conservative treatment (11 cases), transurethral resection of prostatic abscess (23 cases), and TRUS-guided needle aspiration (18 cases). The average hospitalization stay was 17.5 days (range, 6 to 39 days); that of the conservative treatment patient group was 19.08 days (range, 9 to 39 days). Patients treated by transurethral resection of prostatic abscess and TRUS-guided needle aspiration stayed 10.22 days (range, 7 to 21 days) and 23.25 days (range, 6 to 32 days), respectively. Of the 18 cases who underwent needle aspiration, prostatic abscesses recurred in 4 cases (22.2%) within 1 month after discharge from the hospital. The 2 patients subjected to conservative treatment died due to sepsis.
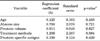
Age, mean PSA, mean prostate volume, mean abscess size, hospital stay, recurrence, and death were examined by using the Kruskal-Wallis test with the Dunn post hoc test. There was a statistically significant difference (p=0.002) in hospital stay (Table 1). On the basis of that result, the independent factors (age, abscess size, prostate volume, treatment methods, and PSA) that could affect hospital stay (days) were examined by multiple linear regression analysis. We found no meaningful independent factors (Table 2).
Prostatic abscess is uncommon because of the wide use of broad-spectrum antibiotics in patients with lower urinary tract symptoms [11]. When not adequately treated or when treatment is delayed, prostatic abscess can progress to sepsis and death [3]. Accurate diagnosis and efficient treatment are thus required. However, there is no standardization of the diagnostic and therapeutic routine for prostatic abscess [10,12].
The signs and symptoms of prostatic abscess are routinely fever, chilling, urinary frequency, acute urinary retention, dysuria, perineal or lower back pain, and hematuria [1,13]. The findings on a digital rectal examination can often detect fluctuant mass. The signs, symptoms, and results of the physical examination of prostatic abscess are similar to those of acute bacterial prostatitis; thus, it is difficult to diagnosis prostatic abscess alone. However, it is very important to distinguish between acute bacterial prostatitis and prostatic abscess, because the therapeutic approach for each is different [14].
Since the advent of antibiotic therapy, the type of organisms responsible for the development of prostatic abscess has changed. In the preantibiotic era, Neisseria gonorrhoeae was the primary organism and was responsible in 75% of cases. In the antibiotic era, gram-negative bacilli (chiefly E. coli) have caused about 60% to 80% of cases. Other significant pathogens include Pseudomonas species, Staphylococcus species, and occasionally obligate anaerobic bacteria [1,15].
Numerous factors have been described in the literature in association with prostatic abscess formation. It is thought that the retrograde flow of contaminated urine within the prostate during micturition is the most prevalent pathogenic factor. Indwelling catheters, a recent prostate biopsy, and instrumentation of the lower urinary tract can be risk factors for prostatic abscess [16]. Bacterial hematogenous spread from distant foci has also been described, such as from respiratory (bronchitis, otitis), digestive (appendicitis, diverticulitis), and urinary tract (perirenal abscess) infections or from the skin (furuncles, abrasions). In these cases, germs like S. aureus, Mycobacterium tuberculosis, E. coli, and Candida sp. may be found [1].
Prostatic abscess is difficult to diagnosis through the signs, symptoms, and physical examination. Prostatic imaging study such as TRUS, CT, and magnetic resonance imaging is important in the diagnosis and treatment. TRUS can be used initially and easily to make a diagnosis of prostatic abscess. The most common TRUS finding is one or more hypoechoic areas with well-defined and thick walls containing thick liquid fluid [17]. TRUS can be interpreted variously in other conditions such as neoplastic processes, cystic lesions, or granulomas. Thus, in the initial stages of abscess formation, it may be inconclusive. TRUS can also cause pain to patients, and abscess size may be changed with the angle of TRUS. CT of the abdomen and pelvic area causes no pain to patients, is less subject to the point of view of the inspector, and can help to detect contiguous spread of infection in nearby organs [18].
Studies of the treatment of prostatic abscess were done several decades ago. Ludwig et al. [19] reviewed a series of 18 patients and suggested that a monofocal abscess of less than 1 cm in diameter be treated with intravenous broad-spectrum antibiotic therapy and a suprapubic catheter. Surgical drainage should be performed for multifocal abscesses greater than 1 cm in diameter, septic shock, recurrent abscess, or in patients responding poorly to antibiotics for 3 days or longer. Traditionally, open perineal incision or transurethral resection was recommended as the method of choice [5,6].
Nowadays, minimally invasive treatment such as TRUS-guided needle aspiration or drainage via tube transperineally or transrectally under local anesthesia or sedation is preferred. First, Becker and Harrin [4] reported that needle aspiration with adjuvant antibiotic therapy could produce a cure, and many clinicians researched the effectiveness of needle aspiration. Collado et al. [8] reported that 20 of 24 patients treated with TRUS-guided needle aspiration and adjuvant antibiotic therapy were successfully treated. Gan [9] suggested that TRUS-needle aspiration is a feasible alternative to transurethral drainage. Lim et al. [10] reported successful treatment of prostatic abscess in 12 of 14 patients with TRUS-guided needle aspiration. Aravantinos et al reported that TRUS-guided placement of a transrectal drainage tube is a feasible, safe, and effective alternative to standard methods of treatment with good therapeutic results [3].
However, there are few reports comparing the treatment of prostate abscess according to modalities. In this study, three treatment methods of prostate abscess were reviewed and the outcomes were compared. Patients who underwent transurethral resection of the prostate had a significantly shorter hospitalization length compared with that in the other two groups, but it can't be said that transurethral resection of the prostate (TURP) is a superior method because it is an invasive procedure that requires general anesthesia and may have surgical complications. Among patients who underwent needle aspiration, 4 of 18 patients experienced recurrence within 1 month from hospital discharge. Unexpectedly, patients treated by needle aspiration had a significantly longer hospitalization stay than did those who were conservatively treated. We don't know the reason for this result. It may be that other factors need to be considered. Two patients died during conservative treatment. Although there were significant factors, these patients were relatively old, 71 and 76 years old, and it may be that more active treatment should be considered for elderly patients with prostate abscess.
This study had the limitation that it was not a controlled study and thus there may be other clinical factors affecting the clinical outcomes that were not taken into account.
Prostatic abscess is not a common disease but may result in mortality; thus, prompt diagnosis and interventional treatment is required. In this study, patients treated by TURP had a significantly shorter hospitalization length, and there were no cases of recurrence or mortality. Needle aspiration resulted in the longest hospitalization and high recurrence. Because there were limitations to this study, these results may be considered when a patient presents with prostate abscess.
Figures and Tables
TABLE 1
Demographic and clinical features of 52 patients with prostatic abscess according to treatment method

Values are presented as mean±SD (range) or number (%).
TURP, transurethral resection of the prostate; PSA, prostate-specific antigen; E. coli, Escherichia Coli; K. pneumonia, Klebsiella aerusinosa; Staphyl. aureus, Staphylococcus aureus; Strep. agalctiae, Streptochoccus agalctiae.
a:No. of comorbidies ≤1, diabetes mellitus (DM) (-) and hypertension (HTN) (-) and spinal cord injury (-); ≥2, DM (+) or HTN (+) or spinal cord injury (+), b:p<0.05 by Fisher's exact test.
References
1. Oliveira P, Andrade JA, Porto HC, Filho JE, Vinhaes AF. Diagnosis and treatment of prostatic abscess. Int Braz J Urol. 2003. 29:30–34.
2. Barozzi L, Pavlica P, Menchi I, De Matteis M, Canepari M. Prostatic abscess: diagnosis and treatment. AJR Am J Roentgenol. 1998. 170:753–757.
3. Aravantinos E, Kalogeras N, Zygoulakis N, Kakkas G, Anagnostou T, Melekos M. Ultrasound-guided transrectal placement of a drainage tube as therapeutic management of patients with prostatic abscess. J Endourol. 2008. 22:1751–1754.
4. Becker LE, Harrin WR. Prostatic abscess: a diagnostic and therapeutic approach. J Urol. 1964. 91:582–585.
5. Chitty K. Prostatic abscess. Br J Surg. 1957. 44:599–602.
6. Dajani AM, O'Flynn JD. Prostatic abscess: a report of 25 cases. Br J Urol. 1968. 40:736–739.
7. Kinahan TJ, Goldenberg SL, Ajzen SA, Cooperberg PL, English RA. Transurethral resection of prostatic abscess under sonographic guidance. Urology. 1991. 37:475–477.
8. Collado A, Palou J, Garcia-Penit J, Salvador J, de la Torre P, Vicente J. Ultrasound-guided needle aspiration in prostatic abscess. Urology. 1999. 53:548–552.
9. Gan E. Transrectal ultrasound-guided needle aspiration for prostatic abscesses: an alternative to transurethral drainage? Tech Urol. 2000. 6:178–184.
10. Lim JW, Ko YT, Lee DH, Park SJ, Oh JH, Yoon Y, et al. Treatment of prostatic abscess: value of transrectal ultrasonographically guided needle aspiration. J Ultrasound Med. 2000. 19:609–617.
11. Weinberger M, Cytron S, Servadio C, Block C, Rosenfeld JB, Pitlik SD. Prostatic abscess in the antibiotic era. Rev Infect Dis. 1988. 10:239–249.
12. Tiwari P, Pal DK, Tripathi A, Kumar S, Vijay M, Goel A, et al. Prostatic abscess: diagnosis and management in the modern antibiotic era. Saudi J Kidney Dis Transpl. 2011. 22:298–301.
13. Granados EA, Caffaratti J, Farina L, Hocsman H. Prostatic abscess drainage: clinical-sonography correlation. Urol Int. 1992. 48:358–361.
14. Bhagat SK, Kekre NS, Gopalakrishnan G, Balaji V, Mathews MS. Changing profile of prostatic abscess. Int Braz J Urol. 2008. 34:164–170.
15. Meares EM Jr. Prostatic abscess. J Urol. 1986. 136:1281–1282.
16. Trauzzi SJ, Kay CJ, Kaufman DG, Lowe FC. Management of prostatic abscess in patients with human immunodeficiency syndrome. Urology. 1994. 43:629–633.
17. Singh P, Yadav MK, Singh SK, Lal A, Khandelwal N. Case series: diffusion weighted MRI appearance in prostatic abscess. Indian J Radiol Imaging. 2011. 21:46–48.
18. Thornhill BA, Morehouse HT, Coleman P, Hoffman-Tretin JC. Prostatic abscess: CT and sonographic findings. AJR Am J Roentgenol. 1987. 148:899–900.
19. Ludwig M, Schroeder-Printzen I, Schiefer HG, Weidner W. Diagnosis and therapeutic management of 18 patients with prostatic abscess. Urology. 1999. 53:340–345.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download