Abstract
Purpose
To evaluate the impact of primary Gleason grade in Gleason score (GS) 7 prostate cancer on biochemical recurrence (BCR) after radical prostatectomy in Korean men.
Materials and Methods
We retrospectively reviewed records of 1,026 patients who underwent radical prostatectomy at Seoul National University Bundang Hospital between November 2003 and June 2009. We excluded patients who had received neoadjuvant therapy and had positive resection margins. Finally, 295 and 113 patients with GS 3+4 and GS 4+3, respectively, were included in this study. All patients were followed for at least 2 years.
Results
Of the 408 GS 7 patients, 295 (72.3%) were 3+4 and 113 (27.7%) were 4+3. Mean serum prostate specific antigen level in primary Gleason 3 was 8.99 ng/ml and primary Gleason 4 was 11.11 ng/ml. Patients with GS 4+3 were more likely to have extracapsular extension (30.1% vs. 17.6%, p<0.010) and lymphatic invasion (16.8% vs. 7.1%, p<0.005). After 2 years follow up BCR was detected in a total of 40 patients. In GS 7 with primary Gleason 3, BCR occurred in 15 (5.08%) patients while 20 (17.70%) showed BCR in GS 7 with primary Gleason 4.
Conclusions
In this study of a large, single center cohort of Korean men with GS 7 prostate cancer a noticeable difference in BCR was seen. Primary Gleason grade 4 have a higher risk of BCR compared to primary Gleason grade 3. This information may be useful when counseling patients on their prognosis and further management options.
In the United States, prostate cancer has the highest incidence and the second-highest mortality rate in men [1]. In Korea, prostate cancer is the fifth most common malignancy in men [2]. The Gleason score (GS) is an important predictor of biochemical recurrence (BCR) and disease-specific survival in men with prostate cancer after definitive treatment [3]. The GS takes into account the degree of glandular differentiation and combines the scores of the primary and secondary patterns, or grades, which indicates tumor heterogeneity. Cancers with a GS of 2 to 6 have a better prognosis than do cancers with a GS of 7 to 10 [4]. GS 7 cancers have a histologically heterogeneous pattern that comprises a different proportion of grade 3 and 4 Gleason patterns. Studies have shown that GS 7 cancers with a primary Gleason grade of 4 have significantly higher rates of seminal vesicle involvement, lymph node extension, extracapsular extension, and positive surgical margins than do GS 7 cancers with a primary Gleason grade of 3 [5].
The aim of this study was to evaluate the impact of primary Gleason grade in GS 7 prostate cancers on BCR after radical prostatectomy (RP) in Korean men from a single-center cohort.
Between November 2003 and June 2009, 1026 men underwent RP for localized prostate cancer at Seoul National University Bundang Hospital, Seongnam, Korea. All surgeries were performed by the staff of the Department of Urology. According to the final pathology report, 665 patients had a GS of 7. Of these 665 patients, 463 and 202 had a primary Gleason grade of 3 and 4, respectively. We excluded 20 patients who had received neoadjuvant therapy and 243 patients who had positive resection margins on the final pathology report. Thus, 295 and 113 patients with GS 3+4 and 4+3, respectively, were included in the analysis. All patients were followed at 1, 3, and 6 months after RP and each 6 months thereafter for at least 2 years. Preoperative serum prostate-specific antigen (PSA), body mass index (BMI), extracapsular extension (ECE), seminal vesicle invasion (SVI), lymphatic invasion, venous invasion, pathological stage, and BCR were evaluated. BCR was defined as cases in which PSA measured 0.2 ng/ml or higher two times successively after the surgery. The study was approved by the hospital Institutional Review Board.
RP specimen samples were step-sectioned at a 4-mm thickness by use of a standardized processing protocol [6]. The pathological examinations were carried out by experienced uropathologists by use of a standardized reporting protocol. The pathological assessment of each prostatectomy specimen determined whether cancer was organ-confined disease (no cancer beyond the prostatic capsule) or had ECE, SVI, or lymph node metastases [7-9].
The primary endpoint of this study was the impact of the primary Gleason pattern in GS 7 prostate cancer on BCR-free survival. The secondary endpoint was the relation between primary Gleason pattern and clinicopathological parameters.
The BCR-free survival rate was estimated with the Kaplan-Meier method and survival curves were tested with the log-rank test. The chi-square test and Student's t-test were used to analyze the association between primary Gleason grade and various clinicopathological parameters. Multivariate Cox regression analysis was used to assess the prognostic significance of certain variables, and the hazard ratio (HR) and 95% confidence intervals (CIs) were computed. A p-value<0.05 was considered statistically significant. Analyses were performed by using the PASW ver. 18.0 (IBM Co., Armonk, NY, USA).
The mean age and serum PSA of the 613 patients with GS 7 prostate cancer were 65.8 years (range, 46 to 82 years) and 9.57 ng/ml (range, 1.23 to 59.5 ng/ml), respectively. Of the 408 GS 7 patients, 295 (72.3%) were 3+4 and 113 (27.7%) were 4+3. The mean serum PSA level in GS 7 prostate cancer patients with a primary Gleason grade of 3 was 8.99 ng/ml and that in patients with a primary Gleason grade of 4 was 11.11 ng/ml. The mean follow-up period was 29.05 months. The clinicopathological findings in our cohort are shown in Table 1.
Compared with patients with GS 3+4, patients with GS 4+3 were more likely to have ECE (30.1% vs. 17.6%, p<0.010) and lymphatic invasion (16.8% vs. 7.1%, p<0.005). Meanwhile there was no significant association between primary Gleason grade and SVI (6.2% vs. 3.1%, p<0.158), perineural invasion (PNI) (66.4% vs. 60.7%, p<0.306), or microvenous invasion (1.8% vs. 0.3%, p<0.187). The mean age, PSA level, and BMI of patients with a primary Gleason grade of 4 compared with a primary Gleason grade of 3 were 66.9 years, 11.1 ng/ml, and 24.3 kg/m2 vs. 65.4 years, 8.9 ng/ml, and 24.1 kg/m2, respectively (p=0.015, p=0.019, and p=0.462, respectively). Taking into account age, PSA, BMI, primary Gleason grade, pathological stage, ECE, SVI, lymphatic invasion, and PNI in a Cox multivariate regression analysis (Table 2), serum PSA level and primary Gleason grade were independently associated with BCR-free survival. When patients with a positive resection margin were added to the multivariate analysis of BCR-free survival, the primary Gleason grade remained statistically predictive of BCR (p=0.002; HR, 2.269; 95% CI, 1.35 to 3.812).
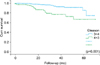
The 3-year BCR-free survival for patients with primary Gleason grades of 3 or 4 was 97.3% and 86.8%, respectively, whereas the 5-year BCR-free survival was 85.4% and 66.7%, respectively (p<0.001) (Fig. 1).
The Gleason grading of prostatic carcinoma is considered to be one of the most important predictors determining disease progression in prostate cancer. Although GS 6 cancers have lower disease progression rates than do GS 7 cancers, the heterogenic patterns within the GS 7 category mean that these cancers cannot be grouped into a unique category but instead are categorized according to the predominant Gleason grade [10,11]. Several studies have shown that GS 7 cancers with a primary Gleason grade of 4 are more aggressive and have a higher risk of BCR than do GS 7 cancers with a primary Gleason grade of 3 [12-14]. Ethnic differences have an effect on the prognosis of prostate cancer. Prostate cancers arising in Korean men exhibit poor differentiation, which adversely affects prognosis and causes a greater rate of BCR [15]. To our knowledge, this is the first study on a Korean population to assess the difference in BCR between both GS 7 groups. In this single-center study, we retrospectively analyzed 408 GS 7 patients with more than 2 years of follow-up.
In recent studies analyzing the impact of primary Gleason grade on BCR, the distribution of 3+4 vs. 4+3 ranged from 57.8% vs. 42.2% to 74.5% vs. 25.5% [8,12, 16,17]. In our study, GS 3+4 comprised 72.3% of GS 7 cancers, which is thus similar to other recent studies. Also, the difference in BCR between GS 3+4 and GS 4+3 in the present study was significant, which is also consistent with previously reported outcomes. The identification of patients with a higher risk of BCR is important for the treating urologist to plan the next mode of treatment in case of recurrence.
The importance of primary Gleason grade in GS 7 prostate cancer and the impact it has on the prognosis of prostate cancer patients has been studied by several groups [18-23], mostly with large cohorts. However, it is not possible to directly compare the outcomes of these studies because of discrepancies in the selection of various parameters used to identify the clinicopathological characteristics in each study. Moreover, the introduction of the modified International Society of Urological Pathology 2005 Gleason grading system has made this task even more difficult. In our study, we excluded 36.5% of patients who had positive resection margins on the final pathology report, which is similar to previously conducted studies [12,17]. The reason for this is that, according to several studies, even though 10 to 40% of patients undergoing RP have a positive surgical margin, only 10 to 40% of those patients develop BCR. Furthermore, although previous studies analyzed resection margin status in their data, we wanted to emphasize the prognostic factors in patients with negative resection margins, which meant those with completely resected prostate cancer.
Rasiah et al. [8] found that a primary Gleason grade of 4 was an independent predictor of disease recurrence in a multivariate analysis after adjustment for PSA, surgical margin, SVI, and ECE. In another study, Alenda et al. [12] found that primary Gleason grade 4 tumors were associated with shorter time to disease recurrence and higher 5-year disease recurrence rates than were primary Gleason grade 3 tumors and that the PSA level, positive surgical margins, SVI, and EPE were predictive factors of recurrence. In our study we also saw that primary Gleason grade was an important prognostic factor in the multivariate analysis along with PSA, although ECE and SVI were not significant predictors. This could be explained by the difference in inclusion criteria and the choice in evaluated parameters such as SVI, ECE, surgical margin status, etc.
This study had several limitations. First, as a retrospective study based on electronic medical records, it was susceptible to bias and was dependent on the integrity of the record keeping. Second, the fact that all RPs were performed by multiple surgeons could have affected the outcomes. Third, of more than 1,000 cases, we excluded 337 Gleason 7 patients who had received neoadjuvant therapy or who had positive resection margins, thus leading to a high exclusion rate.
Last, although this was a large population for a single center, BCR in the follow-up period was detected in only a small proportion of patients. Additional studies with a larger cohort and longer follow-up periods are necessary to better assess the significance of primary Gleason grade in GS 7 prostate cancers on not just BCR but also overall and cancer-specific survival.
The results of this study showed a difference in BCR in a large, single-center cohort of Korean men with GS 7 prostate cancer. Compared with a primary Gleason grade of 3, a primary Gleason grade of 4 had a higher risk of BCR. This information may be useful when counseling patients on their prognosis and further management options.
Figures and Tables
References
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009. 59:225–249.
2. Ministry of Health & Welfare. Korea Central Cancer Registry. National Cancer Center. Annual report of cancer statistics in Korea in 2009. 2011. Seoul: Ministry of Health & Welfare.
3. Eggener SE, Scardino PT, Walsh PC, Han M, Partin AW, Trock BJ, et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J Urol. 2011. 185:869–875.
4. Blute ML, Bergstralh EJ, Iocca A, Scherer B, Zincke H. Use of Gleason score, prostate specific antigen, seminal vesicle and margin status to predict biochemical failure after radical prostatectomy. J Urol. 2001. 165:119–125.
5. Epstein JI, Carmichael MJ, Partin AW, Walsh PC. Small high grade adenocarcinoma of the prostate in radical prostatectomy specimens performed for nonpalpable disease: pathogenetic and clinical implications. J Urol. 1994. 151:1587–1592.
6. Samaratunga H, Montironi R, True L, Epstein JI, Griffiths DF, Humphrey PA, et al. International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 1: specimen handling. Mod Pathol. 2011. 24:6–15.
7. Berney DM, Wheeler TM, Grignon DJ, Epstein JI, Griffiths DF, Humphrey PA, et al. International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 4: seminal vesicles and lymph nodes. Mod Pathol. 2011. 24:39–47.
8. Rasiah KK, Stricker PD, Haynes AM, Delprado W, Turner JJ, Golovsky D, et al. Prognostic significance of Gleason pattern in patients with Gleason score 7 prostate carcinoma. Cancer. 2003. 98:2560–2565.
9. Magi-Galluzzi C, Evans AJ, Delahunt B, Epstein JI, Griffiths DF, van der Kwast TH, et al. International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 3: extraprostatic extension, lymphovascular invasion and locally advanced disease. Mod Pathol. 2011. 24:26–38.
10. Tefilli MV, Gheiler EL, Tiguert R, Sakr W, Grignon DJ, Banerjee M, et al. Should Gleason score 7 prostate cancer be considered a unique grade category? Urology. 1999. 53:372–377.
11. Sakr WA, Tefilli MV, Grignon DJ, Banerjee M, Dey J, Gheiler EL, et al. Gleason score 7 prostate cancer: a heterogeneous entity? Correlation with pathologic parameters and disease-free survival. Urology. 2000. 56:730–734.
12. Alenda O, Ploussard G, Mouracade P, Xylinas E, de la Taille A, Allory Y, et al. Impact of the primary Gleason pattern on biochemical recurrence-free survival after radical prostatectomy: a single-center cohort of 1,248 patients with Gleason 7 tumors. World J Urol. 2011. 29:671–676.
13. Wright JL, Salinas CA, Lin DW, Kolb S, Koopmeiners J, Feng Z, et al. Prostate cancer specific mortality and Gleason 7 disease differences in prostate cancer outcomes between cases with Gleason 4+3 and Gleason 3+4 tumors in a population based cohort. J Urol. 2009. 182:2702–2707.
14. Yu JH, Cho MC, Chang IH, Han JH, Han BK, Jeong SJ, et al. Comparative analysis of the clinicopathological characteristics of patients with prostate cancer with a pathological Gleason score 3+4 versus Gleason score 4+3. Korean J Urol. 2007. 48:804–808.
15. Song C, Ro JY, Lee MS, Hong SJ, Chung BH, Choi HY, et al. Prostate cancer in Korean men exhibits poor differentiation and is adversely related to prognosis after radical prostatectomy. Urology. 2006. 68:820–824.
16. Khoddami SM, Shariat SF, Lotan Y, Saboorian H, McConnell JD, Sagalowsky AI, et al. Predictive value of primary Gleason pattern 4 in patients with Gleason score 7 tumours treated with radical prostatectomy. BJU Int. 2004. 94:42–46.
17. Miyake H, Muramaki M, Furukawa J, Tanaka H, Inoue TA, Fujisawa M. Prognostic significance of primary Gleason pattern in Japanese men with Gleason score 7 prostate cancer treated with radical prostatectomy. Urol Oncol. 2012. 05. 30. [Epub]. http://dx.doi.org/10.1016/j.urolonc.2012.05.001.
18. Chan TY, Partin AW, Walsh PC, Epstein JI. Prognostic significance of Gleason score 3+4 versus Gleason score 4+3 tumor at radical prostatectomy. Urology. 2000. 56:823–827.
19. Herman CM, Kattan MW, Ohori M, Scardino PT, Wheeler TM. Primary Gleason pattern as a predictor of disease progression in gleason score 7 prostate cancer: a multivariate analysis of 823 men treated with radical prostatectomy. Am J Surg Pathol. 2001. 25:657–660.
20. Han M, Partin AW, Zahurak M, Piantadosi S, Epstein JI, Walsh PC. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol. 2003. 169:517–523.
21. Tolonen TT, Kujala PM, Tammela TL, Tuominen VJ, Isola JJ, Visakorpi T. Overall and worst gleason scores are equally good predictors of prostate cancer progression. BMC Urol. 2011. 11:21.
22. Stark JR, Perner S, Stampfer MJ, Sinnott JA, Finn S, Eisenstein AS, et al. Gleason score and lethal prostate cancer: does 3+4=4+3? J Clin Oncol. 2009. 27:3459–3464.
23. Cao D, Kibel AS, Gao F, Tao Y, Humphrey PA. The Gleason score of tumor at the margin in radical prostatectomy is predictive of biochemical recurrence. Am J Surg Pathol. 2010. 34:994–1001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download