Abstract
Purpose
Several recent studies have reported the benefits of tubeless percutaneous nephrolithotomy (PNL). Postoperatively, tubeless PNL patients have an indwelling ureteral stent placed, which is often associated with stent-related morbidity. We have performed totally tubeless (tubeless and stentless) PNL in which no nephrostomy tube or ureteral stent is placed postoperatively. We evaluated the safety, effectiveness, and feasibility of totally tubeless PNL.
Materials and Methods
From March 2008 to February 2012, 57 selected patients underwent standard or totally tubeless PNL. Neither a nephrostomy tube nor a ureteral stent was placed in the totally tubeless PNL group. We compared patient and stone characteristics, operation time, length of hospitalization, analgesia requirements, stone-free rate, blood loss, change in creatinine, and perioperative complications between the standard and totally tubeless PNL groups.
Results
There were no significant differences in preoperative patient characteristics, postoperative complications, or the stone-free rate between the two groups, but the totally tubeless PNL group showed a shorter hospitalization and a lesser analgesic requirement compared with the standard PNL group. Blood loss and change in creatinine were not significantly different between the two groups.
Percutaneous nephrolithotomy (PNL) is a minimally invasive surgical modality for the management of most renal stones. Technological advancements and refinements have contributed to further lowering the morbidity associated with this procedure. Such refinements include the use of a smaller working sheath and nephroscope (mini PNL) [1], sealing of the percutaneous access tract with hemostatic agents [2-4], substituting general anesthesia with regional blocks (ambulatory spinal tubeless PNL) [5], and avoidance of a nephrostomy tube (tubeless PNL) [6].
Tubeless PNL has been known to be comparable to standard PNL in hemorrhagic and postoperative complications. Tubeless PNL has already been reported in Korea and has produced satisfactory results [7]. This modification in technique allows earlier discharge from the hospital, reduction in postoperative pain, and more rapid recovery.
In most tubeless PNL procedures, internal drainage is provided with a double-J stent or temporary ureteral catheter. In those cases, patients must undergo the uncomfortable procedure for removal of the stent. However, in totally tubeless PNL, internal drainage is not provided. In the published data, there are few studies that include totally tubeless PNL [8-10], and to our knowledge, there are no published studies associated with totally tubeless PNL in Korea.
We have performed totally tubeless PNL without inserting ureteral stents in some patients since 2008. The results have shown that totally tubeless PNL does not differ from standard PNL in terms of complications and, moreover, that it is superior in terms of hospitalization and postoperative pain [8,11-14]. This study aimed to compare the totally tubeless and standard PNL procedures as well as to identify cases appropriate for totally tubeless PNL.
At this hospital, 65 patients were diagnosed with renal stones, with or without ureter stones, between March 2008 and February 2012. This study was conducted on 57 patients, with the exception of 8 patients. Exclusions were made for 8 cases for the following reasons: serious hemorrhage occurring during surgery, the need to perform secondary PNL owing to a large burden of remnant stones, and undergoing percutaneous multiple tracts [15,16]. Standard PNL and totally tubeless PNL were performed on 30 and 27 patients, respectively. At first, standard PNL or totally tubeless PNL was performed according to our preference, but the former has not been performed since May 2011.
First of all, the percutaneous tract was acquired by the insertion of a guidewire to the affected kidney preoperatively in all cases, and the surgery was performed under general anesthesia. With the patient in the lithotomy position, the 6-Fr UPJ occlusion balloon catheter (Cook Medical, Bloomington, IL, USA) was inserted retrogradely, and hydronephrosis was induced by a balloon occlusion at the ureteropelvic junction. Following the placement of a 16-Fr Foley catheter, the patient was turned to the prone position, and the percutaneous tract was dilated by using the UltraxxTM nephrostomy balloon (UNB-10-15, Cook Medical). Then, the tract was secured by the placement of a 28-Fr Amplatz sheath, and the surgery was performed with a 26-Fr rigid nephroscope (Karl Storz, Tuttlingen, Germany). The calculus was crushed and removed with the use of a pneumatic lithoclast (Karl Storz) or an ultrasonic lithotriptor (Karl Storz).
After completing the surgery, a 20-Fr Malecot catheter was placed in cases of standard PNL. The Malecot catheter was kept for 3 to 5 days postoperatively until the hematuria recovered. In the case of totally tubeless PNL, nephrostomy and ureteral stents were not placed. The surgical site was sutured after being compressed for about 10 minutes, and the patient was released from the hospital after hematuria took a favorable turn. Patients who complained of pain after surgery were given intramuscular injections of tramadol HCL (50 mg). Multiple renal stones were defined as the detection of at least two calculi, and a febrile urinary tract infection, one of the postoperative complications, as a rise in body temperature to 38 degrees Celsius.
A comparison was made between the two groups in clinical values, such as patients' characteristics, stone characteristics, operation time, transfusion rate, blood loss, changes in serum creatinine levels, length of hospitalization, analgesia requirements, stone-free rate, perioperative complications, and auxiliary treatment. Stone volume was calculated by using the formula of a sphere, with the mean radius of a major axis and a minor axis (stone volume=4/3π [major axis+minor axis/4]3) [17]. Blood loss was calculated by using the formula of active blood loss [18]. The stone-free rate was defined as all cases in which the stone disappeared on the computed tomography or simple X-ray after PNL. Statistical analyses were conducted by using PASW ver. 18.0 (IBM Co., Armonk, NY, USA). Mann-Whitney U test and the Fisher's exact test were used as appropriate. p-values of less than 0.05 were considered significant.
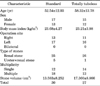
A total of 57 patients undergoing PNL for renal stones, with or without ureter stones, completed the study protocol: 30 patients in the standard group and 27 patients in the totally tubeless group. There were no significant statistical differences in patient age, gender distribution, body mass index, stone size, or stone laterality (Table 1).
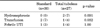
The stone-free rates were 73.3% and 77.8% in the standard group and totally tubeless group, respectively, with no significant statistical difference. The mean operation time was slightly longer in the standard group (148.5 minutes) than in the totally tubeless group (128.7 minutes), but there was no statistically significant difference. There was no significant difference between the two groups with regard to serum creatinine change or blood loss. However, the length of hospitalization in the totally tubeless group was significantly shorter than in the standard group, and analgesic requirements favored the totally tubeless group with statistical significance (Table 2).
There were no adjacent organ injuries during the operation in the two groups, and the postoperative complication rates were similar. The transfusion rates were 7% (2/30) and 4% (1/27) in the standard and totally tubeless groups, respectively, with no significant statistical difference. Postoperative hydronephrosis was 0% (0/30) and 7% (2/27) in the standard and totally tubeless groups, respectively, with no significant statistical difference (Table 3).
There were 14 cases with remnant stones managed by extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic stone removal (URS). There were 2 cases of postoperative hydronephrosis in the totally tubeless PNL group, and both of them had residual stones. There was no hydronephrosis after URS or retrograde ureteral stent insertion.
One patient (3%) in the standard PNL group underwent selective renal angioembolization because of pseudoaneurysm.
PNL has been accepted as a standard procedure for the management of large renal stones [19-22]. Traditionally, nephrostomy tube drainage after PNL has been advocated for several reasons [13]. It provides reliable urinary drainage, it provides hemostatic tamponade to the fresh percutaneous renal tract, and it provides continuous access to the renal collecting system should a secondary percutaneous procedure be required. Despite these obvious and important advantages, however, nephrostomy tubes, especially in the vicinity of a rib, are thought to contribute to postoperative pain and morbidity. Kader et al. [23] reported that hospitalization could be curtailed and the use of analgesics could be reduced by applying a small-diameter nephrostomy tube (PNT) after PNL and that such a tube was not different from large-diameter ones in terms of changes in the hemoglobin level. On the basis of this study, many researchers have insisted on the uselessness of PNT, since Wickham et al. [12] reported the first result of tubeless PNL in 1984. Thereafter, Bellman et al. [6] challenged the necessity of placing a nephrostomy tube after a PNL procedure in 50 patients. In that study, the nephrostomy tube was replaced with a double-J stent. The hospitalization time, analgesia requirements, time to return to normal activities, and cost were significantly lower with this technique. The authors concluded that tubeless PNL is a safe procedure that offers numerous advantages over the routine placement of a nephrostomy tube. After this report, tubeless PNL became popular in many centers.
In Korea, Kwon and Kim [7] compared perioperative outcomes between standard PNLs and tubeless PNLs with ureteral stents in 2007 and reported that the latter was more effective for curtailing hospitalization. Karami and Gholamrezaie [13] compared 30 totally tubeless patients with 30 standard PNL patients and reported that avoiding PNT and removing the ureteral catheter at the end of the procedure in selected patients was safe and was associated with a significantly decreased length of hospitalization and analgesic requirements. Likewise, Bdesha et al. [24] reported that hospitalization was curtailed in 40 patients on whom PNT placements were not performed. Crook randomly performed standard PNL and totally tubeless PNL on 50 patients with renal stones and reported that there were no significant intergroup differences in hemorrhage, infection, blood transfusion, or clinical values, but that the hospitalization time was shorter in the totally tubeless PNL group than in the standard PNL group [14].
In our study, 73.3% of patients in the standard PNL group and 77.8% of patients in the totally tubeless group were stone-free. We managed residual calculi patients with ESWL or URS. Perioperative blood loss, transfusion, and the complication rate in the totally tubeless group were also comparable to the standard PNL group. Meanwhile, the length of hospitalization and analgesic requirements were significantly decreased in the totally tubeless group. Moreover, the procedure for removal of the stent should not be necessary in the totally tubeless group as opposed to the tubeless with internal stent drainage patients. Totally tubeless PNL reduced the additional postoperative cost and discomfort associated with removal of the stent.
The possible limitation of the tubeless procedure is that it precludes secondary procedures for the treatment of residual stones. However, alternatively, residual calculi can be safely managed by ESWL or retrograde intrarenal surgery by use of flexible ureteroscopy. We managed 12 cases of residual calculi with ESWL, and the other two patients were managed by URS. The most common complications of PNL are bleeding and urinary extravasation. Nephrostomy tube placement, at the end of the standard PNL procedure, is thought to prevent these complications. A concern of many urologists with the tubeless technique is the lack of a tamponade effect in the nephrostomy tract. Despite this, tubeless PNL retains its role in selected patients with renal stones who are undergoing uncomplicated PNL. However, a nephrostomy tube should be placed if serious disruption or significant laceration of the collecting system is noted. Also, if significant intrarenal bleeding is found and endoscopic visualization is impossible, a nephrostomy tube should be inserted. The tube is then clamped, allowing the pelvicaliceal system to be tamponaded.
With the intent of reducing postoperative discomfort and pain, hospital stay, and cost, the totally tubeless PNL procedure has gained popularity in recent years. Appropriate patients should be selected for totally tubeless PNL. We believe that this procedure will be acceptable only when safety has not been sacrificed. We believe that uncomplicated percutaneous nephrolithotripsy can be performed without leaving a nephrostomy tube or ureteral stent. We also believe that the major advantage for patients undergoing totally tubeless PNL is the absence of stent-related flank pain and dysuria.
The results of the present study showed that totally tubeless PNL did not differ greatly from standard PNL in the consideration of effectiveness and safety and that it curtailed length of hospitalization and reduced the analgesia requirement. Although prospective and larger-scale studies may be needed to confirm the result of this study, totally tubeless PNL may be an alternative for the management of renal stones in selected patients.
References
1. Feng MI, Tamaddon K, Mikhail A, Kaptein JS, Bellman GC. Prospective randomized study of various techniques of percutaneous nephrolithotomy. Urology. 2001. 58:345–350.
2. Shah HN, Kausik V, Hedge S, Shah JN, Bansal MB. Initial experience with hemostatic fibrin glue as adjuvant during tubeless percutaneous nephrolithotomy. J Endourol. 2006. 20:194–198.
3. Schick V. Sealing of percutaneous nephrolithotomy access after complete stone removal with a hemostyptic gelatin powder (Spongostan). Aktuelle Urol. 2006. 37:52–57.
4. Yu DS. Gelatin packing of intracortical tract after percutaneous nephrostomy lithotripsy for decreasing bleeding and urine leakage. J Chin Med Assoc. 2006. 69:162–165.
5. Singh I, Kumar A, Kumar P. "Ambulatory PCNL" (tubeless PCNL under regional anesthesia) -- a preliminary report of 10 cases. Int Urol Nephrol. 2005. 37:35–37.
6. Bellman GC, Davidoff R, Candela J, Gerspach J, Kurtz S, Stout L. Tubeless percutaneous renal surgery. J Urol. 1997. 157:1578–1582.
7. Kwon S, Kim HG. A comparative study between standard and tubeless percutaneous nephrolithotomy. Korean J Urol. 2007. 48:45–48.
8. Crook TJ, Lockyer CR, Keoghane SR, Walmsley BH. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2008. 22:267–271.
9. Aghamir SM, Hosseini SR, Gooran S. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2004. 18:647–648.
10. Aghamir SM, Mohammadi A, Mosavibahar SH, Meysamie AP. Totally tubeless percutaneous nephrolithotomy in renal anomalies. J Endourol. 2008. 22:2131–2134.
11. Istanbulluoglu OM, Ozturk B, Cicek T, Gonen M, Ozkardes H. Case report: bilateral simultaneous tubeless and stentless percutaneous nephrolithotomy. J Endourol. 2008. 22:25–28.
12. Wickham JE, Miller RA, Kellett MJ, Payne SR. Percutaneous nephrolithotomy: one stage or two? Br J Urol. 1984. 56:582–585.
13. Karami H, Gholamrezaie HR. Totally tubeless percutaneous nephrolithotomy in selected patients. J Endourol. 2004. 18:475–476.
14. Crook TJ, Lockyer CR, Keoghane SR, Walmsley BH. A randomized controlled trial of nephrostomy placement versus tubeless percutaneous nephrolithotomy. J Urol. 2008. 180:612–614.
15. Zilberman DE, Lipkin ME, de la Rosette JJ, Ferrandino MN, Mamoulakis C, Laguna MP, et al. Tubeless percutaneous nephrolithotomy: the new standard of care? J Urol. 2010. 184:1261–1266.
16. Istanbulluoglu MO, Cicek T, Ozturk B, Gonen M, Ozkardes H. Percutaneous nephrolithotomy: nephrostomy or tubeless or totally tubeless? Urology. 2010. 75:1043–1046.
17. Pryor JL, Jenkins AD. Use of double-pigtail stents in extracorporeal shock wave lithotripsy. J Urol. 1990. 143:475–478.
18. McCullough TC, Roth JV, Ginsberg PC, Harkaway RC. Estimated blood loss underestimates calculated blood loss during radical retropubic prostatectomy. Urol Int. 2004. 72:13–16.
19. Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, Gallucci M, et al. Guidelines on urolithiasis. Eur Urol. 2001. 40:362–371.
20. Stables DP, Ginsberg NJ, Johnson ML. Percutaneous nephrostomy: a series and review of the literature. AJR Am J Roentgenol. 1978. 130:75–82.
21. Alken P, Hutschenreiter G, Gunther R, Marberger M. Percutaneous stone manipulation. J Urol. 1981. 125:463–466.
22. Joseph WS. Percutaneous nephrolithotomy: technique, indication and complication. AUA Update Ser. 1993. 12:154–159.
23. Kader AK, Finelli A, Honey RJ. Nephroureterostomy-drained percutaneous nephrolithotomy: modification combining safety with decreased morbidity. J Endourol. 2004. 18:29–32.
24. Bdesha AS, Jones CR, North EA, Pinfield J, Boyd PJ. Routine placement of nephrostomy tube is not nessary after pertutaneous nephrolithotomy. Br J Urol. 1997. 79:Suppl 4. 1.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download