Abstract
Purpose
To evaluate the direct anti-cancer effect of a single instillation of epirubicin (SIE) after transurethral resection of bladder tumor (TURBT) for non-muscle-invasive bladder cancer (NMIBC) by analysis of immediate urine cytology (IUC).
Materials and Methods
We reviewed the records of 158 patients who had IUC after TURBT for NMIBC. Fifty-six patients were treated with SIE after TURBT and 102 patients were not treated with SIE. The direct anti-cancer effect of SIE was compared in the two groups according to the result of IUC. The relationship between SIE and IUC in NMIBC was analyzed by use of multivariate Cox proportional hazards regression models.
Results
The IUC-positive rate was 33.9% in the SIE group and 42.1% in the non-SIE group (p=0.005). The IUC-positive rate was lower in the SIE group than in the non-SIE group for each factor, including tumor stage, tumor grade, tumor size, tumor multiplicity, and preoperative urine cytology. Multivariate Cox proportional hazards regression analysis revealed that SIE was significantly associated with a negative IUC result in patients with NMIBC (HR, 0.163) (p<0.001).
Bladder cancer is the most common urological malignancy in Korea [1,2]. Transurethral resection of bladder tumor (TURBT) is commonly performed for the diagnosis and initial therapy of bladder cancer [3]. Although non-muscle-invasive bladder cancer (NMIBC) can be treated with transurethral resection of bladder tumor (TURBT), the high frequency of intravesical recurrence is a serious concern. It was reported that intravesical recurrence occurred in 50 to 70% of patients within 5 years after TURBT for NMIBC and that the risk of progression to invasive cancer was 5 to 20% [4]. A common belief is that freely floating tumor cells adhere to the bladder mucosa during TURBT, resulting in the formation of new tumors that are detected at follow-up. Popeert et al. [5] noted that a single instillation of epirubicin (SIE) into the bladder had a significant effect on marker lesions with acceptable toxicity. A number of randomized studies have shown that a single instillation of a cytotoxic drug, mainly epirubicin or mitomycin, decreases the number of subsequent recurrences [6-8].
Knowledge is lacking, however, about the direct anti-cancer effect of the single instillation concept. Thus, we assessed the direct anti-cancer effect of SIE after TURBT for NMIBC by analyzing the results of immediate urine cytology (IUC).
We reviewed the records of 158 patients who had IUC after TURBT for NMIBC from October 2003 to January 2011, excluding patients who had muscle-invasive bladder cancer, metastatic bladder cancer, or combined urinary upper tract tumor and carcinoma in situ (CIS) confirmed by permanent biopsy. Among 158 patients, 56 patients were treated with SIE after TURBT and 102 patients were not treated with SIE. Patients received 50 mg epirubicin in 50 ml saline solution, which was instilled within 6 hours after TURBT. The catheter was clamped for 1 hour. Patients also received bladder irrigation twice a day during the postoperative days. The Foley catheter was removed when the gross hematuria had resolved after TURBT. Before Foley catheter removal, washed urine for IUC was obtained by bladder irrigation with 0.9% normal saline solution. IUC was evaluated by a pathologist in accordance with the 1999 World Health Organization (WHO) classification. The cytology was categorized as positive if cancer cells or cells with atypical changes suggesting malignancy were found, and it was regarded as negative in cases with mild to moderate atypical changes.
Tumors were staged according to the 2002 American Joint Committee on Cancer staging system. Tumors were graded according to the 2004 WHO/International Society of Urologic Pathology (WHO/ISUP) classification of urothelial neoplasia. Tumor size was classified as either less than 3 cm tumor diameter or 3 cm or larger tumor diameter. Tumor multiplicity was classified into 1 and 2-3 lesions and more than 3 lesions.
The direct anti-cancer effect of SIE was compared in the two groups according to IUC. Comparison of the patients' baseline characteristics between the SIE group and the non-SIE group was performed by chi-square test. Chi-square tests were also performed to measure the association between IUC and SIE with 5 variables, including tumor stage, tumor grade, tumor size, tumor multiplicity, and preoperative urine cytology. The IUC-positive rate of the SIE and non-SIE groups was compared by chi-square tests. The relationship between SIE and IUC in NMIBC was studied by use of multivariate Cox proportional hazards regression models. Statistical analysis was performed by use of SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA), and p<0.05 were considered statistically significant.
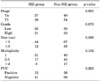
The median (range) age of the patients was 63 (range, 35 to 88) years. The median follow-up period was 21 (range, 3 to 77) months. Table 1 shows the tumor stage, tumor grade, tumor size, tumor multiplicity, and preoperative urine cytology of the SIE group and the non-SIE group. There were no significant differences in tumor stage, tumor grade, tumor size, tumor multiplicity, or preoperative urine cytology between the two groups.
In the total patients, 62 patients (39.3%) had a positive IUC result and 96 patients (60.7%) had a negative IUC result. Table 2 shows the relationship between a positive IUC result and SIE for the 5 variables. In the positive IUC group, tumor stage was higher than in the negative IUC group (p=0.042). Also, tumor grade was higher (p<0.001) and more tumor lesions were present in the positive IUC group (p=0.001). Tumor size was larger in the positive IUC group and there was a significant difference between the two groups (p=0.033). In the positive IUC group, more preoperative urine cytology was positive than in the negative IUC group, and the difference between groups was significant (p=0.018). In the negative IUC group, SIE treatment was greater than in the positive IUC group, and this difference was significant (p<0.001).
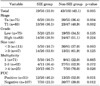
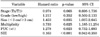
The IUC positive rate was 33.9% in the SIE group and 42.1% in the non-SIE group (p=0.005). In the SIE group, the IUC positive rate was lower for each factor, including tumor stage, tumor grade, tumor size, tumor multiplicity, and preoperative urine cytology (Table 3). Multivariate Cox proportional hazards regression analysis revealed that tumor size (HR, 1.453; p=0.035), tumor multiplicity (HR, 3.733; p=0.025), and preoperative urine cytology (HR, 1.278; p=0.023) were significantly associated with IUC in the patients with NMIBC (Table 4). Also, SIE was significantly associated with IUC in the patients with NMIBC (HR, 0.163; p<0.001) (Table 4). We can therefore recognize a direct anti-cancer effect of SIE in the patients who underwent TURBT for NMIBC.
Epirubicin, a derivative of doxorubicin, is an anthracycline antibiotic that undergoes minimal trans-urothelial absorption [9]. It was reported that epirubicin has anti-tumor efficacy that decreases the recurrence rate when used an intravesical chemotherapeutic agent after TURBT for superficial bladder cancer [10,11]. In a large controlled study performed by the European Organization for the Research and Treatment of Cancer, Oosterlinck et al. [8] reported that a single instillation of 80 mg epirubicin given immediately (within 6 hours) after TURBT decreased the recurrence rate by nearly 50% compared with the water-instilled group. Epirubicin is a chemotherapeutic drug that has a favorable tolerability profile and has been shown to prevent recurrences in patients with low- and intermediate-risk NMIBC [12,13]. Therefore, we used epirubicin as a primary agent. We used a dose of 50 mg epirubicin based on the successful results of Ali-el-Dein et al. [10], but better results may be achieved with a dose of 80 mg epirubicin. We are going to adjust the titration of epirubicin.
There are many reports regarding the timing and duration of instillation therapy, including epirubicin [14,15]. Instillation of epirubicin immediately after TURBT for superficial bladder cancer significantly decreased disease recurrence compared with instillation of water [15]. It was reported that one of the mechanisms of intravesical recurrence after TURBT of bladder cancer is implantation of tumor cells in the bladder wall, and instillation immediately after TURBT seems to be effective in preventing free tumor cells from implanting in the bladder wall during or after TURBT [16]. However, no research has studied the direct effect of SIE.
The initial diagnosis and follow-up of previous bladder cancer are commonly based on urine cytology and cystoscopy. The sensitivity value of urinary cytology for detecting bladder cancer reported in various series ranges from 16 to 60% [17]. Budman et al. [18] reported that urine cytology has 12.1 to 84.6% sensitivity and 78.0 to 100% specificity [13]. The high specificity is the most important feature of cytology, because a positive reading regardless of cystoscopic or radiographic findings suggests the existence of malignancy in the vast majority of patients [18]. IUC has the same pathological property as usual follow-up urine cytology, although IUC can predict cancer recurrence immediately [19]. Also, IUC is an easy and noninvasive examination method for detecting recurrence of NMIBC.
Several studies have suggested risk tables for recurrence and progression of NMIBC, such as number of tumors, tumor size, prior recurrence rate, T category, and presence of CIS [20]. However, these cannot sufficiently reflect the probability of recurrence. Situations such as tumor implantation after TURBT, invisible tumor during TURBT, and incomplete TURBT can be a reason for cancer recurrence. In our study, tumor stage, tumor grade, tumor size, tumor multiplicity, and preoperative urine cytology also had a significant relationship with positive IUC.
There are some reasons for cancer recurrence after TURBT. Tumor implantation can be an important reason. The concept that tumor cells implant on the altered urothelial surface, such as after endoscopic resection, has been demonstrated in animal models [10]. The fact that early postoperative chemotherapy reduces the recurrence rates strongly suggests that implantation of liberated tumor cells is one of the mechanisms responsible for recurrence [10]. In our study, we were focused on tumor implantation as the reason for recurrence. The IUC positive rate was lower in the SIE group. Also, SIE was significantly associated with IUC in the patients with NMIBC. This result means that SIE has an effect of preventing free tumor cells from implanting in the bladder wall after TURBT.
Our analysis is limited in that we were unable to evaluate cancer recurrence. In addition, studies with standardized protocols for evaluating cancer recurrence after TURBT for NMIBC in the SIE group and non-SIE group are needed to verify our findings.
Figures and Tables
References
1. Seo HS, Lee NK, Jee SH. The effect of cigarette smoaking on bladder cancer in Korean: a prospective cohort study. Korean J Urol. 2005. 46:234–240.
2. Kim WJ, Chung JI, Hong JH, Kim CS, Jung SI, Yoon DK. Epidemiological study for urologic cancer in Korea (1998-2002). Korean J Urol. 2004. 45:1081–1088.
3. Yang SJ, Song PH, Kim HT. Comparison of deep biopsy tissue damage from transurethral resection of bladder tumors between bipolar and monopolar devices. Korean J Urol. 2011. 52:379–383.
4. Jone JS, Campbell SC. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Non-muscle-invasive bladder cancer (Ta, T1, and CIS). Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;2447–2467.
5. Popert RJ, Goodall J, Coptcoat MJ, Thompson PM, Parmar MK, Masters JR. Superficial bladder cancer: the response of a marker tumour to a single intravesical instillation of epirubicin. Br J Urol. 1994. 74:195–199.
6. Abrams PH, Choa RG, Gaches CG, Ashken MH, Green NA. A controlled trial of single dose intravesical Adriamycin in superficial bladder tumours. Br J Urol. 1981. 53:585–587.
7. Zincke H, Utz DC, Taylor WF, Myers RP, Leary FJ. Influence of thiotepa and doxorubicin instillation at time of transurethral surgical treatment of bladder cancer on tumor recurrence: a prospective, randomized, double-blind, controlled trial. J Urol. 1983. 129:505–509.
8. Oosterlinck W, Kurth KH, Schröder F, Bultinck J, Hammond B, Sylvester R. A prospective European Organization for Research and Treatment of Cancer Genitourinary Group randomized trial comparing transurethral resection followed by a single intravesical instillation of epirubicin or water in single stage Ta, T1 papillary carcinoma of the bladder. J Urol. 1993. 149:749–752.
9. Cersosimo RJ, Hong WK. Epirubicin: a review of the pharmacology, clinical activity, and adverse effects of an adriamycin analogue. J Clin Oncol. 1986. 4:425–439.
10. Ali-el-Dein B, Nabeeh A, el-Baz M, Shamaa S, Ashamallah A. Single-dose versus multiple instillations of epirubicin as prophylaxis for recurrence after transurethral resection of pTa and pT1 transitional-cell bladder tumours: a prospective, randomized controlled study. Br J Urol. 1997. 79:731–735.
11. Melekos MD, Dauaher H, Fokaefs E, Barbalias G. Intravesical instillations of 4-epi-doxorubicin (epirubicin) in the prophylactic treatment of superficial bladder cancer: results of a controlled prospective study. J Urol. 1992. 147:371–375.
12. Rajala P, Kaasinen E, Raitanen M, Liukkonen T, Rintala E. Finnbladder Group. Perioperative single dose instillation of epirubicin or interferon-alpha after transurethral resection for the prophylaxis of primary superficial bladder cancer recurrence: a prospective randomized multicenter study? FinnBladder III long-term results. J Urol. 2002. 168:981–985.
13. Berrum-Svennung I, Granfors T, Jahnson S, Boman H, Holmäng S. A single instillation of epirubicin after transurethral resection of bladder tumors prevents only small recurrences. J Urol. 2008. 179:101–105.
14. Okamura K, Kinukawa T, Tsumura Y, Otani T, Itoh H, Kobayashi H, et al. A randomized study of short-versus long-term intravesical epirubicin instillation for superficial bladder cancer. Nagoya University Urological Oncology Group. Eur Urol. 1998. 33:285–288.
15. Nomata K, Noguchi M, Kanetake H, Tsuda N, Hayashi M, Yamashita S, et al. Intravesical adjuvant chemotherapy for superficial transitional cell bladder carcinoma: results of a randomized trial with epirubicin comparing short-term versus long-term maintenance treatment. Cancer Chemother Pharmacol. 2002. 50:266–270.
16. Akaza H. New strategy of bio-chemoprevention on recurrence of superficial bladder cancer based on a hypothesis of the mechanism of recurrence. Gan To Kagaku Ryoho. 1997. 24:Suppl 1. 253–256.
17. Lokeshwar VB, Soloway MS. Current bladder tumor tests: does their projected utility fulfill clinical necessity? J Urol. 2001. 165:1067–1077.
18. Budman LI, Kassouf W, Steinberg JR. Biomarkers for detection and surveillance of bladder cancer. Can Urol Assoc J. 2008. 2:212–221.
19. Shin YS, Kim SD, Cha JS, Kim MK, Jeong YB, Kim HJ. Clinical significance of immediate urine cytology after transurethral resection of bladder tumor in patients with non-muscle invasive bladder cancer. Int J Urol. 2011. 18:439–443.
20. Kiemeney LA, Witjes JA, Heijbroek RP, Verbeek AL, Debruyne FM. Predictability of recurrent and progressive disease in individual patients with primary superficial bladder cancer. J Urol. 1993. 150:60–64.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download