Abstract
Purpose
Metabolic syndrome (MS) plays a potential role in the etiology of benign prostatic hyperplasia (BPH). Recent studies have reported on an association between MS and BPH. However, there has been no consensus on recent results. This study was conducted to evaluate the associations among prostate-specific antigen (PSA), prostate volume (PV), and metabolic components in men who visited our health promotion center.
Materials and Methods
During the period from January 2005 to December 2010, 521 consecutive men (age range, 40 to 70 years) who underwent transrectal ultrasonography were enrolled in this retrospective study. The health screening program includes blood pressure, body measurements (height, weight, waist circumference, body mass index), biochemical analysis (serum glucose, total cholesterol, triglycerides, high-density and low-density lipoprotein cholesterol, fasting plasma glucose, tumor markers), stool and urine analysis, and a detailed clinical examination.
Results
The serum PSA level and PV were significantly higher in patients with MS than in patients without MS, retrospectively (p<0.001, p<0.001). Patients with more than one metabolic component were significantly more likely to have a larger PV and higher serum PSA level. The serum PSA level and PV were increased in a similar manner with the increasing sum of MS components (p<0.0001, p<0.0001).
Benign prostatic hyperplasia (BPH) is among the most common ailments in older men [1]. The prevalence of pathological BPH is only 8% in the fourth decade of life; however, 50% of the male population in the age range of 51 to 60 years is diagnosed with pathological BPH [1]. This prevalence increases to 90% in men older than 80 years [2]. BPH is a specific histopathologic entity characterized by the presence of nonmalignant, unregulated hyperplasia of the stromal and epithelial cells [3]. Clinically, BPH may be associated with obstructive and irritative lower urinary tract symptoms (LUTS) secondary to the prostate enlargement and is associated with complications such as acute urinary retention, bladder stones, gross hematuria, and urinary tract infections [3]. Although BPH is a highly prevalent disease, the cellular mechanism of BPH involving the stromal and epithelial components of the prostate is not well understood [4,5]. For over a century, there have been two known etiologic factors for the pathogenesis of BPH: aging and testicular androgens [5]. In addition, family history, race/ethnicity, cigarette smoking, hypertension, non-insulin-dependent diabetes mellitus (NIDDM), high insulin content, and central obesity have been reported to be risk factors for the development of BPH [6,7].
Metabolic syndrome (MS) is a combination of several metabolic and physiological abnormalities in the individual, including increased waist circumference (WC), high blood pressure, fasting plasma glucose (FPG), low high-density lipoprotein cholesterol (HDL-C), and dyslipidemia. Furthermore, MS is associated with high morbidity and mortality [8,9]. Many reports have discussed the finding that diabetic and obese men have larger prostate glands than do men without these conditions [7-10]. Also, recent reports have suggested an association between MS components and LUTS related to BPH [11]. However, MS as a risk factor for BPH has been under debate despite the epidemiologic and pathophysiologic evidence.
Therefore, this study was conducted to evaluate the effect of MS components on the serum PSA level and prostate volume (PV) in healthy men aged 40 to 70 years.
From January 2005 to December 2010, 521 consecutive men (age range, 40 to 70 years) who underwent transrectal ultrasonography (TRUS) were enrolled in the study. The health screening data included blood pressure, body measurements (height, weight, WC, body mass index [BMI]), biochemical analysis (complete blood cell count, serum glucose, total cholesterol, triglycerides (TG), HDL-C and low-density lipoprotein cholesterol [LDL-C], FPG, serologic test, coagulation test, and tumor markers), stool and urine analysis, chest radiography, electrocardiography, and detailed clinical examination. All subjects were asked to complete a questionnaire designed to assess their detail medical history, particularly of systemic diseases such as diabetes mellitus (DM) and hypertension. Among the 521 men, 101 men were excluded from this study owing to current medical treatment for BPH, having a history of DM or cardiovascular disease, having a diagnosis of prostate cancer and previous prostate or urethral surgery, or having abnormal serum PSA (≥4 ng/ml, n=15). In addition, patients with pyuria and bacteriuria on urinalysis were excluded from the study.
MS was defined by using the criteria established by the National Cholesterol Education Program-Adult Treatment Panel III-American Heart Association/National Heart, Lung, and Blood Institute (NCEP ATPIIIAHA/NHLBI) statement published in 2005. MS was diagnosed when at least three of the following criteria were present: 1) WC of ≥90 cm, 2) TG levels of ≥150 mg/dl, 3) HDL-C levels of <40 mg/dl, 4) systolic blood pressure (SBP) ≥130 mmHg and/or diastolic blood pressure (DBP) ≥85 mmHg and/or pharmacological treatment, and 5) FPG of ≥100 mg/dl. Central obesity was defined as WC ≥90 cm in men or ≥80 cm in women by the modified ATP III guideline that the World Health Organization Western Pacific Region and the International Association for the Study of Obesity presented for Asian populations in 2000. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2).
All parameters were measured on fresh blood samples obtained from overnight-fasting patients. PV was measured according to the prostate ellipsoid formula, multiplying the largest anteroposterior (height, H), transverse (width, W), and cephalocaudal (length, L) prostate diameters by 0.524 (H×W×L×π/6) by using TRUS (ALOKA, prosound-α5sv).
PASW ver. 18.0 (IBM Co., Armonk, NY, USA) was used for all statistical analyses. The mean value and independent t-test were used to compare the PV and serum PSA level in men with and without each metabolic component. Linear regression analysis was performed to compare the relationship between serum PSA level, PV, and clustering of MS components. A p-value of less than 0.05 was considered statistically significant.
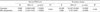
The mean age of the patients was 53.8±6.9 years. The mean PV and mean serum PSA level in the patients were 26.8±8.2 ml and 1.0±0.7. The baseline characteristics of men with and without MS are shown in Table 1. There were no statistically significant differences between the two groups in mean age, height, BMI, or total cholesterol level. In the patients with MS, the weight (p<0.001), WC (p<0.001), SBP (p<0.001), DBP (p<0.001), TG (p<0.001), and FPG (p<0.001) were significantly higher, and the HDL-C (p<0.001) was significantly lower, than in the patients without MS. In addition, serum PSA level and PV were significantly higher in the patients with MS than in the patients without MS, respectively (p<0.001, p<0.001).
The differences in PV and serum PSA level according to the presence of each metabolic component are shown in Table 2. The patients with central obesity (p<0.0001, <0.0001), high SBP (p=0.021, p=0.003), high DBP (p=0.001, p<0.0001), high TG (p=0.001, p<0.0001), low HDL-C (p=0.012, p<0.0001), and high FPG (p=0.0001, p<0.0001) had significantly higher serum PSA levels and larger PVs than did the patients without these conditions. Therefore, the presence of metabolic components in these patients was significantly related to higher serum PSA level and larger PV.
The frequencies of zero, one, two, three, four, and five MS components were 74 (17.6%), 114 (27.2%), 90 (21.4%), 88 (20.9%), 44 (10.5%), and 10 (2.4%), respectively. The relationship between PV, serum PSA level, and the sum of MS components is shown in Table 3. The serum PSA level was increased similarly with the increasing sum of MS components (R2=0.104, p<0.0001). Every increase in an MS component resulted in an increase of approximately 0.17 ng/dl in the serum PSA level. There was a significant contribution of MS components to PV also (R2=0.139, p<0.0001), with an increase of approximately 2.28 ml in PV for every component increase in MS components.
BPH is a complex and highly prevalent disease in men older than 50 years and it may lead to aggravation in the quality of life of suffering men [1,2]. Previous studies have shown that BPH is associated with several etiologic factors that may influence the prostate pathophysiology [12-14].
Recently, many studies have also shown that components of MS (central obesity, hypertension, NIDDM, hyperlipidemia, low HDL-C, hypertriglyceridemia) are risk factors for BPH development and that these components may play a part in BPH pathogenesis [12-14]. Hammarsten and Hogstedt [13,14] reported that men with MS had a significantly larger PV and faster annual BPH growth rates than did men without MS. In particular, central obesity, NIDDM, hypertension, low HDL-C, and high fasting insulin level are risk factors in the development of BPH [14-17]. Ozden et al. [4] demonstrated that PV was positively correlated with central obesity, as represented by WC, but that overall obesity measured by BMI was not correlated with PV. There was no significant relationship between obesity-related parameters and LUTS [18]. The present study illustrated that patients with high WC, high SBP/DBP, high TG, low HDL-C, and high FPG level had a significantly larger PV.
The serum PSA level test is a screening tool that is the most widely used marker for the early detection of prostate cancer and is used in the management of the disease after the diagnosis of BPH [19]. The serum PSA level may be influenced by many factors, such as age, BMI, PV, and prostate disease [19,20]. Han et al. [9] reported trends for a positive association between older age, diastolic BP, and the serum PSA level, whereas BMI, HDL, and FBG correlated negatively with the serum PSA level. We demonstrated that patients with central obesity, high SBP/DBP, high TG, low HDL-C, and high FPG had a significantly higher serum PSA level than did patients without these conditions.
Although several investigators have observed a significant association between BPH and MS or its components, others have opposing opinions. Gupta et al. [17] suggested that there were no significant relationships between BPH and MS, weight, BMI, lipid level, or thyroid hormone status. Jeong et al. [8] suggested that MS was not associated with PSA level in a screened population. Among the risk factors for MS, BP, WC, and FPG were independently associated with serum PSA levels [8]. Unfortunately, the relationships between PV, serum PSA level, and components of MS have not been clearly established and there is no consensus on the basis of recent results.
However, in the present study, most of the metabolic components were significantly related to larger PVs and a higher serum PSA level. Also, patients with more numerous MS components had increased serum PSA levels and PV. In general, MS develops as a result of westernized diet and lifestyle, which are in turn are related with obesity and insulin resistance [21]. Central obesity also contributes to insulin resistance [22]. Adipose tissue secretes several substances (adipocytokines), and these substances can induce insulin resistance. Several reports have suggested that insulin resistance with hyperinsulinemia is related to prostate enlargement [21,22]. Hypertension was also associated with BPH/LUTS in several animal models and epidemiologic studies. Golomb et al. [23] reported that spontaneously hypertensive rats develop BPH-like features with aging in the absence of any inductive exogenous agents. Similar to obesity, the relationship between BPH and dyslipidemia has been documented in several epidemiologic studies [24]. Hammarsten et al. [10] examined the data of 158 men and reported that individuals with a low HDL-C level had a larger PV and a higher annual BPH growth rate than did individuals with a high HDL-C level. Hyperinsulinemia contributes to activation of the sympathetic nerve system and leads to an increased level of catecholamine in the tissue [25]. It may also contribute to MS development and increased smooth muscle tone of the prostate, leading to severe LUTS [24,26]. These observations suggest that components of MS may interact to increase the risk of BPH. As seen in the above mentioned studies, each study reported different results for the relationship between MS components and PSA. These differences can be attributed to the different sample sizes and different selection process of the study subjects. Also, there are several studies confirming a correlation between the serum PSA level and PV [25,27]. PV is strongly related to serum PSA and age in men with symptomatic BPH and in whom prostate cancer has been excluded. PSA can also be used as an aid to estimate the degree of prostate enlargement [28,29]. In summary, because patients with MS components have a larger PV than do patients without MS components, larger PV is related to a high serum PSA level.
Possible limitations of our study should be considered. This study reported a different result for the relationship between PSA and MS components from the result of Jeong et al. [8]. The small sample size may have influenced the difference in results. Our study was not community-based; however, the subjects were healthy and were applicants for a routine health screening. Therefore, the serum PSA levels of our study subjects may not be significantly different from the serum PSA levels of a community-based population. In addition, prostate biopsy was not performed in all study subjects. The presence of undiagnosed prostate cancer could have confounded our results. Therefore, a prospective, community-based study including prostate biopsy is necessary to verify whether MS influences the accuracy of the serum PSA level test and PV measurement.
We demonstrated that MS components were associated with larger PV and a high serum PSA level. Each MS component could be an important factor in the development and management of BPH. When treating patients with BPH, the MS components of patients should be considered and should be managed. Further studies are needed to confirm the relationship between MS components and BPH and to explain the underlying mechanisms.
Figures and Tables
References
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.
2. Issa MM, Regan TS. Medical therapy for benign prostatic hyperplasia: present and future impact. Am J Manag Care. 2007. 13:Suppl 1. S4–S9.
3. Mongiu AK, McVary KT. Lower urinary tract symptoms, benign prostatic hyperplasia, and obesity. Curr Urol Rep. 2009. 10:247–253.
4. Ozden C, Ozdal OL, Urgancioglu G, Koyuncu H, Gokkaya S, Memis A. The correlation between metabolic syndrome and prostatic growth in patients with benign prostatic hyperplasia. Eur Urol. 2007. 51:199–203.
5. Lee C, Kozlowski JM, Grayhack JT. Etiology of benign prostatic hyperplasia. Urol Clin North Am. 1995. 22:237–246.
6. Ziada A, Rosenblum M, Crawford ED. Benign prostatic hyperplasia: an overview. Urology. 1999. 53:3 Suppl 3a. 1–6.
7. Hammarsten J, Hogstedt B. Clinical, anthropometric, metabolic and insulin profile of men with fast annual growth rates of benign prostatic hyperplasia. Blood Press. 1999. 8:29–36.
8. Jeong IG, Hwang SS, Kim HK, Ahn H, Kim CS. The association of metabolic syndrome and its components with serum prostate-specific antigen levels in a Korean-screened population. Cancer Epidemiol Biomarkers Prev. 2010. 19:371–380.
9. Han JH, Chang IH, Ahn SH, Kwon OJ, Bang SH, Choi NY, et al. Association between serum prostate-specific antigen level, liver function tests and lipid profile in healthy men. BJU Int. 2008. 102:1097–1101.
10. Hammarsten J, Hogstedt B, Holthuis N, Mellstrom D. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998. 1:157–162.
11. Eom CS, Park JH, Cho BL, Choi HC, Oh MJ, Kwon HT. Metabolic syndrome and accompanying hyperinsulinemia have favorable effects on lower urinary tract symptoms in a generally healthy screened population. J Urol. 2011. 186:175–179.
12. Bosch RJ. Pathogenesis of benign prostatic hyperplasia. Eur Urol. 1991. 20:Suppl 1. 27–30.
13. Hammarsten J, Hogstedt B. Calculated fast-growing benign prostatic hyperplasia: a risk factor for developing clinical prostate cancer. Scand J Urol Nephrol. 2002. 36:330–338.
14. Hammarsten J, Hogstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001. 39:151–158.
15. Hammarsten J, Hogstedt B. Clinical, haemodynamic, anthropometric, metabolic and insulin profile of men with high-stage and high-grade clinical prostate cancer. Blood Press. 2004. 13:47–55.
16. Matsuda T, Abe H, Suda K. Relation between benign prostatic hyperplasia and obesity and estrogen. Rinsho Byori. 2004. 52:291–294.
17. Gupta A, Gupta S, Pavuk M, Roehrborn CG. Anthropometric and metabolic factors and risk of benign prostatic hyperplasia: a prospective cohort study of Air Force veterans. Urology. 2006. 68:1198–1205.
18. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991. 14:173–194.
19. Baillargeon J, Pollock BH, Kristal AR, Bradshaw P, Hernandez J, Basler J, et al. The association of body mass index and prostate-specific antigen in a population-based study. Cancer. 2005. 103:1092–1095.
20. Kristal AR, Chi C, Tangen CM, Goodman PJ, Etzioni R, Thompson IM. Associations of demographic and lifestyle characteristics with prostate-specific antigen (PSA) concentration and rate of PSA increase. Cancer. 2006. 106:320–328.
21. Becker S, Dossus L, Kaaks R. Obesity related hyperinsulinaemia and hyperglycaemia and cancer development. Arch Physiol Biochem. 2009. 115:86–96.
22. Giovannucci E, Rimm EB, Chute CG, Kawachi I, Colditz GA, Stampfer MJ, et al. Obesity and benign prostatic hyperplasia. Am J Epidemiol. 1994. 140:989–1002.
23. Golomb E, Rosenzweig N, Eilam R, Abramovici A. Spontaneous hyperplasia of the ventral lobe of the prostate in aging genetically hypertensive rats. J Androl. 2000. 21:58–64.
24. Rahman NU, Phonsombat S, Bochinski D, Carrion RE, Nunes L, Lue TF. An animal model to study lower urinary tract symptoms and erectile dysfunction: the hyperlipidaemic rat. BJU Int. 2007. 100:658–663.
25. Hochberg DA, Armenakas NA, Fracchia JA. Relationship of prostate-specific antigen and prostate volume in patients with biopsy proven benign prostatic hyperplasia. Prostate. 2000. 45:315–319.
26. Vikram A, Jena GB, Ramarao P. Increased cell proliferation and contractility of prostate in insulin resistant rats: linking hyperinsulinemia with benign prostate hyperplasia. Prostate. 2010. 70:79–89.
27. Bosch JL, Hop WC, Bangma CH, Kirkels WJ, Schroder FH. Prostate specific antigen in a community-based sample of men without prostate cancer: correlations with prostate volume, age, body mass index, and symptoms of prostatism. Prostate. 1995. 27:241–249.
28. Roehrborn CG, Boyle P, Gould AL, Waldstreicher J. Serum prostate-specific antigen as a predictor of prostate volume in men with benign prostatic hyperplasia. Urology. 1999. 53:581–589.
29. Mochtar CA, Kiemeney LA, van Riemsdijk MM, Barnett GS, Laguna MP, Debruyne FM, et al. Prostate-specific antigen as an estimator of prostate volume in the management of patients with symptomatic benign prostatic hyperplasia. Eur Urol. 2003. 44:695–700.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download