Abstract
We report a case of primary penile undifferentiated sarcoma. A 16-year-old adolescent man visited Pusan National University Hospital complaining of a painless mass on his penis that was increasing in size. Magnetic resonance images revealed a 5×5-cm mass and pathological examinations revealed small round cell sarcomas with neuroendocrine differentiation. The tumor, which had metastatic pulmonary nodules, was treated by tumorectomy and systemic chemotherapy. Thirty-four months after the initial diagnosis, the patient was still alive without evidence of local recurrence or metastatic disease. This is our second case of an undifferentiated penile sarcoma.
Primary penile sarcoma is a rare disease. The prevalence of penile malignancies varies from 0.5 to 5 cases in every 100,000 males, with sarcomas consisting of less than 5% of all types of penile malignancies [1,2]. Among the cases of penile sarcomas, vascular sarcomas are the most common type, followed by rhabdomyosarcomas, leiomyosarcomas, and fibrosarcomas, which also include soft tissue sarcomas. Other types are much more rare [3]. Sixteen cases of epithelioid sarcomas and only 1 case of undifferentiated sarcoma have so far been documented in the English language literature [1,4]. Here we report the case of a 16-year-old boy, the youngest penile sarcoma patient ever recorded, with a brief review of the literature.
A 16-year-old boy was presented to our clinic complaining of a painless mass on his penis that was increasing in size. The fist-sized mass had a firm consistency without inguinal lymphadenopathy. The patient had been unaware of the existence of the mass until his urinary stream weakened. However, the mass had recently been growing rapidly with intermittent pain.
Magnetic resonance images revealed a 5×5-cm mass invading the left corpus cavernosum and corpus spongiosum (Fig. 1). Several inguinal lymph node enlargements were found; however, their diameters were less than 10 mm, which suggested that they were reactive lymph nodes. On cystourethroscopy, the penile urethra appeared to have been compressed by an external mass and mucosal erythemas were found around the mass. There were no abnormal findings on the chest computed tomography (CT) or bone scan. Laboratory examinations including urine analysis showed nonspecific findings. Core biopsy of the mass revealed a small round cell tumor.
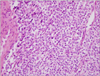
Tumorectomy was performed because the patient and his mother wished penile preservation. A circular subcoronal and ventral penile longitudinal incision was made. Although the tumor had rich vascularity, dissection between the tumor and the overlying penile skin was not difficult. The corpus cavernosum and the corpus spongiosum that were invaded by the tumor were partially resected and repaired. A large mass was identified on the penile shaft (Fig. 2). Pathological examinations revealed small round cell sarcomas with neuroendocrine differentiation (Fig. 3). The surgical margin appeared most likely to be free of tumor and there were multiple lymphovascular tumor emboli with poorly defined mitotic figures. Immunohistochemical study showed that reactivity to CD56 and vimentin was positive and reactivity to CD34, CD31, factor-VIII, cytokeratin, smooth muscle actin, CD99, and c-kit was negative. The reactivity to epithelial membrane antigen (EMA) was weakly positive.
A follow-up chest CT performed 1 month after the surgery showed multiple nodules of less than 1 cm in size in both lung fields. These lung nodules were removed by use of CT-guided biopsy, which revealed metastatic small round cell sarcomas identical to the penile mass. Therefore, chemotherapeutic treatment was planned.
According to the surgicopathologic staging system of the Intergroup Rhabdomyosarcoma Study Group, our case belonged to Group IV, and according to the International Union Against Cancer staging system, his case was classified as stage 4. The patient underwent chemotherapy with etoposide (100 mg/m2/day) and ifosfamide (1.8 g/m2/day) and regular CT control every 3 months. Despite chemotherapy, however, the size of the nodules did not change. We then changed the regimen of chemotherapy to vincristine (1.5 mg/m2/day, maximum dose 2 mg/day, weekly), actinomycin-D (1.5 mg/m2/day, maximum 2.5 mg/day, every 3 weeks), and cyclophosphamide (2.2 g/m2/day, every 3 weeks) because his cumulative dose of ifosfamide had exceeded 69.4 g/m2. Until week 6 of the second-line chemotherapy passed, there was no evidence of a decrease in the size of the lung nodules. However, wedge resection of the two nodules on right upper lobe was then performed and the specimens revealed no residual tumor cells. After a total of 42 weeks of chemotherapy and 34 months of follow-up, the patient showed no evidence of distant metastases.
Primary penile sarcoma is very rare and its etiology remains unknown. Diagnosis of this disease is difficult because the disease often has a benign appearance as painless nodules similar to Peyronie's disease, and it is morphologically similar to granuloma and chronic inflammation [5]. The slow-growing nature of several sarcomas often leads to late diagnosis and treatment, although penile sarcoma requires early treatment with multiple therapeutic modalities.
The diagnostic challenges and subsequent uncertain clinical management related to undifferentiated or primitive sarcomas in children and adolescents remain unresolved. The confusion is also enhanced by the grouping of small, blue, round cell tumors together with sarcomas displaying a spindle-fascicular growth, resembling "infantile fibrosarcoma," under the meaningless term of undifferentiated sarcoma. Some of the larger series investigating this issue come from the Intergroup Rhabdomyosarcoma Study (IRS) [6]. Among the 1,527 patients entered on IRS-III and IRS pilot-IV, 34 (5%) remained unclassified after retrospective re-review and application of immunohistochemical ancillary techniques (but not molecular diagnostic techniques). The incidence of similar histology among soft tissue sarcoma in adults remains undefined.
Penile epithelioid sarcoma is a much rarer type of soft tissue sarcoma than is penile leiomyosarcoma and was first described by Enzinger in 1970 [7]. Epithelioid sarcoma has aggressive mesenchymal malignant entities, usually in the upper and lower extremities of young adults. The penis is the site where primary epithelioid sarcoma rarely occurs. Only 16 cases have been reported so far [1,5,7].
Penile undifferentiated sarcoma is an extremely rare disease. Only one English language case report exists. The patient was 78 years old. The present case is the second case of penile undifferentiated sarcoma.
The superficial type of leiomyosarcomas arises from 1) the dartos muscle layer of the prepuce and shaft, 2) the erector pilorum muscle of the penile shaft, or 3) the muscular wall of superficial vessels. Patients with the superficial type of tumor generally lack symptoms such as dysuria and obstruction. The deep type of leiomyosarcomas originates from the smooth muscles of deep vessels that constitute the corpus spongiosum and the corpus cavernosum. This type grows rapidly within several months with more frequent urinary symptoms and distant metastasis.
Common symptoms of penile epithelioid sarcoma include penile nodularity or mass, urethral stenosis, penile curvature, and dysuria. Lesions are often mistaken for other diseases, such as Peyronie's disease. The most important symptom distinguishing penile sarcoma from Peyronie's disease is urethral narrowing. The sarcomatous condition shows positive symptoms and signs of urethral narrowing [1].
Core biopsy is necessary when making a differential diagnosis of penile sarcoma histopathologically. Leiomyosarcoma is composed of ill-defined bundles of smooth muscle cells and spindle-shaped smooth muscle fibers with blunt-ended cigar-shaped nuclei arranged into interlacing fascicles on light microscopy. Electron microscopic findings include myofibrils, dense bodies, and abundant pinocytic vesicles and a continuous basal lamina is present around most of the tumor cells. Immunoreactivity for vimentin, muscle-specific actin, smooth muscle actin, and desmin are positive in leiomyosarcoma [2,8,9].
Geographic necrosis, a central degeneration or necrosis of a tumor, is a common feature of epithelioid sarcoma. Tumor cells are round, polygonal, or spindle-shaped with densely eosinophilic cytoplasm, often surrounding an area of central necrosis [1,5]. However, it is difficult to distinguish epithelioid sarcoma from other types of sarcoma and inflammatory diseases through conventional light microscopy, especially in the unusual primary site [1]. Coexpression of vimentin, cytokeratin AE1/AE3, CD34, and EMA, without expression of desmin, smooth muscle actin, factor VIII-related antigen, or CD31 are the basic immunohistochemical characteristics [1,5].
The superficial type of leiomyosarcoma has a good prognosis with only a local excision or amputation. Distant metastasis is rarely observed [2,3,8,10]. The deep type of leiomyosarcoma requires more aggressive treatments, including radical penectomy, radiation therapy, and chemotherapy, although the outcome of these treatments is still poor. In one study, it was reported that 69% (9/13) of patients died within 3 years after diagnosis because of multiple metastases and dissemination of the disease [9]. Excision of the regional lymph nodes in deep type leiomyosarcoma has no definite benefits for a patient's survival contrary to squamous cell carcinoma of the penis. Also, radiation therapy and chemotherapy produce little effect in treating leiomyosarcoma of the penis, but they might decrease the risk of local and distant recurrence postoperatively [2,3]. Accepted poor prognostic factors of leiomyosarcoma include deep tumor depth, a tumor size of greater than 5 cm, a high meiotic rate, and necrosis [2,3,8,10].
Total or partial penectomy is the treatment choice in most patients with penile epithelioid sarcoma, despite a high local recurrence rate after surgery of up to 80% and occurrence rates of pulmonary and regional lymph node metastasis of up to 51% and 30%, respectively [7]. The 5-year survival rate is 70% and the 10-year survival rate is 50%, similar to those of epithelioid sarcoma with classical lesions [1]. Adjuvant radiation therapy has some beneficial effects on the local control of high-grade resected sarcoma, contrary to adjuvant chemotherapy, though it is still debatable. Advanced age, tumor size of greater than 5 cm, deep location, nuclear polymorphism, high mitotic activity, and the presence of vascular invasion are acceptable poor prognostic factors of penile epithelioid sarcoma [1,5,7]. In the first reported case, the patient underwent neoadjuvant chemotherapy with doxorubicin (25 mg/m2/day) and iphosphamide (1.7 mg/m2/day) from day 1 to day 3 followed by intensity-modulated radiotherapy (total dose of 66 Gy) of the pelvic area and total penectomy. The patient received an extra course of chemotherapy using Taxotere (36 mg/m2) and gemcitabine (800 mg/m2) from day 1 to day 8. In that case, the patient had local and systemic progression to adjacent fat tissue and pulmonary and hepatic nodules despite total penectomy, systemic chemotherapy, and radiation therapy. He died 17 months after the initial diagnosis of the disease (Table 1) [4].
Multiple types of primary sarcomas can also arise from the penis, although they are very rare. There is no established standard therapy because of the small number of cases so far. Further studies are needed to determine the standard therapeutic modalities for these diseases.
Figures and Tables
 | FIG. 1Magnetic resonance images showing a 5-cm mass lesion on the left side of the penis. The mass invaded the corpus cavernosum and corpus spongiosum. This mass arising from the corpus cavernosum showed heterogeneous high signal intensity on the T2-weighted image. |
 | FIG. 2Gross findings of the penile mass. The hypervascular mass is present on the left side of the penis and had a hard consistency and irregular shape. The mass grossly invaded the corpus cavernosum and spongiosum. |
References
1. Hoebeke PB, Rottey S, Van Heddeghem N, Villeirs G, Pauwels P, Schrauwen W, et al. One-stage penectomy and phalloplasty for epithelioid sarcoma of the penis in an adolescent: part 2. Eur Urol. 2007. 51:1744–1747.
2. Katsikas VS, Kalyvas KD, Ioannidis SS, Papathanasiou MV, Panagiotopoulou KP, Hitiroglou PM, et al. Leiomyosarcoma of the penis. Sarcoma. 2002. 6:75–77.
3. Dominici A, Delle Rose A, Stomaci N, Pugliese L, Posti A, Nesi G. A rare case of leiomyosarcoma of the penis with a reappraisal of the literature. Int J Urol. 2004. 11:440–444.
4. El Hayek OR, Ibrahim R, Lemos GC. Pleomorphic undifferentiated sarcoma of the penis. Clinics (Sao Paulo). 2008. 63:841–842.
5. Sirikci A, Bayram M, Demirci M, Bakir K, Sarica K. Penile epithelioid sarcoma: MR imaging findings. Eur Radiol. 1999. 9:1593–1595.
6. Pawel BR, Hamoudi AB, Asmar L, Newton WA Jr, Ruymann FB, Qualman SJ, et al. Undifferentiated sarcomas of children: pathology and clinical behavior--an Intergroup Rhabdomyosarcoma study. Med Pediatr Oncol. 1997. 29:170–180.
7. Enzinger FM. Epitheloid sarcoma. A sarcoma simulating a granuloma or a carcinoma. Cancer. 1970. 26:1029–1041.
8. Fetsch JF, Davis CJ Jr, Miettinen M, Sesterhenn IA. Leiomyosarcoma of the penis: a clinicopathologic study of 14 cases with review of the literature and discussion of the differential diagnosis. Am J Surg Pathol. 2004. 28:115–125.
9. Sundersingh S, Majhi U, Narayanaswamy K, Balasubramanian S. Primary leiomyosarcoma of the penis. Indian J Pathol Microbiol. 2009. 52:447–448.
10. Glucker E, Hirshowitz B, Gellei B. Leiomyosarcoma of the glans penis. Case report. Plast Reconstr Surg. 1972. 50:406–408.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download