Abstract
Purpose
We aimed to compare the cystatin C-based estimated glomerular filtration rate (eGFR) and the serum creatinine-based eGFR and to investigate the clinical roles of the cystatin C-based eGFR in assessing the follow-up renal function of kidney donors.
Materials and Methods
We enrolled 121 healthy kidney donors who underwent live donor nephrectomy between October 2009 and December 2010 in a prospective manner. Serum creatinine and cystatin C were measured preoperatively and were followed after the surgery (1st, 4th, and 7th postoperative day and 1st, 3rd, 6th, and 12th postoperative month). We also compared the sensitivity and specificity of each eGFR method for predicting the development of chronic kidney disease (CKD) after donor nephrectomy.
Results
For those who had a Modification of Diet in Renal Disease postoperative day 4 eGFR of less than 60 ml/min/1.73 m2, the probability of developing CKD was 89.0% (Chronic Kidney Disease Epidemiology Collaboration eGFR, 66.0%; Cockcroft-Gault eGFR, 74.0%; cystatin C eGFR, 57.1%). A cystatin C eGFR of below 60 ml/min/1.73 m2 at postoperative day 4 predicted CKD at 6 months with a specificity of 90.3%, which was the highest among the estimation methods used. Cystatin C eGFRs were generally higher than the creatinine-based eGFRs.
Conclusions
We conclude that cystatin C-based estimations of the GFR are helpful for predicting the recovery of renal function in kidney donors and could be added to the follow-up protocol of kidney donors who may develop CKD, especially patients whose immediate postoperative renal function is marginal.
Long-term studies of healthy kidney donors have shown that living kidney donation is safe and rarely affects the individual's health [1]. However, some studies have reported decreased renal function during short to intermediate follow-up periods after living-donor nephrectomy [2,3]. Although controversy over the impact of nephrectomy on donor health exists, chronic kidney disease (CKD) has recently been shown to be an important risk factor for cardiovascular disease, thus highlighting the importance of living kidney donor follow-up [4]. Currently, there is no standard follow-up protocol for kidney donors following nephrectomy. Regular hospital visits are burdensome and are still considered unnecessary for healthy kidney donors [5]. The most important follow-up factor is kidney filtration of waste products from the circulation, which is defined as the glomerular filtration rate (GFR). The GFR can be estimated by measuring creatinine clearance in the urine. In the clinical setting, however, because of the difficulty in collecting urine (usually taking 24 hours), estimated creatinine clearance or estimated GFR (eGFR) is used instead. Many formulas are available for generating the eGFR on the basis of measured serum creatinine levels [6-8]. An alternative method uses serum cystatin C, a low molecular weight protein secreted by most cells in the body [9]. Whereas serum creatinine varies with patient age, gender, and muscle mass, serum cystatin C concentrations appear to be independent of those individual factors [10]. In this study, we compared the sensitivity and specificity of each eGFR method for predicting CKD development by use of sequential follow-up after donor nephrectomy and investigated the clinical roles of serum cystatin C eGFRs versus serum creatinine-based eGFRs.
From October 2009 to December 2010, a total of 121 healthy kidney donors underwent donor nephrectomy at our institution. Preoperatively, patient medical histories were taken and all donors underwent serum tests including measurement of creatinine and cystatin C, random urine analysis, and measurement of the creatinine clearance rate by use of 24-hour urine collection. Patients also underwent 99mtechnetium diethylenetriaminepentaacetic acid renal scintigraphy and angio-computerized tomography for evaluation of the renovascular system. Serum creatinine and cystatin C values were obtained on the 1st, 4th, and 7th postoperative day and at the 1st, 3rd, 6th, and 12th postoperative month.
We used the Jaffe method (Hitachi 7600, Hitachi High Technologies Co., Osaka, Japan) for serum creatinine measurement. Serum creatinine levels were converted to eGFRs by using three different GFR estimation equations:
1) the Modification of Diet in Renal Disease (MDRD) equation,
MDRD eGFR (ml/min/1.73 m2)=186×(SCr)-1.154×(age)-0.203×(0.742 if female);
2) the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation,
CKD-EPI eGFR (ml/min/1.73 m2)=141×min (SCr/k or 1)α×max (SCr/k or 1)-1.209×0.993age×1.018 (if female),
where k is 0.7 for females and 0.9 for males, α is -0.329 for females and -0.411 for males, min indicates the minimum of SCr/k or 1, and max indicates the maximum of SCr/k or 1;
and 3) the Cockcroft-Gault (GC) equation,
GC eGFR (ml/min/1.73 m2)=(140-age×(weight in kg)×(0.85 if female)/(72×SCr).
Serum cystatin C levels were measured by using a particle-enhanced immunonephelometric assay (Roche Tinaquant Cystatin C, Roche Cobas 6000 turbidimetry, Roche Diagnostics, Barcelona, Spain). We used the Larsson equation for GFR estimation:
Cys C eGFR (ml/min/1.73 m2)=77.239×(1.0675×cystatin C [mg/l]-0.1)-1.2623.
If the MDRD eGFR was lower than 60 ml/min/1.73 m2 during the follow-up, the patient was diagnosed with "chronic kidney disease" [11]. Depending on the MDRD eGFR at the 6th postoperative month, we divided the patients into either the CKD group or the normal group. After institutional review board approval, we compared the preoperative and postoperative eGFRs (MDRD, CKD-EPI, GC, and cystatin C) according to the estimation method used and graphed these data on a scatter plot. We analyzed the relationship of postoperative day 4 eGFR values and CKD development by using receiver operating characteristic (ROC) curves. Statistically significant differences between groups were defined by p-values<0.05. All data analyses were processed with PASW ver. 18 (IBM Co., Armonk, NY, USA).
Of 121 kidney donor patients, postoperative 6-month follow-up data were available for 80 cases. Among them, 27 patients (33.8%) had an MDRD eGFR less than 60 ml/min/1.73 m2, which is the standard definition of CKD. The patients' mean age was 39.7±11.6 years, and their mean BMI was 23.2±2.8 kg/m2. Creatinine and cystatin C serum levels increased immediately after nephrectomy (Table 1). The eGFR values obtained from the four different equations varied before and after the surgery, but cystatin C-based eGFR values were the highest of all the methods used. This finding was consistent for the preoperative, postoperative day 4, and postoperative 6 months data. We drew scatter plots with the eGFR data both before nephrectomy (Fig. 1A) and at 6 months after the donor surgery (Fig. 1B). With use of the MDRD eGFR as the reference, the CKD-EPI eGFR had the strongest correlation with reference values (CKD-EPI eGFR preoperative r2=0.904, postoperative r2=0.984; cystatin C eGFR preoperative r2=0.124, postoperative r2=0.184; GC eGFR preoperative r2=0.188, postoperative r2=0.146). Cystatin C eGFR values had a definite tendency toward being the highest among the four eGFRs evaluated at all time points.
For those who had an MDRD postoperative day 4 eGFR less than 60 ml/min/1.73 m2, the chance of acquiring CKD (GFR<60 ml/min/1.73 m2 at postoperative 6 months) was 89.0%. The probability was 66.0% when the CKD-EPI eGFR was used, 74.0% with the GC eGFR, and 57.1% with use of the cystatin C eGFR (Table 2). In contrast, a cystatin C eGFR below 60 ml/min/1.73 m2 at postoperative day 4 predicted CKD at 6 months with a specificity of 90.3%, which was the highest among the estimation methods used.
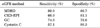
We generated an ROC curve by using the sensitivity and specificity data for CKD prediction derived from each eGFR method (Fig. 2). The area under the curve of the MDRD eGFR was 0.845 (95% confidence interval [CI], 0.763 to 0.928), that of the CKD-EPI eGFR was 0.844 (95% CI, 0.761 to 0.928), that of the GC eGFR was 0.712 (95% CI, 0.581 to 0.843), and that of the cystatin C eGFR was 0.674 (95% CI, 0.551 to 0.797).
We measured preoperative and postoperative GFRs in kidney donors by using serum cystatin C and creatinine levels. Preoperative cystatin C eGFRs were slightly higher than the creatinine-based eGFRs, and this tendency continued throughout the postoperative follow-up period. Compared with the MDRD eGFR, the cystatin C eGFR was more useful for predicting renal function recovery, especially for patients whose immediate postoperative renal function was marginal.
We defined CKD as an MDRD postoperative 6 months eGFR lower than 60 ml/min/1.73 m2. When the MDRD postoperative day 4 eGFR was lower than 60 ml/min/1.73 m2, the chance of developing CKD was 89.0%. In contrast, among the patients whose cystatin C postoperative day 4 eGFR was lower than 60 ml/min/1.73 m2, only 57.1% developed CKD. Regarding specificity, the MDRD postoperative day 4 eGFR showed 66.7% specificity for predicting CKD development, whereas in the same patient group the cystatin C eGFR demonstrated 90.3% specificity.
Kidney donor renal function is reported to decrease 30 to 40% after donor nephrectomy [1-3]. After CKD was found be an important cardiovascular disease risk factor, institutes that had used extended kidney donation criteria started to focus more on donors' renal function during their follow-up [4]. It is now generally accepted that scheduled GFR check-ups are mandatory for patients who have donated a kidney [5]. Insulin-based GFR measurement is accurate but takes too much time. Creatinine-based GFR estimation is generally precise but may be affected by the kidney surgery itself during the acute compensatory period. The cystatin C eGFR has the advantages described above and is also less affected by the dynamic and hyperfiltrating renal status following donor nephrectomy. On this basis, we designed a prospective study protocol to compare cystatin C eGFRs with the various creatinine eGFRs.
Previous studies have shown that serum cystatin C is comparable to serum creatinine as a marker of glomerular filtration changes after donor nephrectomy [12-14]. Additionally, our results suggest that cystatin C may assist in predicting CKD in the immediate postoperative period. Because the creatinine-based MDRD eGFR had good sensitivity but poor specificity, whereas the cystatin C-based eGFR had good specificity and poor sensitivity, measuring both cystatin C and creatinine during follow-up will produce a synergistically increased accuracy in predicting kidney donors' outcomes.
The higher mean cystatin C eGFR values compared with creatinine eGFR values can be interpreted in two ways: cystatin C eGFR overestimation or creatinine eGFR underestimation. We could not reach a certain conclusion in this respect because both GFR estimation methods were sufficiently reliable in the given situation [13]. Louvar et al. [14] reported similar results in postnephrectomy donors, but they did not specify the reason.
As a prospective study, our results are more reliable than previous studies using a retrospective design. However, because all laboratory results came from a single institution, the risk of laboratory error exists. There are significant differences in cystatin C measurement across laboratories even with the use of an identical assay from the same manufacturer [15]. The IFCC Working Group for Standardization of Cystatin C has been trying to produce and characterize cystatin C reference materials [16]. Cystatin C measurement standardization has not yet been established. However, cystatin C has more beneficial aspects for renal function measurement compared with creatinine, and cystatin C eGFR equations appear to be simpler and more accurate than creatinine-based equations [17]. The cystatin C eGFR is known to be more reliable that serum creatinine-based tests in mild kidney dysfunction [18,19]. Especially in the diabetic population, cystatin C was shown to be superior in detecting renal function decline in comparison with creatinine-based methods [20,21]. Furthermore, acute kidney injury can be detected earlier by serum cystatin C measurement than by evaluating serum creatinine. When renal function is diminished, serum cystatin C reflects GFR changes 1 or 2 days earlier than serum creatinine; thus, cystatin C may allow earlier detection of acute renal failure [22,23].
Louvar et al. [14] reported that cystatin C eGFR models generally overestimate the eGFR value after live donor nephrectomy. In this study, the eGFR values using cystatin C were usually higher than the values of the other creatinine-based eGFRs (i.e., MDRD, CKD-EPI, and GC) (Fig. 1A and 1B). However, controversy exists as to whether cystatin C eGFR equations really overestimate the GFR compared with creatinine-based equations. The serum cystatin C concentration is independent of patient age, gender, and muscle mass [9,12]. Therefore, we can assume that the cystatin C-based eGFR will be less biased than the creatinine-based eGFR by the decreased amount of exercise and muscle mass or alteration of diet in the immediate postoperative period. Also, it is still not evident whether kidney donors whose postoperative MDRD eGFR is CKD level 3 possess a risk of significant medical complication equal to the general CKD population [24,25]. Because no decisive reports are available, a large, prospective comparison study is required to reach certain conclusions.
When the cystatin C eGFR value was compared with the serum creatinine-based eGFR value, it overestimated the GFR in the overall follow-up period of kidney donors. However, the cystatin C eGFR (cutoff value<60 ml/min/1.73 m2) showed high prediction ability for CKD at postoperative 6 months. Therefore, we believe that cystatin C eGFR determination is helpful for the early detection of renal function recovery, especially for patients whose immediate postoperative renal function is marginal and who may develop CKD.
Figures and Tables
FIG. 1
Scattered plot of eGFR value distribution: (A) preoperative, (B) 6 months postoperative. Cystatin C-based values were generally higher than the other creatinine-based values. eGFR, estimated glomerular filtration rate; MDRD, the Modification of Diet in Renal Disease equation; CKD-EPI, the Chronic Kidney Disease Epidemiology Collaboration equation; GC, the Cockcroft-Gault equation.

FIG. 2
Receiver operating characteristic for CKD prediction by postoperative day 4 eGFR less than 60 ml/min/1.73 m2. The area under the curve of the MDRD eGFR was the highest (0.845; 95% CI, 0.763 to 0.928); that of the cystatin C eGFR was the lowest (0.674; 95% confidence interval, 0.551 to 0.797). CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; MDRD, the Modification of Diet in Renal Disease equation; CKD-EPI, the Chronic Kidney Disease Epidemiology Collaboration equation; GC, the Cockcroft-Gault equation.
References
1. Ibrahim HN, Foley R, Tan L, Rogers T, Bailey RF, Guo H, et al. Long-term consequences of kidney donation. N Engl J Med. 2009. 360:459–469.
2. Lee JH, Kim SC, Han DJ, Chang JW, Yang WS, Park SK, et al. Risk factors for MDRD-GFR of less than 60 ml/min per 1.73 m2 in former kidney donors. Nephrology (Carlton). 2007. 12:600–606.
3. Jeon HG, Lee SR, Joo DJ, Oh YT, Kim MS, Kim YS, et al. Predictors of kidney volume change and delayed kidney function recovery after donor nephrectomy. J Urol. 2010. 184:1057–1063.
4. Weiner DE, Tighiouart H, Amin MG, Stark PC, MacLeod B, Griffith JL, et al. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol. 2004. 15:1307–1315.
5. Mandelbrot DA, Pavlakis M, Karp SJ, Johnson SR, Hanto DW, Rodrigue JR. Practices and barriers in long-term living kidney donor follow-up: a survey of U.S. transplant centers. Transplantation. 2009. 88:855–860.
6. European Best Practice Guidelines Expert Group on Hemodialysis, European Renal Association. Section I. Measurement of renal function, when to refer and when to start dialysis. Nephrol Dial Transplant. 2002. 17:Suppl 7. 7–15.
7. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002. 39:2 Suppl 1. S1–S266.
8. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009. 150:604–612.
9. Westhuyzen J. Cystatin C: a promising marker and predictor of impaired renal function. Ann Clin Lab Sci. 2006. 36:387–394.
10. Filler G, Bokenkamp A, Hofmann W, Le Bricon T, Martinez-Bru C, Grubb A. Cystatin C as a marker of GFR--history, indications, and future research. Clin Biochem. 2005. 38:1–8.
11. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003. 139:137–147.
12. Herget-Rosenthal S, Pietruck F, Volbracht L, Philipp T, Kribben A. Serum cystatin C--a superior marker of rapidly reduced glomerular filtration after uninephrectomy in kidney donors compared to creatinine. Clin Nephrol. 2005. 64:41–46.
13. Gourishankar S, Courtney M, Jhangri GS, Cembrowski G, Pannu N. Serum cystatin C performs similarly to traditional markers of kidney function in the evaluation of donor kidney function prior to and following unilateral nephrectomy. Nephrol Dial Transplant. 2008. 23:3004–3009.
14. Louvar DW, Rogers TB, Bailey RF, Matas AJ, Ibrahim HN. Cystatin C is not superior to creatinine-based models in estimating glomerular filtration rate in former kidney donors. Transplantation. 2007. 84:1112–1117.
15. White CA, Rule AD, Collier CP, Akbari A, Lieske JC, Lepage N, et al. The impact of interlaboratory differences in cystatin C assay measurement on glomerular filtration rate estimation. Clin J Am Soc Nephrol. 2011. 6:2150–2156.
16. Grubb A, Blirup-Jensen S, Lindstrom V, Schmidt C, Althaus H, Zegers I, et al. First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin Chem Lab Med. 2010. 48:1619–1621.
17. Hojs R, Bevc S, Ekart R, Gorenjak M, Puklavec L. Serum cystatin C-based equation compared to serum creatinine-based equations for estimation of glomerular filtration rate in patients with chronic kidney disease. Clin Nephrol. 2008. 70:10–17.
18. Rule AD, Bergstralh EJ, Slezak JM, Bergert J, Larson TS. Glomerular filtration rate estimated by cystatin C among different clinical presentations. Kidney Int. 2006. 69:399–405.
19. Herget-Rosenthal S, Bokenkamp A, Hofmann W. How to estimate GFR-serum creatinine, serum cystatin C or equations? Clin Biochem. 2007. 40:153–161.
20. Lee BW, Ihm SH, Choi MG, Yoo HJ. The comparison of cystatin C and creatinine as an accurate serum marker in the prediction of type 2 diabetic nephropathy. Diabetes Res Clin Pract. 2007. 78:428–434.
21. Premaratne E, MacIsaac RJ, Finch S, Panagiotopoulos S, Ekinci E, Jerums G. Serial measurements of cystatin C are more accurate than creatinine-based methods in detecting declining renal function in type 1 diabetes. Diabetes Care. 2008. 31:971–973.
22. Herget-Rosenthal S, Marggraf G, Husing J, Goring F, Pietruck F, Janssen O, et al. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004. 66:1115–1122.
23. Nejat M, Pickering JW, Walker RJ, Endre ZH. Rapid detection of acute kidney injury by plasma cystatin C in the intensive care unit. Nephrol Dial Transplant. 2010. 25:3283–3289.
24. Barri Y, Parker T 3rd, Kaplan B, Glassock R. Primum non Nocere: is chronic kidney disease staging appropriate in living kidney transplant donors? Am J Transplant. 2009. 9:657–660.
25. Tan JC, Ho B, Busque S, Blouch K, Derby G, Efron B, et al. Imprecision of creatinine-based GFR estimates in uninephric kidney donors. Clin J Am Soc Nephrol. 2010. 5:497–502.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download