Abstract
Purpose
The purpose of this study was to investigate the risk factors for urethrocutaneous fistula development after hypospadias repair.
Materials and Methods
Between January 1990 and May 2010, 348 patients underwent hypospadias repair. This study included 294 patients who were followed up for more than 6 months. Potential risk factors for the development of fistula after operation included age, location of hypospadias, type of hypospadias repair, suture materials and methods, methods and duration of catheterization, combined congenital urologic disorders, timing of presentation and repair of fistula, and location of fistula. Data were analyzed retrospectively. Binary logistic regression analysis was used for univariate and multivariate analysis.
Results
Out of 294 patients, 63 patients (21.4%, 63/294) developed urethrocutaneous fistulas after hypospadias repair. In the univariate analysis, fistula formation was statistically related with type of hypospadias and type of hypospadias repair. In the multivariate analysis with stratification by hypospadias site, however, only the location of hypospadias was a significant independent risk factor in urethrocutaneous fistula development after hypospadias repair (p<0.001).
Conclusions
Our results suggest that the risk of developing urethrocutaneous fistula after hypospadias repair is associated with the location of hypospadias (more proximal-type hypospadias). Type of hypospadias repair, suture materials, suture techniques, and number of other combined urologic disorders were not related to the development of urethrocutaneous fistulas.
Urethrocutaneous fistulas after hypospadias repair remain a significant problem for pediatric urologists despite advances in surgical techniques. The incidence of urethrocutaneous fistula development varies from 4 to 28%. In the case of severe proximal hypospadias, two-stage hypospadias repair had previously been widely performed because of the high complication rate. Nowadays, however, with advances in surgical techniques, many pediatric urologists prefer one-stage hypospadias repair to two-stage repair [1-3]. Despite these surgical advances, complication rates after hypospadias repair remain high [2,4]. No single technique is omnipotent in all cases of urethrocutaneous fistula; thus, pediatric urologists should be familiar with a variety of reconstructive techniques. Even though urethrocutaneous fistula is very common and an important complication after hypospadias repair, few studies have been conducted to date concerning pre- and intraoperative risk factors for the development of urethrocutaneous fistula after hypospadias repair to date. The purpose of this study was to identify the perioperative risk factors for urethrocutaneous fistula development after hypospadias repair.
From January 1990 to May 2010, a period of 20 years, 348 patients underwent hypospadias repair at our urologic clinic. Of the 348 patients, 294 patients who were followed up for more than 6 months were included in this study. A mail or telephone survey was carried out for patients who did not routinely visit the clinic. Patients were divided into two groups: group A, in which urethrocutaneous fistulas occurred after hypospadias repair (63 patients, or 21.4%), and group B, in which no urethrocutaneous fistulas occurred after hypospadias repair (231 patients, or 78.6%).
Data were analyzed retrospectively according to the patients' age at the time of last follow-up, location of hypospadias (distal, middle, or proximal), type of hypospadias repair, suture materials and techniques (continuous versus interrupted, subcuticular versus full-thickness), methods and duration of catheterization after hypospadias repair, combined congenital urologic disorders, timing of presentation and repair of fistula, and number and location of fistula.
Classifications of hypospadias are based on an abnormal location of the urethral meatus and include distal (glandular, coronal, subcoronal), middle (penile), and proximal (penoscrotal, scrotal, perineal) hypospadias.
The operative methods used to repair hypospadias were tubularized incised plate urethroplasty, onlay island flap urethroplasty, Mathieu hypospadias repair, meatal advancement and glanuloplasty, and transverse preputial island flap urethroplasty. Repair of hypospadias and urethrocutaneous fistula was exclusively performed by a single surgeon in our urologic clinic.
All statistical analyses were performed by using PASW ver. 18.0 (IBM Co., Armonk, NY, USA), and p<0.05 was considered statistically significant (Student's t-test, Fisher's exact test, binary logistic regression for multivariate analysis).
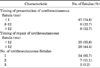
Of the 294 children who underwent hypospadias repair, 63 patients (21.4%) developed urethrocutaneous fistulas after hypospadias repair. Mean follow-up periods, mean age of the patients at the time of follow-up, and number of other congenital urologic disorders were comparable between the two groups (Table 1).
The incidence rates of urethrocutaneous fistula according to the type of hypospadias were 10.3% (19/184), 33.8% (22/65), and 48.9% (22/45) for distal, middle, and proximal hypospadias, respectively. There were significant differences in incidence rates of urethrocutaneous fistulas according to the type of hypospadias between the two groups in the univariate (p<0.001) and multivariate (p<0.001) analysis (Tables 2, 3).
The suture materials used in hypospadias repair were polyglactin 910 (Vicryl), chromicized catgut (Chromic catgut), and polydioxanone (PDS). The incidence rates of urethrocutaneous fistula according to the type of suture materials were 20.0%, 24.3%, and 24.0%, respectively. We also divided the group according to the suture technique used. The incidence rates of urethrocutaneous fistula according to suture technique I were 28.0% and 26.1% for interrupted and continuous suture methods, respectively. Rates for suture technique II were 27.3% and 27.1% for full-thickness and subcuticular suture methods, respectively. There were no significant differences in incidence rates of urethrocutaneous fistula development according to the suture material or techniques (p=0.684, p=0.538, p=0.809, respectively) (Tables 3, 4).
In the univariate analysis, fistula formation was statistically related to type of hypospadias and type of hypospadias repair. In the multivariate analysis with stratification by hypospadias site, however, only the location of hypospadias was a significant independent risk factor for urethrocutaneous fistula development after hypospadias repair (Tables 3, 4).
All children were catheterized by urethral stents and there were no cases of suprapubic cystostomy. Mean duration of urethral stenting was 11.9±3.0 and 11.1±3.2 days in groups A and B, respectively.
Of the 63 patients who developed urethrocutaneous fistulas after hypospadias repair, 47 patients (74.6%) developed urethrocutaneous fistulas within 1 month after hypospadias repair (Table 5). The longest period from hypospadias repair to development of urethrocutaneous fistula was 15 months. A total of 35 patients (55.6%) underwent repair of urethrocutaneous fistulas within 12 months after hypospadias repair (Table 5). Most of the patients (54/63, or 85.7%) had only one fistula and no patients had more than three.
Hypospadias is one of the most common congenital urologic disorders that occurs only in male infants. Although the incidence rate of hypospadias differs greatly by urologic center, studies by Carlson et al. [5] reported an incidence rate of 1 per 125 newborn infants. A recent study that analyzed a huge pool of hypospadias patients reported that the incidence of hypospadias is increasing nowadays. The direct causes of hypospadias are still unknown, but genetic and environmental factors, especially endocrine disruption, may have a crucial role in the development of hypospadias [6-9].
Hypospadias repair should be focused on three important goals: voiding in an upstanding position, proper voiding stream, and normal penile appearance that can lead to normal erection and normal sexual coitus. After the surgery, male patients should not be stressed out emotionally by hypospadias. To achieve these critical goals, it is very important that the urethral meatus be located at the end of the glans and that the penis be erected straight up during hypospadias repair.
Nowadays, pediatric surgical techniques and pediatric anesthesia skills have advanced greatly. As a result, hypospadias repair can be done at an earlier age in children. Proper timing of hypospadias repair is 6 to 24 months after birth. In this period, the children are not yet aware of their sexual identity. Most hypospadias can be corrected by single-stage hypospadias repair, but severe hypospadias can be corrected by several stages of repair at 6- to 12-month intervals.
In general, to increase the success rate of hypospadias repair, it is important that the surgeon be able to handle the tissue with the viable vessel, manipulate the tissue very exquisitely, suture without tension, and use fine suture materials and careful bleeding control. The suture material should be a very fine and absorbable thread (6-0 to 8-0 Vicryl, Chromic Catgut, PDS, Dexan). PDS is not widely used because the incidence rate of urethral stricture after hypospadias repair has been reported to be high. Suture techniques can be divided into subcuticular and full-thickness sutures, but many studies have reported that there are no significant differences between the two techniques in the development of urethrocutaneous fistula after hypospadias repair.
One of the most common complications of hypospadias repair is urethrocutaneous fistula [10]. Small-sized fistulas may disappear spontaneously, but most fistulas need surgical correction [11]. The incidence of urethrocutaneous fistula after hypospadias repair varies from surgeon to surgeon. Kass and Bolong [12] reported just 1 patient (0.48%) with fistula development out of 206 cases of hypospadias repairs. Sarhan et al. [13] reported 47 patients (9.4%) with development of fistula out of 500 cases of hypospadias repairs. According to Korean research, Kwon et al. [14] reported 42 patients (19.8%) with development of fistula out of 212 cases of hypospadias repairs and Hwang et al. [15] reported 16 patients (31.4%) with development of fistula out of 51 cases of hypospadias repairs.
Our data showed 63 patients (21.4%) with development of urethrocutaneous fistulas after hypospadias repair out of the 294 children who underwent hypospadias repair, which is considered to be average. In the univariate analysis, the type of hypospadias and the type of hypospadias repair had a statistically significant effect on outcome. However, the type of hypospadias and the type of hypospadias repair were strongly related in the cross-tabulation analysis. Thus, the analysis was carried out with stratification by location of hypospadias separately, and the results showed that no other factors had a significant impact on the outcome of the surgery.
Why patients do or do not develop urethrocutaneous fistula is not completely understood. Surgical technique is thought to be a key factor, although a local deficit in growth factors may also play a role [16]. Local or systemic, adjuvant or neoadjuvant hormonal therapy has been proposed to reduce fistula development, but the results are controversial so far. Also, some of the postoperative care including the use of particular types of dressing and surgical material, wound status, and antibiotics should be considered [17]. These postoperative factors were excluded in our study and may play an important role as risk factors; henceforth, we will need to add these factors in our follow-up studies.
There are few studies regarding perioperative risk factors for the development of urethrocutaneous fistula because there are too many variables to consider and it is quite difficult to perform the analysis. In this respect, even though our preliminary study had some limitations and pitfalls, it could be helpful to those who are planning to perform hypospadias repair. Further investigations with new study designs will be necessary to confirm our initial findings in this relatively small patient series.
Considering the incidence rate of urethrocutaneous fistula development after hypospadias repair, significantly better outcome is achieved with distal hypospadias. Our data suggest that only the type of hypospadias has a statistically significant impact on urethrocutaneous fistula development, whereas type of hypospadias repair, suture materials, and technique have no significant effect on the outcome.
Figures and Tables
TABLE 3
Multivariate analysis of risk factors for urethrocutaneous fistula development after hypospadias repair

TABLE 4
Multivariate analysis of risk factors for urethrocutaneous fistula development after hypospadias repair according to hypospadias site

Values are presented as mean±standard deviation or number (%).
Binary logistic regression analysis was used for multivariate analysis.
TIP, tubularized incised plate urethroplasty; MAGPI, meatal advancement and glanuloplasty; Mathieu, Mathieu hypospadias repair; OIF, onlay island flap urethroplasty; TPIF, transverse preputial island flap urethroplasty.
ACKNOWLEDGEMENTS
This research was supported by Kyungpook National University Research Fund, 2012 and Hankok Medical Science Foundation Fund.
References
1. Ghali AM, el-Malik EM, al-Malki T, Ibrahim AH. One-stage hypospadias repair. Experience with 544 cases. Eur Urol. 1999. 36:436–442.
2. Nuininga JE, DE Gier RP, Verschuren R, Feitz WF. Long-term outcome of different types of 1-stage hypospadias repair. J Urol. 2005. 174(4 Pt 2):1544–1548.
3. Uygur MC, Unal D, Tan MO, Germiyanoğlu C, Erol D. Factors affecting outcome of one-stage anterior hypospadias repair: analysis of 422 cases. Pediatr Surg Int. 2002. 18:142–146.
4. Demirbilek S, Kanmaz T, Aydin G, Yucesan S. Outcomes of one-stage techniques for proximal hypospadias repair. Urology. 2001. 58:267–270.
5. Carlson WH, Kisely SR, MacLellan DL. Maternal and fetal risk factors associated with severity of hypospadias: a comparison of mild and severe cases. J Pediatr Urol. 2009. 5:283–286.
6. Paulozzi LJ, Erickson JD, Jackson RJ. Hypospadias trends in two US surveillance systems. Pediatrics. 1997. 100:831–834.
7. Paulozzi LJ. International trends in rates of hypospadias and cryptorchidism. Environ Health Perspect. 1999. 107:297–302.
8. Schnack TH, Zdravkovic S, Myrup C, Westergaard T, Christensen K, Wohlfahrt J, et al. Familial aggregation of hypospadias: a cohort study. Am J Epidemiol. 2008. 167:251–256.
9. Wang MH, Baskin LS. Endocrine disruptors, genital development, and hypospadias. J Androl. 2008. 29:499–505.
10. Retik AB, Keating M, Mandell J. Complications of hypospadias repair. Urol Clin North Am. 1988. 15:223–236.
11. Waterman BJ, Renschler T, Cartwright PC, Snow BW, DeVries CR. Variables in successful repair of urethrocutaneous fistula after hypospadias surgery. J Urol. 2002. 168:726–730.
12. Kass EJ, Bolong D. Single stage hypospadias reconstruction without fistula. J Urol. 1990. 144(2 Pt 2):520–522.
13. Sarhan OM, El-Hefnawy AS, Hafez AT, Elsherbiny MT, Dawaba ME, Ghali AM. Factors affecting outcome of tubularized incised plate (TIP) urethroplasty: single-center experience with 500 cases. J Pediatr Urol. 2009. 5:378–382.
14. Kwon T, Song GH, Song K, Song C, Kim KS. Management of urethral fistulas and strictures after hypospadias repair. Korean J Urol. 2009. 50:46–50.
15. Hwang JS, Jung GW, Cho WY. Outcome of tubularized incised plate urethroplasty for correction of hypospadias. Korean J Urol. 2003. 44:1026–1031.
16. el-Galley RE, Smith E, Cohen C, Petros JA, Woodard J, Galloway NT. Epidermal growth factor (EGF) and EGF receptor in hypospadias. Br J Urol. 1997. 79:116–119.
17. Gapany C, Grasset N, Tercier S, Ramseyer P, Frey P, Meyrat BJ. A lower fistula rate in hypospadias surgery. J Pediatr Urol. 2007. 3:395–397.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download