Abstract
Bladder neck incision or transurethral incision of the prostate is a procedure described for men with bladder outflow obstruction associated with a gland size of less than 30 ml. We report a case of a man with detrusor dysfunction who was having increasing difficulty performing clean intermittent self-catheterization of the bladder. The successful use of the 120 W lithium triborate laser to perform a "mini-photoselective vaporization of the prostate" ("mini-PVP") enabled discharge of the patient on the same day as well as resolution of the patient's difficulties in performing self-catheterization. Mini-PVP has proven to be a simple and effective approach to resolution of a prostate configuration impeding the process of clean intermittent self-catheterization.
Bladder neck incision or transurethral incision of the prostate (TUIP) is a procedure described for men with bladder outflow obstruction and a gland size of less than 30 ml. Not uncommonly, a transurethral resection of the prostate (TURP) is performed instead and a mini-TURP when the occlusive median lobe is resected. Whether treated by mini-TURP or TURP, most patients undergoing this procedure require continuous bladder irrigation for 24 hours postoperatively and are discharged on the day following surgery. An uncommon indication for performing surgery is to allow for ease of self-catheterization when the configuration of the prostate interferes with this process. We report here the successful use of the 120 W lithium triborate laser to perform a "mini-photoselective vaporization of the prostate" ("mini-PVP"), which allowed for resolution of the patient's self-catheterization difficulties and discharge of the patient from the hospital on the same day.
A 75-year-old man was referred owing to difficulty in performing clean intermittent self-catheterization (CISC) of the bladder. Approximately 3 years earlier, he had been found to have chronic urinary retention and a noncontractile detrusor on urodynamic evaluation. The precise etiology behind his detrusor dysfunction has not been clarified. He had subsequently been performing CISC 4 times daily. On occasions, he reported voiding a small amount of urine between CISCs. He was otherwise in excellent health with no significant medical comorbidities. Over a period of 2 months, he described increasing difficulty in passing the catheter. He felt obstructed at the level of the bladder neck, and on occasions was unable to pass the catheter all the way into the bladder. An attempt to improve the success of CISC with the use of a Coude tip catheter was not successful.
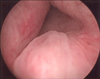
Cystoscopic examination revealed a small prostate with only slight lateral lobe protrusion. The posterior lip of the bladder neck was "high-riding" (Fig. 1).
A concavity in the posterior bladder neck is indicated by the arrow in Fig. 2. This is consistent with indentation due to the catheter striking this area "end on." The ureteric orifices were noted to be particularly close to the bladder neck. Consequently, performing a standard bladder neck incision would potentially place the orifices at risk of injury.
Using the 120 W lithium triborate laser at a setting of 80 W power, the ridge of the bladder neck tissue was vaporized at the midline. This straightened out the prostatic urethra to allow for easier catheter insertion (Fig. 3). A total of 25 kJ of energy was used, and the laser time was 4 minutes.
There was no bleeding associated with the procedure. A 16 Ch latex Foley catheter was placed at the completion of the procedure. The catheter was removed 2 hours after the procedure and the patient was discharged. The patient recommenced CISC that afternoon. There was no bleeding in the postoperative period. The catheters now pass easily and there have been no further episodes of difficult CISC. Since this procedure, the patient has observed a significantly increased level of spontaneous urethral voiding and now finds it necessary to perform ISC only twice daily.
Performing surgery for bladder outflow obstruction for reasons other than obstruction to the flow of urine is unusual. A detailed search of the literature failed to uncover a previous description of endoscopic prostate surgery being performed for the indication of difficulty in passing catheters for CISC.
In this case, there was no objective evidence that the prostate configuration was obstructive to urine flow. This would be difficult to establish in the presence of detrusor dysfunction. The prostate configuration did, however, impede the easy passage of a catheter for the purposes of CISC. This was evidenced by what was observed to be a clear indentation concavity on the surface of the "high-riding" bladder neck seen endoscopically.
This case demonstrates the efficacy of mini-PVP in the treatment of a high bladder neck. The term mini-PVP is used to describe performing a minimal PVP with only as much vaporization as necessary, and in this case the creation of an easy channel for the passage of a catheter. Other than this, there were no differences in technique or patient preparation other than that the procedure was of a short duration. Owing to the small quantity of tissue vaporized, it was possible to perform this procedure as a day case. Consequently, the patient has been minimally inconvenienced and significant inpatient treatment costs have been saved. There are few cost comparison studies between PVP and TURP, although an Australian randomized controlled trial estimated cost savings of 22% in favor of PVP [1]. However, these data were based on a 24-hour admission for PVP. Thus, day case mini-PVP would have an even greater potential cost advantage over mini-TURP. Performing a TUIP or a bladder neck incision requires similar after care as TURP, although most patients are able to be discharged home the following day [2]. This procedure differs in that an incision is primarily made at the 5 or 7 o'clock position, and given the anatomy in this particular case, could have placed these structures at risk. With PVP, the tissue was removed by vaporization rather than by being incised, which in this case enabled safe removal of the tissue in the path of catheterization in the midline.
Alternative methods of treating this patient include using a Coude tip catheter, but this approach was not successful in this patient. Coude tip catheters can make catheterization easier, and this is a popular approach after failed conventional catheterization [3].
It was of interest that the patient experienced a greater degree of spontaneous urethral voiding subsequent to surgery. This implies that despite there being detrusor dysfunction, there was probably an element of bladder outlet obstruction as well. The relief of such obstruction has favorably tipped the balance to enable voiding, although the degree of detrusor function present remains sufficient to necessitate continued CISC.
The mini-PVP approach has been demonstrated in this case to be a simple and effective approach to resolution of a prostate configuration impeding the process of CISC.
References
1. Bouchier-Hayes DM, Van Appledorn S, Bugeja P, Crowe H, Challacombe B, Costello AJ. A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int. 2010. 105:964–969.
2. Traficante A, Disabato G, Grieco A, Ditaranto G, Grande N, Vaccaro A. Transurethral incision of the prostate. Arch Ital Urol Androl. 1997. 69:Suppl 1. 81–85.
3. Villanueva C, Hemstreet GP 3rd. The approach to the difficult urethral catheterization among urology residents in the United States. Int Braz J Urol. 2010. 36:710–715.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download