This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To evaluate the efficacy and safety of the ureteroscopic management of ureteral stones immediately after a first colic attack.
Materials and Methods
We retrospectively analyzed the data of 226 patients with obstructive ureteral stones who underwent ureteroscopy with stone retrieval. The 67 patients in group A underwent ureteroscopy within 48 hours of admission to our emergency department, whereas the 159 patients in group B underwent ureteroscopy more than 48 hours after admission. The chi-square test was used to evaluate and compare stone-free status, auxiliary procedures, and complications and the Kruskal-Wallis and Fisher's exact tests were used to analyze qualitative data.
Results
Mean stone sizes in groups A and B were 2.41±1.62 mm and 4.11±2.64 mm, respectively. No patient experienced a major complication during or after the procedure. Stone-free rates were 89.55% and 89.93%, respectively.
Conclusions
Emergency ureteroscopy in cases of obstructive ureteral stones is both safe and effective and offers the advantages of immediate stone fragmentation and the relief of acute-onset colic pain.
Go to :

Keywords: Emergencies, Ureteral calculi, Ureteroscopy
INTRODUCTION
The lifetime risk of urolithiasis is estimated to be between 5% and 12% in Europe and the United States [
1]. Acute renal colic is commonly observed in emergency rooms and is usually described as an acute flank pain radiating to the groin. It is often caused by ureteral stones [
2]. Because up to 98% of ureteral calculi of <5 mm in diameter are likely to pass spontaneously, shock wave lithotripsy (SWL) and ureteroscopy (URS) have become the most common treatment modalities for stones lodged in the ureter [
3]. When drug therapy does not resolve symptoms, the next step involves the placement of a ureteral catheter or a nephrostomy tube [
1]. These simple procedures can provide prompt symptom relief, and they are usually followed by URS or SWL, which are currently the main treatment options for symptomatic ureteral stones [
4]. Although URS is a more invasive option than SWL, it probably has a better success rate, especially for mid- and distal ureteral stones [
5].
Today, consensus appears to favor the superiority of minimally invasive therapeutic procedures, but it is still debated whether SWL or URS should be the first-line treatment option for patients with ureteral stones [
6].
The recent developments of small-caliber semi-rigid and flexible deflectable ureteroscopes and of diminutive intracorporeal lithotripsy probes have made retrograde access to urinary calculi throughout the entire ureter more feasible and of lower risk [
7]. However, few data are available regarding the emergency ureteroscopic management of ureteral colic caused by ureteral stones.
In the present study, we describe our experiences with emergency ureteroscopic management of ureteral stones and compared these data with data obtained by the delayed ureteroscopic management of ureteral stones.
Go to :

MATERIALS AND METHODS
From January 2009 to June 2011, 760 patients visited the emergency department at Sanggye Paik Hospital because of renal colic caused by ureteral stones. The medical records of these patients were available for this retrospective study. All patients provided informed consent before the procedure. The study inclusion criteria were as follows: no evidence of urinary tract infection or acute renal failure. Children, pregnant women, patients with radiolucent stones or a solitary kidney, and patients with a history of ureteral stricture or multiple ureteral stones were excluded. Patients were divided into two groups according to the time when ureteroscopic management was performed. Group A consisted of patients who were hospitalized immediately at their first visit to the emergency department and underwent URS within 48 hours (n=67), and group B consisted of patients who underwent URS more than 48 hours after their first visit (n=159). All patients underwent a radiologic examination (plain X-ray, ultrasonography, non-enhanced computed tomography, or intravenous pyelography) to evaluate stone location and size. Proximal and distal ureteral stones were defined as above and below the pelvic brim, respectively, as suggested by Hollenbeck et al. [
8], and midureteral stones were defined as over the sacral bone. URS was performed under general or spinal anesthesia by use of an 8 Fr semirigid ureteroscope (Wolf). When necessary, pneumatic intracorporeal lithotripsy was performed by using the Swiss Lithoclast (EMS Medical, Nyon, Switzerland). Attempts were made to remove stone fragments with an endoscopic grasper, but small fragments (<3 mm) were largely left to pass spontaneously. At the end of the procedure, a ureteral catheter was left in place in 158 patients (69.9%) and was removed 24 hours later. In the other 68 remaining patients, a double-J stent was inserted because of significant tissue trauma (n=11, 16.2%) and edema at the impaction site (n=26, 38.2%) or suspected ureteral perforation (n=5, 7.4%), because of mild or severe dilation (n=5, 7.4%), because a large fragment was still in place (n=10, 14.7%), or because stones had been pushed back into the pyelocaliceal system (n=11, 16.2%). Mean treatment time was 37.5 minutes (range, 20 to 105 minutes). After treatment, all patients were evaluated by urinalysis, urine culture, and renal function tests. Scheduled postoperative radiologic follow-ups included plain abdominal radiography on day 1 to assess the initial stone-free rate, and for those with a stent in place, to confirm the correct stent position. At 15 to 21 days postoperatively, plain abdominal radiography was repeated before scheduled stent removal. In a few selected cases, the stent was maintained for 1 month when plain abdominal radiography was also performed. Treatment outcomes were assessed by using postprocedural stone sizes. The production of fragments of <3 mm was considered successful fragmentation and overall stone-free status was defined as the complete absence of calculus at 1 month after URS.
Cost analysis was performed by analyzing preoperative evaluation, operative, office visit, emergency department visit, and auxiliary procedure costs.
The chi-square, Kruskal-Wallis, and Fisher's exact test were used to compare group variables. The two-tailed t-test was used to assess the significance of differences between continuous variables. The analysis was performed by using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA), and statistical significance was accepted for p-values <0.05.
Go to :

RESULTS
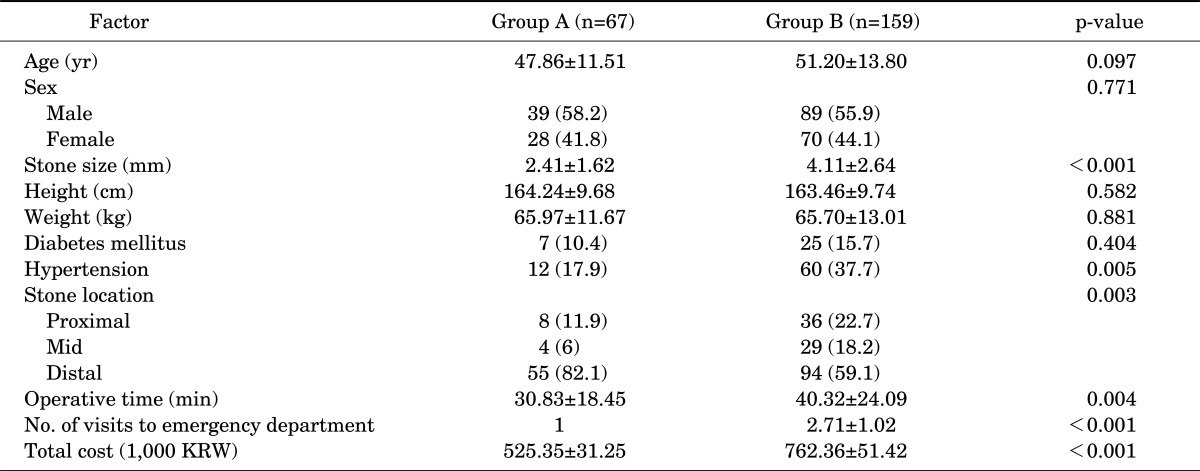
Mean patient age was 47.86±11.51 years (range, 22 to 72 years) in group A and 51.20±13.80 years (range, 14 to 82 years) in group B (p=0.097) (
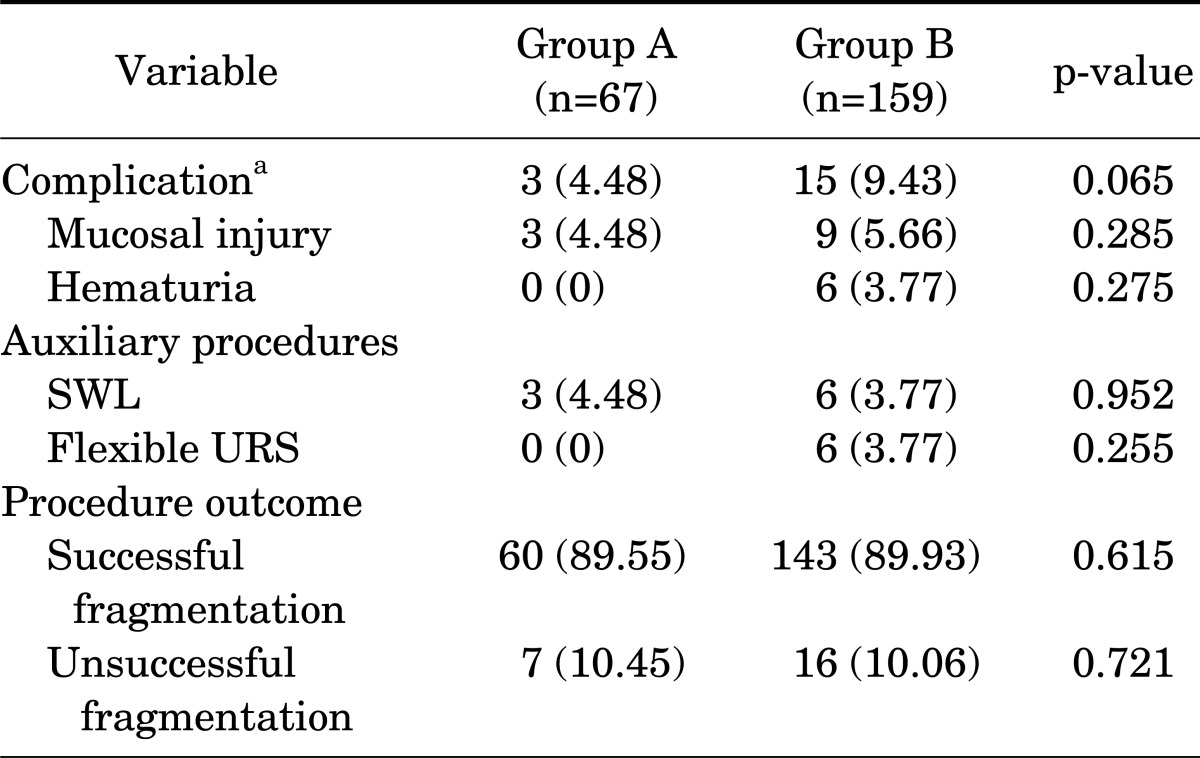
Table 1). Mean stone size was 2.41±1.62 mm in group A and 4.11±2.64 mm in group B (p<0.001), and the mean number of visits to the emergency department was 1 in group A and 2.71±1.02 in group B (p<0.001). Mean total hospital cost was 525,350±31,250 Korean Won (KRW, the currency of South Korea) in group A and 762,360±51,420 KRW in group B. With respect to intraoperative complications, no significant difference was found between the two groups (4.48% and 9.43%, respectively: p>0.05) (
Table 2). Mucosal injury was observed in 3 patients (4.48%) in group A and in 9 patients (5.66%) in group B. Hematuria, which occurred in 6 patients in group B, was considered a minor intraoperative complication (grade 1 complication according to the modified Clavien classification system [
9]) like mucosal injury. No major complications occurred in either group.
TABLE 1
Patient and stone characteristics
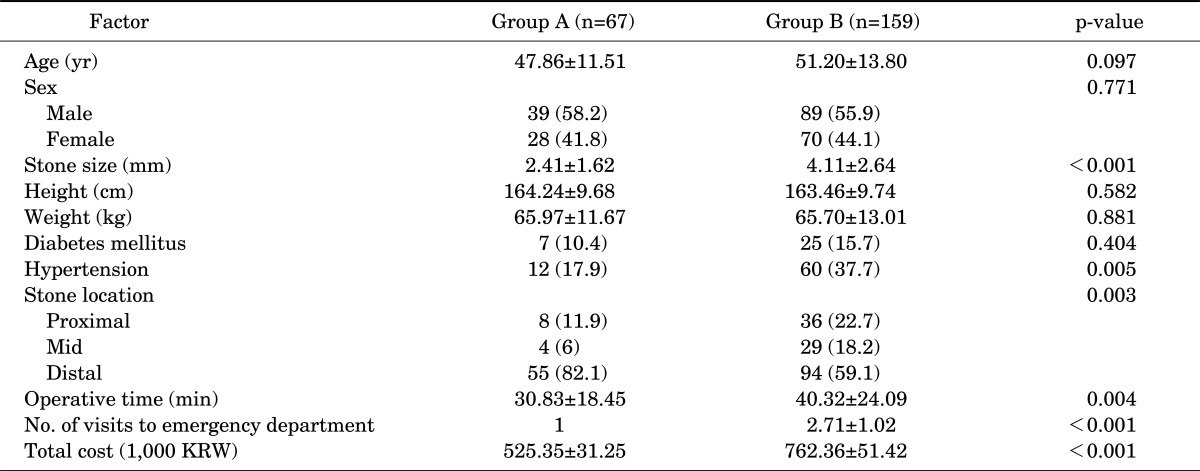

TABLE 2
Efficacies and complication rates
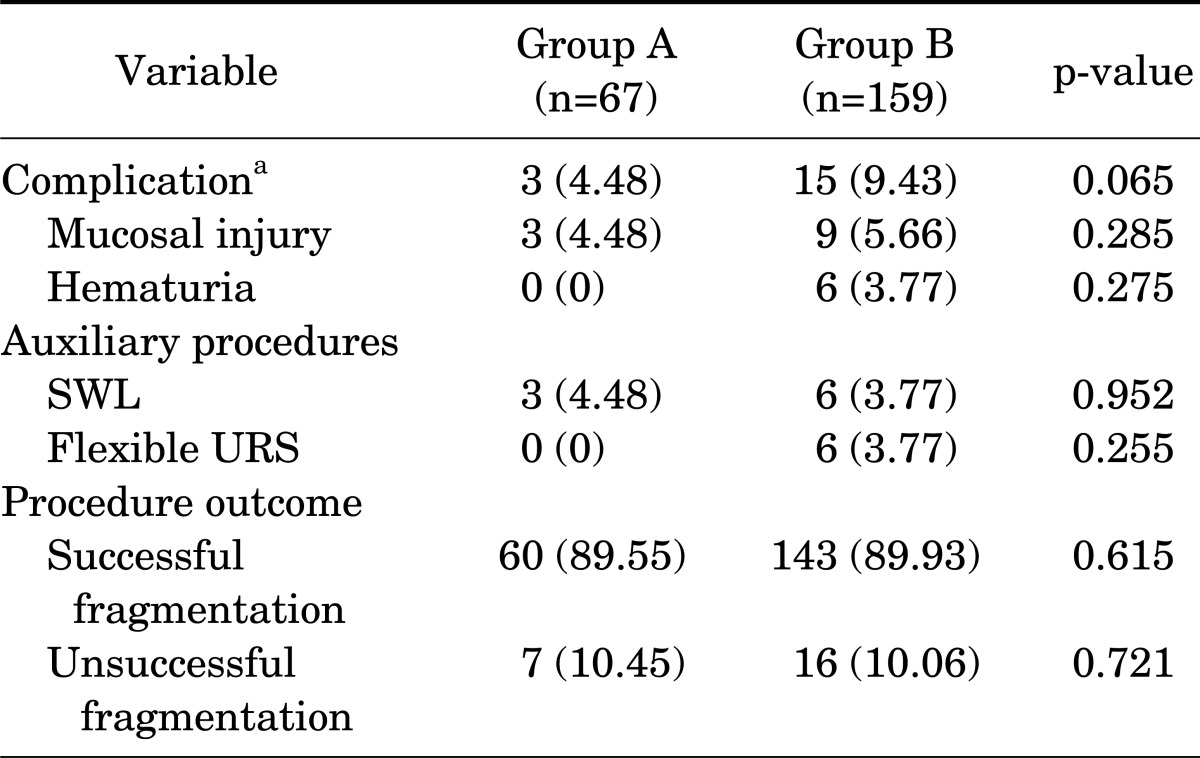

After ureteroscopic stone removal, SWL was performed to manage the remaining fragments in 3 patients (4.48%) in group A and in 6 patients (3.77%) in group B. Flexible URS was performed in 6 patients in group B. No significant difference was found between the two groups in terms of the need for additional procedures (p>0.05).
Stone-free rates were 89.55% (60 of 67) and 89.93% (143 of 159) in groups A and B, respectively. The procedure was unsuccessful in 2 patients (2.98%) in group A and in 6 patients (3.77%) in group B. Residual fragments were present in 5 patients (7.46%) in group A and in 10 patients (6.29%) in group B, and all fragments were confirmed by non-contrast spiral computed tomography after suspicious plain abdominal radiographic findings after URS.
In group A, the 2 patients (2.98%) who underwent unsuccessful URS had stones located in the proximal ureter. The underlying reason for failure was push back of calculi during pneumatic lithotripsy. In the 5 patients (7.46%) with residual fragments (>3 mm), the stones were located in the proximal ureter in 3 and in the distal ureter in 2. Mean stone size was 8.4 mm (range, 7 to 15 mm) in the 7 patients who underwent an unsuccessful procedure or who had residual fragments of >3 mm.
In group B, evaluation of the 6 patients in whom the procedure was unsuccessful showed that stone migration into the renal pelvis and severe kinking with a relatively narrowed ureteral segment preventing stone access were underlying reasons for failure during lithotripsy. Severe edema formation and bleeding due to large, impacted calculi and migration of disintegrated fragments into the renal pelvis during lithotripsy were the causes of the residual fragments in group B.
Go to :

DISCUSSION
Obstructive ureteral calculi are the most common cause of severe colic pain evaluated and treated in an emergent manner [
10]. Most ureteral stones can be reasonably expected to be uneventfully passed, and if successful, this strategy is less costly and less invasive than any other option [
11]. Ureteral stones with a diameter of less than 5 mm will pass in up to 98% of cases, but for stones with a diameter of greater than 7 mm, the overall likelihood of spontaneous passage is low [
12]. When active ureteral stone treatment is warranted, the best procedure to choose depends on several factors, such as stone size and location, operator experience, patient preference, available equipment, and related costs [
13].
Because of its noninvasive and practical nature, SWL is the preferred therapeutic option and is performed after the onset of renal colic to relieve stones and related problems [
14]. However, SWL is more successful for the management of proximal ureteral calculi and its success rates tend to decrease for distal stones and stones treated in an emergency setting. Furthermore, published data demonstrate that URS could play a major role in these selected cases [
15,
16].
URS represents a safe and minimally invasive procedure for the management of ureteral stones [
5], and technologic advancements have made it a highly successful procedure with low complication rates [
17]. Regarding the success rates of URS, the American Urological Association ureteral stones guidelines panel summary report found a stone-free rate of 56% for stones of <1 cm and a stone-free rate of 44% for stones of >1 cm in the proximal ureter as compared with rates of 89% and 73% for stones in the distal ureter, respectively [
18].
In the present study, the overall stone-free rate was 89.8% and increased to 97.6% when only stones in the distal ureter were considered. The overall complications rate was 7.96%, which decreased to 2.7% when only stones of <10 mm were considered. These results are in accordance with published data for electively scheduled URS, which ranges from 86.6 to 94.6% for all ureteral stones and from 95.6 to 100% for distal stones [
13,
15,
19,
20].
Highly effective stone fragmentation and reasonably lower complication rates have resulted in the application of emergency URS in selected cases. The possible reasons for adopting this approach are the need for prolonged anti-inflammatory and analgesic medication to prevent additional colic attacks and an expected protracted hospitalization period. However, this approach has some limitations, which include decreasing the chance of conservative management and spontaneous passage of calculi without the use of interventions that require the patient being under anesthesia [
16,
21]. Thus, it seems that, depending on stone-related and patient-related factors, preferred treatment management, that is, medical, emergency URS, or elective URS, is a matter for joint decision making by the physician and the informed patient [
10].
The findings of the present study and published data demonstrate that the removal of ureteral calculi immediately after the first colic attack should significantly decrease readmission rates to emergency departments, and thus decrease analgesic medication and economic costs originating from prolonged hospitalization and loss of work. Furthermore, our comparison of the complication rates in our two study groups showed that emergency URS can be ideal for relieving the colic pain and morbidity associated with spontaneous passage.
In addition, cost analysis showed that total charges (initial procedures, additional procedures, radiographs, postoperative office visits) were less when URS was performed emergently.
This study is limited by its retrospective nature and a relatively small cohort. However, in the absence of international guidelines regarding the ureteroscopic management of ureteral stones in an emergency setting, the results of this study suggest the need for emergency URS.
Go to :

CONCLUSIONS
Emergency URS appears to be an effective and safe procedure for the treatment of obstructive ureteral stones that provides immediate relief from colic pain and allows ureteral stones to be fragmented. In addition, emergency URS was found to be a cost-effective option. Nonetheless, it should be borne in mind that this procedure requires specific technical expertise and dedicated facilities. We recommend that an additional large-scale study that includes other parameters be conducted to confirm our findings.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download