Abstract
Purpose
The purpose of this study was to identify the necessity for professional urology treatment and the roles of urology in the treatment of inpatients referred to the urology department.
Materials and Methods
The subjects were patients referred to the department of urology among the inpatients of Chosun University Hospital from January 1, 2009, to December 31, 2011. The patients' sex and age, the referring department, and the disease group were extracted from the patients' medical records. Disease groups were classified as urination disorder, infection, tumor, calculus, trauma, pediatrics, andrology, and others. The urination disorder group was classified into the subcategories of neurogenic bladder, benign prostatic hypertrophy, urinary retention, urinary incontinence, and overactive bladder.
Results
The total number of referrals was 3,261, and males made up 54.79%. In the age distribution, 2,321 patients (71.17%) were over 60 years of age and the largest population group was patients in their 70s (32.72%). According to the department referring the patients, internal medicine (34.06%) and orthopedic surgery (16.83%) made up a high percentage. Concerning the disease group, urination disorder was the highest, being 61.26%. In the subclassification of the urination disorder group, benign prostatic hypertrophy was the highest category at 32.23%.
Conclusions
In this urology cooperative behavior analysis of our hospital over 3 years, a high percentage of older patients over 60 years of age and a high percentage of urination disorders were found. Urination disorder-related diseases in persons of advanced age are expected to increase as Korea becomes an aged society, and doctors in other departments should be aware that professional treatment and management by a urologist is needed for the treatment of these disorders.
As the expected lifespan and interest in quality of life increase, medical demands by patients increase and become segmented. Because of the westernization of diets and lifestyle, hypertension, diabetes, dyslipidemia, and obesity are increasing with age, and proactive treatment is being performed on aged patients with the development of medical technology [1,2]. Urination disorders and urinary incontinence represented by prostatic hypertrophy and its related lower urinary tract symptoms (LUTS) among old men and urination disorders represented by overactive bladder in old women are increasing remarkably, and it has been reported that these disorders are closely related to chronic diseases such as hypertension, diabetes, and metabolic syndrome [3-5]. In other words, many patients have various kinds of other diseases as well as urologic problems, and there are many patients in departments other than urology who complain of various urologic problems such as urinary retention. According to data from the Health Insurance Review & Assessment Service in 2012, there are 2 tertiary hospitals, 19 secondary hospitals, 69 primary hospitals, and 29 nursing hospitals in Gwangju. The number of urologists in those institutions are 9 in tertiary hospitals, 13 in secondary hospitals, 1 in primary hospitals, and 0 in nursing hospitals. If tertiary hospitals are excluded, 14 urologists are managing inpatients referred by doctors in other departments [6]. In particular, patients in nursing hospitals in this area may have difficulties in urologic treatment and management because of the absence of urologists, although these hospitals are presumed to have many patients with urologic problems considering the characteristics of the inpatients [7]. Accordingly, we aimed to determine the necessity of professional treatment and the role of urologists in treating inpatients by analyzing the cooperative behavior patients referred to the department of urology.
The sex, age, referring department, and disease group of the inpatients referred to the department of urology from January 1, 2009, to December 31, 2011, were extracted from the patients' medical records regardless of current or past medical history of urologic disease. The patients were divided into 10 subgroups by age and into disease groups as follows: urination disorder, infection, tumor, calculus, trauma, pediatrics, andrology, and others. The urination disorder group included neurogenic bladder, benign prostatic hypertrophy, urinary retention, urinary incontinence, and overactive bladder. The neurogenic bladder patients included patients with suspected neurogenic bladder, those with congenital or acquired disease that could induce neurogenic disorder, those with a past medical history of pelvic surgery such as radical hysterectomy or radical colectomy, and those who were diagnosed as having neurogenic bladder. Patients with urinary retention were defined as those who had difficulties in self-voiding despite enough volume of urine in the bladder or who had considerable remaining urine in the bladder in the residual urine test. Overactive bladder patients who complained of urge urinary incontinence were placed in the urinary incontinence group. For infection, not only pyuria simplex but also prostatitis was included. For tumor, not only the patients with confirmed urogenital tract tumors but also cases acquiring hematuria and those with an abnormal prostate-specific antigen level were included. In the pediatric group, all patients under 10 years of age regardless of disease were classified as pediatrics. The "others" group included cystoscope test commission to identify the pathogenesis of other departmental carcinomas, installation and removal of ureteral stents, and inquiries for urologic radiology tests.
The total number of referrals to the department of urology in our hospital was 3,261, or 1,787 males (54.79%) and 1,474 females (45.20%) by sex, showing that more male patients than female patients were referred to urology (Fig. 1). This distribution was similar yearly for the 3-year period examined.
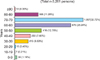
Concerning the distribution of the patients by age, there were 39 patients aged 0 to 9 years (1.19%), 7 patients aged 10 to 19 years (0.21%), 15 patients aged 20 to 29 years (0.45%), 213 patients aged 30 to 39 years (6.53%), 250 patients aged 40 to 49 years (7.66%), 416 patients aged 50 to 59 years (12.75%), 876 patients aged 60 to 69 years (25.94%), 1076 patients aged 70 to 79 years (32.72%), 368 patients aged 80 to 89 years (11.28%), and 10 patients aged 90 years or older (0.30%). A total of 2321 (71.17%) patients were 60 years or older, and the largest population age slot was patients in their 70s (Fig. 2).
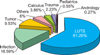
Chosun University Hospital has 24 departments in total. Referrals were made for collaborative practice from 17 departments except family medicine, occupational and environmental medicine, radiation oncology, pathology, radiology, laboratory medicine, and nuclear medicine. Of the total 3,261 cases, there were 1,111 internal medicine cases (34.06%), 549 orthopedic surgery cases (16.83%), 311 neurosurgery cases (9.53%), 268 general surgery cases (8.21%), 263 obstetrics and gynecology cases (8.06%), 207 neurology cases (6.34%), 143 thoracic and cardiovascular surgery cases (4.38%), 96 neuropsychiatry cases (2.94%), 92 rehabilitation medicine cases (2.82%), 59 plastic surgery cases (1.80%), 43 otorhinolaryngology cases (1.31%), 39 pediatrics cases (1.19%), 22 ophthalmology cases (0.67%), 20 dentistry cases (0.61%), 19 dermatology cases (0.58%), 12 emergency cases (0.36%), and 7 anesthesiology cases (0.21%) (Fig. 3). The rate of referral according to the number of all inpatients in each department for 3 years was as follows: internal medicine, 5.70%; general surgery, 4.50%; obstetrics and gynecology, 7.53%; pediatrics, 0.64%; orthopedic surgery, 8.74%; neurosurgery, 6.14%; neurology, 4.67%; thoracic and cardiovascular surgery, 12.50%; plastic surgery, 3.80%; rehabilitation medicine, 20.74%; otorhinolaryngology, 1.42%; neuropsychiatry, 8.82%; ophthalmology, 0.81%; anesthesiology, 0.71%; emergency, 1.74%; dermatology, 4.65%; and dentistry, 3.59%. When they were analyzed by year for the 3-year period, the largest portion of the patients were from internal medicine and orthopedic surgery, and the next departments showing the highest frequency were in the order of neurosurgery, general surgery, obstetrics and gynecology, and neurology.
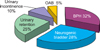
In the distribution of disease groups, LUTS occupied the highest percentage of 3,261 cases, composed of 1,998 LUTS cases (61.26%), 541 infection cases (16.59%), 311 tumor cases (9.53%), 126 calculus cases (3.86%), 73 trauma cases (2.23%), 18 pediatrics cases (0.55%), 9 andrology cases (0.27%), and 185 other cases (5.67%) (Fig. 4). When subclassifying the LUTS group, there were 644 benign prostatic hypertrophy cases (32.23%), 556 neurogenic bladder cases (27.82%), 492 urinary retention cases (24.62%), 197 urinary incontinence cases (9.85%), and 109 overactive bladder cases (5.45%) out of 1998 cases in total (Fig. 5).
Because of westernized diets and changes in lifestyle, chronic diseases such as diabetes and hypertension have increased, and there are reports that various diseases in internal medicine are related to urologic diseases. Thus, many patients with urologic problems have problems that are addressed in other departments as well. Considering the characteristics of the inpatients, many patients with chronic diseases show acute aggravation of the chronic disease or complications because of the aggravation. Such a trend is more conspicuous among aged patients, and more medication administration and operational treatments are being administered among inpatients. It is possible that there is a more obvious tendency toward these features of the inpatients in upper-scale general hospitals.
In this study, concerning the sex and age distribution of the patients, there were more male patients than female among cooperative behavior referrals and there were more patients older than 60 years of age than other age groups. The United Nations has defined a society with an aged population of 7 to 14% as an aging society, a society with an aged population of 14 to 20% as an aged society, and a society with an aged population of more than 20% as an ultra-aged society [8]. According to the Statistics Office, Korea has already entered into an aging society, with 9.1% of the population aged over 65, and it is expected to enter into an aged society in 2018 and an ultra-aged society in 2026 [9]. According to Lee et al. [10] regarding the prevalence of overactive bladder, urinary incontinence, and LUTS, more males over the age of 50 show LUTS than females and the occurrence of LUTS in males increases with age. Such LUTS in males are caused by benign prostatic hypertrophy, which is prevalent in aged males. It is known that 40 to 70% of males over 60 have benign prostatic hypertrophy symptoms in Western reports [11,12]. The prevalence of benign prostatic hyperplasia increases from approximately 50% at 60 years of age to 90% in men older than 85 years [13].
Looking into the departmental distribution, it was in the descending order of internal medicine, orthopedic surgery, neurosurgery, general surgery, obstetrics and gynecology, and neurology. Of these departments, the internal medicine department recorded 34% of referrals in the 3 years studied. The most common chronic diseases that the patients in internal medicine have are diabetes and hypertension. In particular, metabolic syndrome is defined when diseases such as hypertension, diabetes, dyslipidemia, and obesity causing coronary artery disease are shown together [14]. It is known that the basic pathophysiology of metabolic syndrome may cause LUTS because of secondary hyperinsulinemia owing to insulin resistance and overactivation of the sympathetic system [15], and abdominal fat is related to prostatic hypertrophy [16]. Additionally, urinary symptoms in the patients with obesity and diabetes may be aggravated because of more frequent urinary tract infections owing to decreased immunity. Obesity and diabetes may cause LUTS and erectile malfunction because of the dysfunction of vascular endothelial cells [17,18]. Additionally, because of the aggravated base diseases in internal medicine, LUTS can occur because of dementia or delirium. Furthermore, various medications, such as hypertension-preventive calcium channel blockers, nasal decongestant α-adrenergic agonists, diuretic and nonsteroidal anti-inflammatory drugs for congestive heart failure, angiotensin converting enzyme inhibitors, and anticholinergics, can cause LUTS [19].
In departments where operations for nongenitourinary diseases take place, such as orthopedic surgery, neurosurgery, general surgery, and obstetrics and gynecology, urination disorders are reported in 4 to 25% of cases after an operation using general anesthesia or spinal anesthesia [20]. According to the type of operation, the occurrence of voiding dysfunction after the operation was 26% in laparotomy, 14% in herniotomy, 30% in laparocholecystotomy [21-23], and 28% in total hip reconstruction and total knee reconstruction [24]. In this study, compared with the other surgery departments, the rate of referrals was high in orthopedic surgery. This may be because there were more inpatients in orthopedic surgery than in other departments and that disorders in walking were caused after the operations.
When looking into the distribution by disease, urination disorder was the highest, with a rate of 61.26%. Among urination disorder diseases, they were in the descending order of benign prostatic hypertrophy, neurogenic bladder, urinary retention, urinary incontinence, and overactive bladder. Urinary retention may easily occur in older populations because they have retarded renal function, thus concentrating the urine; reduced contraction power of the bladder; difficulties in mobility because of failed joints; changes in cognitive processes; lost integrity of the nervous system; and obstruction disease such as benign prostatic hypertrophy and uterus or bladder prolapse [25]. Additionally, with the lengthened hours of the operation, the amount of anesthetic and narcotic analgesic administered to the patient increases and the hydration solution amount also increases. Therefore, urinary retention may occur more easily [21]. This mainly happens in perineum, gynecology, and anal surgery. Urinary retention occurring after surgery may be temporary. However, urinary retention can be related to inappropriate management or lack of management of urologic problems. Additional agents used after the operation can also cause problems in urination; therefore, these patients need continuous referral to urology.
In the urinary incontinence prevalence survey of the general public in Korea, the overall prevalence rate was 41.2% [26] and the rate of urinary incontinence in this study was 9.85%. According to Shin et al. [7] study regarding the prevalence rate and management status of urinary incontinence among the inpatients of nursing hospitals in Busan, the reasons for admittance to a nursing hospital included cerebral vascular disease (33.8%), senile infirmity (20.3%), dementia (16.4%), immobilization (10.3%), chronic wasting disease (9.8%), and other diseases including Parkinson's disease (9.4%). The prevalence rate of urinary incontinence was 48.1%, and most of the patients managed urinary incontinence by use of diapers. Complications were reported as cutaneous disorders in the inguinal region and perineum, eczema, and decubitus.
It is generally thought that uncomplicated urinary tract infections can occur easily and are harmless because they can be cured with the administration of antibiotics. However, in the case of complicated urinary tract infections, ranging from cystitis to sepsis accompanying shock, the strain would be most frequently enterobacteria such as Escherichia coli. Compared with uncomplicated urinary tract infections, the causative strains of complicated urinary tract infections are much more various with high antibiotic resistance [27]. According to the clinical guidance of the European Urology Association, factors suggesting complicated urinary tract infections are male sex, elderly age, hospital-acquired infection, pregnancy, indwelling urinary catheter, diabetes mellitus, immunosuppression, and recent antimicrobial use [28]. Patients in the hospital frequently show fragile physiques with a high level of accompanying diseases; thus, the occurrence of infections would have more serious results. Accordingly, it is important to prevent urinary tract infections in patients in the hospital and to treat such infections early. Indiscreet use of catheters, one of the most important causes, and unnecessary long-time custody should be avoided. Also, in the case of elderly patients with diseases that may cause dysuria, such as neurogenic bladder and benign prostatic hypertrophy, the occurrence of urinary tract infections may be increased; thus, management with regard to such infections should be given due consideration.
In this study, there were 69 primary hospitals in Gwangju, only one of which had a department of urology, although most of them had internal medicine, orthopedic surgery, neurosurgery, and general surgery. When we examined the collaborative practice cases referred to the department of urology in Chosun University Hospital, we found that most of the referrals were made by internal medicine, orthopedic surgery, neurosurgery, and general surgery, and the most frequent disease was urination disorder. It is possible that the urination disorder, urinary tract infection, and erectile dysfunction that are frequent complaints of inpatients, and the urination disorder after operations for non-genitourinary diseases, could be prevented with the interest and attention of the doctors in other departments and that these disorders are not treated in their early stages because of the absence of a urologist. As the society ages, more and more people use medical services such as nursing hospitals, but urination disorder and its complications are not properly treated because of the absence of urologists. Efforts should be made to improve the quality of life of the patients by administrating proper methods and education.
In this analysis of the cooperative behavior in our hospital over a 3-year period, older patients over the age of 60 with urination disorder occupied a high percentage of the cooperative behavior cases. In the future when Korea becomes an aged society, it is expected that urination disorder-related diseases in advanced age will increase and doctors in other departments should be aware that the professional treatment and management of these disorders by a urologist is needed.
Figures and Tables
FIG. 1
Distribution of the sex of the patients referred to the department of urology over 3 years (n=3,261).

FIG. 3
Distribution of departments making referrals to the department of urology over 3 years. IM, internal medicine; OS, orthopedics; NS, neurosurgery; GS, general surgery; OBGY, obstetrics and gynecology; NE, department of neurology; CS, thoracic and cardiovascular surgery; NP, neuropsychiatry; RE, rehabilitation medicine; PS, plastic surgery; ENT, otorhinolaryngology; PD, pediatrics; Others, ophthalmology, dentistry, dermatology, emergency medicine, and anesthesiology.
References
1. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998. 97:1837–1847.
2. 27th Bethesda Conference. Matching the Intensity of Risk Factor Management with the Hazard for Coronary Disease Events. September 14-15, 1995. J Am Coll Cardiol. 1996. 27:957–1047.
3. Boon TA, Van Venrooij GE, Eckhardt MD. Effect of diabetes mellitus on lower urinary tract symptoms and dysfunction in patients with benign prostatic hyperplasia. Curr Urol Rep. 2001. 2:297–301.
4. Michel MC, Heemann U, Schumacher H, Mehlburger L, Goepel M. Association of hypertension with symptoms of benign prostatic hyperplasia. J Urol. 2004. 172(4 Pt 1):1390–1393.
5. Hammarsten J, Högstedt B, Holthuis N, Mellström D. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998. 1:157–162.
6. Health Insurance Review & Assessment Service [Internet]. c2011. cited 2012 Feb 23. Seoul: Health Insurance Review & Assessment Service;Available from: http://www.hira.or.kr/main.do.
7. Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean J Urol. 2009. 50:450–456.
8. Korea National Statistical Office. Population projections for Korea. 2006. Seoul: Korean National Statistical Office.
9. Korean Ministry of Health and Welfare. Yearbook on health and welfare statistics. 2007. 53rd ed. Seoul: Korean Ministry of Health and Welfare.
10. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011. 29:185–190.
11. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.
12. Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet. 1991. 338:469–471.
13. Yoo TK, Cho HJ. Benign prostatic hyperplasia: from bench to clinic. Korean J Urol. 2012. 53:139–148.
14. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.
15. Hammarsten J, Högstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001. 39:151–158.
16. Matsuda T, Abe H, Suda K. Relation between benign prostatic hyperplasia and obesity and estrogen. Rinsho Byori. 2004. 52:291–294.
17. Hoepelman AI, Meiland R, Geerlings SE. Pathogenesis and management of bacterial urinary tract infections in adult patients with diabetes mellitus. Int J Antimicrob Agents. 2003. 22:Suppl 2. 35–43.
18. Giugliano F, Esposito K, Di Palo C, Ciotola M, Giugliano G, Marfella R, et al. Erectile dysfunction associates with endothelial dysfunction and raised proinflammatory cytokine levels in obese men. J Endocrinol Invest. 2004. 27:665–669.
19. Neil M. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Geriatric incontinence and voiding dysfunction. Campbell-Walsh Urology. 2011. 10th edition. Philadelphia: Saunders;2206–2207.
20. Wein AJ. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Lower urinary tract dysfunction in neurologic injury and disease. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;2040–2041.
21. Petros JG, Rimm EB, Robillard RJ. Factors influencing urinary tract retention after elective open cholecystectomy. Surg Gynecol Obstet. 1992. 174:497–500.
22. Stallard S, Prescott S. Postoperative urinary retention in general surgical patients. Br J Surg. 1988. 75:1141–1143.
23. Kwon MI, Kim KM, Kim KW, Kim BK, Kim SY, Kim SD, et al. Anesthesiology. 2005. 3rd ed. Seoul: Ryomoongak.
24. Hozack WJ, Carpiniello V, Booth RE Jr. The effect of early bladder catheterization on the incidence of urinary complications after total joint replacement. Clin Orthop Relat Res. 1988. (231):79–82.
25. Wren KR, Wren TL. Postsurgical urinary retention. Urol Nurs. 1996. 16:45–47.
26. Oh SJ, Park WH, Park CH, Paick JS, Seo JT, Lee YS, et al. Prevalence of urinary incontinence and incontinence-related quality of life in Korean women: a Population-based Study. J Korean Continence Soc. 2003. 7:73–80.
27. Cho YH. Introduction to urinary tract infections. Korean J Urol. 2006. 47:559–567.
28. Naber KG, Bishop MC, Bjerklund-Johansen TE, Botto H, Cek M, Grabe M, et al. European Association of Urology. The management of urinary and male genital tract infections. European Association of Urology Guidelines. 2006. Arnhem: Drukkerij Gelderland;1–126.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download