Abstract
Purpose
We aimed to analyze the changes in kidney function during the postoperative early period caused by the application of percutaneous nephrolithotomy (PNL), which is commonly used in kidney stone surgery.
Materials and Methods
PNL was performed in 80 patients (48 men, 32 women) with kidney stones. The mean age of the patients was 43.71 years (range, 18 to 71 years). Preoperative and postoperative values for stone size, glomerular filtration rate (GFR), serum creatinine, urea, electrolytes (Na, K, Cl), and Hb were compared in 80 patients in whom PNL surgery was performed. The formula of Cockroft-Gault was used to calculate the GFR during the early postoperative period (72 to 96 hours).
Results
Statistically significant decreases after PNL were observed in average stone size (preoperative, 627.75±375.10 mm2; postoperative, 81.70±16.15 mm2), serum urea (preoperative, 38.40±17.26 mg/dl; postoperative, 33.28±16.98 mg/dl), and creatinine (preoperative, 1.03±0.53 mg/dl; postoperative, 0.97±0.55 mg/dl) and an increase was observed in GFR (preoperative, 104.30±37.30 ml/min; postoperative, 112.38±40.1 ml/min). No changes were detected in the serum electrolyte values (Na, K, Cl). Multiple access, operation time, and type of lithotripter did not have any significant effects on the change in the GFR.
Urinary system stone disease, which has affected humankind since the early ages and is endemic in our country, constitutes an important part of daily urology application. It has been reported that the risk of encountering stone disease at any stage of the human lifespan varies between 1% and 15% [1].
Endoscopic kidney stone surgery is one of the greatest and most important developments in urology practices over the past 50 years. These surgical developments began with the description of endoscopic procedural methods that cause the least damage to the kidney. Percutaneous nephrolithotomy (PNL) is the most important and commonly used of these endoscopic procedural methods [2].
In several studies, it was shown that PNL does not cause permanent renal damage or that the damage is negligible [3,4]. The number of studies showing changes in kidney functions in the early period after PNL is limited. In the studies done for this purpose in which changes in the glomerular filtration rate (GFR) were evaluated during the early postoperative period, a decrease and then an increase in the GFR was observed during the 24 to 48 hours following tract dilatation after PNL [5]. It is thought that knowledge of the changes that can develop in kidney function after PNL during the early period may act as a guide during postoperative follow-up, especially when managing those at risk and in the selection of drugs.
In our study, we aimed to analyze the changes in kidney function during the early postoperative period caused by the application of PNL, which is commonly used in kidney stone surgery.
This prospective study, having the approval of the local ethics committee, was performed in 80 patients who were referred to our clinic for kidney stones and who underwent PNL. All patients completed the informed consent form before the study
Urine cultures were taken from all patients before the surgery. Antibiotic therapy was given to patients with urinary infection according to the results of the urine culture, and the operation was planned after sterilization of the urine. Standard laboratory methods were performed on all patients for preoperative hemogram, serum biochemistry examinations (creatinine, urea, Na, K, Cl), bleeding and coagulation time examinations, and hepatitis markers. The body weights of all patients were recorded. Kidney-ureter-bladder imaging and unenhanced abdominal computed tomography were performed in all patients before the operation.
The two diameters of the stones were multiplied and the stone size was calculated as mm2 in the preoperative kidney-ureter-bladder image of each case. The GFR was calculated by using the formula of Cockroft-Gault, as follows: GFR=(140-age)×body weight/serum creatinine×72. In female patients, the formula was multiplied by a constant of 0.85.
Ceftriaxone 1 g intramuscular/intravenous was given to all patients on the morning of the operation day preoperatively. Administering nephrotoxic drugs before and after the operation was avoided. The number of renal access points, type of lithotripter, operation and scope times, the amount of irrigation fluid, and the blood transfusion during the preoperative and postoperative periods were recorded during PNL surgery.
All patients were evaluated by kidney-ureter-bladder imaging or unenhanced computerized tomography (for patients with nonopaque stones) in terms of residue stones during the postoperative early period. The size of residual stones was calculated as mm2.
The nephrostomy tube was removed after nephrostography was performed between the 48th and 72nd postoperative hours when hematuria ceased, the urine became discolored, and intravenous saline and drugs had stopped being administered. Then, the changes in the kidney function of the patients were analyzed according to the GFR measured by the Cockroft-Gault formula during the early postoperative period (72 to 96 hours).
The patients were anesthetized in the supine position. In the lithotomy position, a 5 Fr or 6 Fr open-ended ureteral catheter was placed at the kidney ureteral orifice where the stone was located. Then, the patient was put into the prone position. The pelvicaliceal system was monitored by use of C-arm fluoroscopy (Philips BV 29) by injecting radio-opaque material or air from the ureteral catheter. A 19-gauge percutaneous syringe was used to enter the proper calyx under fluoroscopy. Attempts were made to insert the guide wire (Sensor Guide Wire, 0.038, Boston Scientific Co., Natick, MA, USA) into the ureter within the syringe. The entry point of the kidney was widened to 28 Fr or 30 Fr by gradually passing the dilator set materials (Amplatz Renal Dilatator Set; Marflow AG, Zürich, Switzerland) over the guide wire. A 26 Fr (Karl Storz Gmbh & Co. KG, Tuttlingen, Germany) or 24 Fr (Richard Wolf Gmbh, Knittlingen, Germany) rigid nephroscope was used for endoscopic monitoring of the kidney. According to its size, the stone was only extracted by stone-grasping forceps (Grasping Forceps, Karl Storz Gmbh & Co. KG) or was removed with forceps by breaking the stone with a pneumatic, ultrasonic, or combined lithotripter (Swiss Lithoclast, E.M.S. Electro Medical Systems SA, Nyon, Switzerland). A 20 Fr Foley nephrostomy tube was placed after completion of the operation and the nephrostography was checked by injecting opaque material from the Foley catheter.
Chi-square analysis and Pearson's coefficient of correlation were used to determine the relationship between the levels of two categorical variables and the linear relationship between continuous variables, respectively. The Shapiro Wilks test was applied to determine the relevance of a normal distribution. The Student's t-test or Mann Whitney U test was used to compare the two independent groups, and analysis of variance or the Kruskal Wallis test was used to compare more than two independent groups. In addition, the Dunn test was used for multiple comparisons. Mean±standard deviation, frequency, and percentage values are given as descriptive statistics. SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA) was used for the analyses and p<0.05 was accepted as significant.
A total of 48 patients (60%) were men and 32 (40%) were women. The mean age of the patients was 43.71±13.63 years (range, 18 to 71 years). The stones were found in the right kidneys of 38 patients (47.5%) and in the left kidneys of 42 patients (52.5%). The average preoperative stone size of 80 patients who underwent PNL surgery was 627.75±375.10 mm2 and the average postoperative stone size was 81.70±16.15 mm2 (p=0.001).
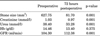
The average preoperative serum creatinine was 1.03±0.53 mg/dl and the average postoperative serum creatinine was 0.97±0.55 mg/dl (p=0.001). The average preoperative serum urea value was 38.40±17.26 mg/dl and the average postoperative serum urea value was 33.28±16.98 mg/dl (p=0.001). The average preoperative GFR was 104.30±37.30 ml/min and the average postoperative GFR was 112.38±40.1 ml/min (p=0.001). These changes were found to be statistically significant (Table 1).
The average preoperative serum Hb value of the patients was 14.46±1.66 g/dl and the average postoperative serum Hb value was 13.40±10.7 g/dl. The decrease in Hb value was not found to be statistically significant (p=0.375). No statistically significant differences in preoperative or postoperative serum Na, K, or Cl of the patients were observed.
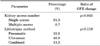
A total of 61 of the 80 patients (76.25%) were found to be stone free, whereas residual stones were detected in 19 patients (23.75%). The average operation time of the cases was 94.50±36.60 minutes, the average scope time was 82.19±53.67 seconds and the average amount of used irrigation fluid was 13.05±6.26 l (Table 2). Operation time had no significant effect on change in the GFR (r=0.091, p=0.432).
Single access was performed on 73 of 80 patients (91.3%) and multiple accesses were performed on 7 patients (8.7%). No significant difference in GFR between the patients who underwent PNL with a single access and those with multiple accesses was observed (p=0.845). In terms of lithotripter use, a pneumatic lithotripter was used on 26 patients (32.5%) and an ultrasonic lithotripter was used on 39 patients (48.8%). In addition, a combined lithotripter was used on nine patients (11.3%). No lithotripter was used on six of the patients (7.5%). No significant differences between the lithotripter used and GFR change rates were observed (p=0.119) (Table 3).
D-J catheter implantation was performed in 4 patients (5%) owing to prolonged urine leakage. A-V fistula was detected in two patients with postoperative hematuria and was controlled by embolization. Nephrectomy was performed in one patient who developed pyonephrosis due to unsuccessful access and the patient was excluded from the study. Three patients with postoperative fever and infection were treated with parenteral antibiotic therapy.
The aim of treatment of urinary system stone disease is to attain overachievement with the least kidney damage. Therefore, PNL is preferred to open surgery nowadays owing to these advantages: short length of hospital stay, low cost of treatment, a return to work in the postoperative period, and the absence of cosmetic disorders resulting from an incision scar [6].
Evaluation of renal parenchymal damage after PNL is important for determining the modality of renal stone treatment. It is more significant in patients with a solitary kidney. In the study carried out by Liou and Streem [3], extracorporeal shock wave lithotripsy was applied to 53 patients with a solitary kidney and PNL was applied to 18 patients. In addition, both techniques were carried out for 12 patients. It was determined that there was no significant disruption in GFRs or serum creatinine levels in these three groups during a 2-year follow-up. In a similar study carried out by Canes et al. [7], 81 patients with a solitary kidney who underwent percutaneous surgery showed recovery in GFR values by the end of 1 year.
Marberger et al. [8] evaluated PNL cases with computerized tomography and Tc-99m dimercaptosuccinic acid (DMSA) scintigraphy during the postoperative period. According to the results of the computerized tomography, thickening in the kidney cap, subcapsular hematoma, and thicknening in the perirenal tissue were detected at the area obedient to the nephrostomy tract. DMSA scintigraphy was evaluated as normal. Although scar tissue was observed at computed tomography, no changes were detected in the scintigraphy results of the patients. In a similar study with scintigraphy carried out by Moskovitz et al. [9], no disruption was observed in total renal function, whereas damage was detected in the operation site after PNL.
Most of the studies showed changes in kidney functions due to PNL during the late period. The number of studies reporting changes in the GFR in the early period is quite limited. In a study on pigs carried out by Handa et al. [10], decreases in the GFR, renal plasma flow, and renal excretory functions were observed in the first few hours after unilateral percutaneous renal tract dilation.
In the study performed by Nouralizadeh et al.[5], PNL was applied to 94 patients and the effects of PNL on early period kidney functions were determined. The GFR was calculated with the Cockroft-Gault formula at 6, 24, 48, and 72 hours before and after surgery. Whereas a decrease in GFR values was detected up to 48 hours after surgery, an increase was observed in GFR values calculated at 72 hours, and no significant differences were observed between them and the values before surgery. It was emphasized that the GFR may be normalized at 3 to 14 days after PNL. It was indicated that the decrease in the GFR up to 48 hours after surgery could be due to the drugs used during and after surgery and the contrast material. In our study, the mean preoperative GFR was 104.30±37.30 ml/min and the mean postoperative GFR was 112.38±40.1 ml/min and the increase was statistically significant. The increase in GFR at 72 hours postoperatively supports the previous study.
It is possible that kidney dilation performed for access to the pyelocaliceal system during PNL surgery can have negative effects on kidney function owing to the invasive nature of kidney dilation. In the study carried out by Handa et al. [11], single access and multiple accesses were applied to different groups of patients. No significant differences were observed in kidney functions between these two groups. In our study, single access was applied to 73 patients (91.3%) and multiple accesses were applied to 7 patients (8.8%). No significant differences were observed in the GFR between these two groups (p=0.845).
Owing to its invasive nature, PNL can cause disruption in kidney function depending on kidney parenchymal damage. In parallel with other studies, the results of our study showed a significant recovery in the GFR instead of disruption in the early period after PNL. This recovery may have been due to the removal of stone weight, which is the primary reason for obstruction in the kidney and for kidney function disorder. Also, it was observed that kidney dilatation during PNL operation and multiple accesses had no negative effects on kidney function. In addition, operation time and lithotripter type had no significant effects on GFR change.
Figures and Tables
TABLE 1
Comparison of the values of average stone size, serum creatinine, urea, electrolytes, hb, and GFR before and after PNL surgery
References
1. Pearle MS, Lotan Y. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Urinary lithiasis: etiology, epidemiology, and pathogenesis. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders Company;1386–1387.
2. Fernstrom I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976. 10:257–259.
3. Liou LS, Streem SB. Long-term renal functional effects of shock wave lithotripsy, percutaneous nephrolithotomy and combination therapy: a comparative study of patients with solitary kidney. J Urol. 2001. 166:36.
4. Parsons JK, Jarrett TW, Lancini V, Kavoussi LR. Infundibular stenosis after percutaneous nephrolithotomy. J Urol. 2002. 167:35–38.
5. Nouralizadeh A, Sichani MM, Kashi AH. Impacts of percutaneous nephrolithotomy on the estimated glomerular filtration rate during the first few days after surgery. Urol Res. 2011. 39:129–133.
6. Aridogan IA, Bayazit Y. Percutaneous surgery in renal stone disease. Turkiye Klinikleri J Urol-Spec Top. 2009. 2:66–70.
7. Canes D, Hegarty NJ, Kamoi K, Haber GP, Berger A, Aron M, et al. Functional outcomes following percutaneous surgery in the solitary kidney. J Urol. 2009. 181:154–160.
8. Marberger M, Stackl W, Hruby W, Kroiss A. Late sequelae of ultrasonic lithotripsy of renal calculi. J Urol. 1985. 133:170–173.
9. Moskovitz B, Halachmi S, Sopov V, Burbara J, Horev N, Groshar D, et al. Effect of percutaneous nephrolithotripsy on renal function: assessment with quantitative SPECT of (99m)Tc-DMSA renal scintigraphy. J Endourol. 2006. 20:102–106.
10. Handa RK, Matlaga BR, Connors BA, Ying J, Paterson RF, Kuo RL, et al. Acute effects of percutaneous tract dilation on renal function and structure. J Endourol. 2006. 20:1030–1040.
11. Handa RK, Evan AP, Willis LR, Johnson CD, Connors BA, Gao S, et al. Renal functional effects of multiple-tract percutaneous access. J Endourol. 2009. 23:1951–1956.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download