Abstract
One of the annoying complications of radical prostatectomy is urinary incontinence. Post-prostatectomy incontinence (PPI) causes a significant impact on the patient's health-related quality of life. Although PPI is stress urinary incontinence caused by intrinsic sphincter deficiency in most cases, bladder dysfunction and vesicourethral anastomotic stenosis can induce urine leakage also. Exact clinical assessments, such as a voiding diary, incontinence questionnaire, pad test, urodynamic study, and urethrocystoscopy, are necessary to determine adequate treatment. The initial management of PPI is conservative treatment including lifestyle interventions, pelvic floor muscle training with or without biofeedback, and bladder training. An early start of conservative treatment is recommended during the first year. If the conservative treatment fails, surgical treatment is recommended. Surgical treatment of stress urinary incontinence after radical prostatectomy can be divided into minimally invasive and invasive treatments. Minimally invasive treatment includes injection of urethral bulking agents, male suburethral sling, and adjustable continence balloons. Invasive treatment includes artificial urinary sphincter implantation, which is still the gold standard and the most effective treatment of PPI. However, the demand for minimally invasive treatment is increasing, and many urologists consider male suburethral slings to be an acceptable treatment for PPI. The male sling is usually recommended for patients with persistent mild or moderate incontinence. It is necessary to improve our understanding of the pathophysiologic mechanisms of PPI and to compare different procedures for the development of new and potentially better treatment options.
Prostate-specific antigen (PSA) has been widely used throughout the world as a marker for the diagnosis of prostate cancer (PCa). The advent of PSA screening has reduced the rate of advanced PCa and has increased the detection rate of early stages of PCa [1-3]. In addition, owing to the development of minimally invasive techniques and advanced instruments for surgery, such as laparoscopy and robotic surgery, the rate of radical prostatectomy, which is the standard-of-care option for localized PCa, has surged. As a result, interest has been increasing in urinary incontinence, which is one of the most devastating complications after radical prostatectomy. The prevalence of post-prostatectomy incontinence (PPI) varies from 1 to 87% [4,5], according to the definition, timing of evaluation, surgical technique, preoperative condition of the patients, and the individual who carries out the evaluation (physician or patient). The temporal trend in the incidence of PPI is decreasing [6] as a result of improvements in surgical techniques, but the number of patients with PPI is likely to increase owing to the surge in the number of radical prostatectomy procedures performed. In addition, PPI can be associated with significant psychosocial stress and poor health-related quality of life [7,8]. The treatment options for PPI vary, according to the cause of urinary incontinence and the degree of invasiveness of management. The aim of this review is to summarize the current trends in the management of PPI.
In most cases, PPI is caused by a dysfunction of the sphincter, which can result from rhabdosphincter injury during the apical dissection; from damage caused by the placement of large, deep sutures for the vesicourethral anastomosis; or as a result of denervation caused by injury to the neurovascular bundles. Most patients with intrinsic sphincter deficiency complain of stress urinary incontinence (SUI) [9]. Bladder dysfunction, such as detrusor overactivity, impaired bladder compliance, and impaired detrusor contractility, owing to bladder denervation during surgery may also be present as the sole diagnosis or coupled with intrinsic sphincter deficiency [10]. Bladder outlet obstruction (BOO) caused by vesicourethral anastomotic stenosis can induce urine leakage or urgency incontinence as well as urinary retention [11]. Therefore, we should not overlook the fact that patients with PPI complain of not only SUI but also urgency with urgency incontinence.
Known factors affecting continence are age [12]; neurovascular bundle resection [13]; medical comorbidities, particularly diabetes mellitus [14]; body mass index [15]; prostate volume [16]; and previous radiation treatment [17]. Numerous specific surgical techniques, such as periurethral suspension, lateral prostatic fascia preservation, bladder neck preservation, and posterior urethral reconstruction, have been introduced in attempts to improve urinary continence after radical prostatectomy [18,19]. However, different results have been reported about each risk factor for PPI, and those factors are not yet well defined.
There are no clear data on the timing of the evaluation of PPI. The majority of patients complain of incontinence immediately after urethral catheter removal, but SUI after radical prostatectomy gradually improves over time [20], and many physicians first observe patients without active treatment at the beginning of SUI treatment. Most investigators agree that the time required to evaluate the exact degree of continence is at least 1 year [21]. Lepor and Kaci [22] reported a continued recovery of continence for up to 24 months postoperatively, from 80.6% at 3 months to 95.2% at 12 months and plateauing at 98.5% at 24 months. However, because PPI can be caused by bladder dysfunction or BOO and the symptoms of some patients persist beyond the first postoperative year, an early evaluation and the selection of adequate treatment for PPI can improve the patient's quality of life.
Initial clinical assessment includes taking a medical history, physical examination, postvoid residual urine, urine analysis, voiding diary, incontinence questionnaire for subjective assessment, and pad test [23]. Concerning incontinence questionnaire instruments, a simple and short questionnaire, such as the International Consultation on Incontinence Questionnaire-Short Form, which is recommended by the European Association of Urology, has been found to be useful in outpatient clinics [24]. Although a pad test is a simple test and may be a useful method for quantifying urine loss in incontinent patients, the sensitivity and specificity of the standard 1-hour pad test are not high [25], and the test could be replaced by simply asking the patients whether or not they are continent [26].
After the initial clinical assessment, noninvasive or conservative management can be started. Early noninvasive treatment has a significant positive impact on the early recovery of continence. Mariotti et al. [27] reported that the group who received a noninvasive physical treatment with biofeedback and pelvic floor electrical stimulation that began 7 days after a catheter removal showed a significantly lower urine leakage weight than did a control group. Usually, conservative management may be tried for periods of up to 6 to 12 months. If the noninvasive treatment fails, a specialized clinical assessment, such as urodynamic study (UDS) and urethrocystoscopy is indicated, especially before a surgical treatment for PPI. The accurate method for determining the cause of incontinence after prostatectomy is UDS. Urethrocystoscopy is performed to identify the vesicourethral anastomotic stenosis and anatomic position of the external sphincter.
The timing of surgical intervention for the treatment of PPI is not clear either. According to several reports, the time between prostatectomy and surgical treatment for PPI was at least 12 months, with an average of 41.5 to 52.8 months [28-31]. Some studies have evaluated the effect of early surgical intervention for PPI. Early injection (mean 23 days postoperatively) of a periurethral bulking agent showed better results than treatment at a mean of 26 months postoperatively [32]. Surgical intervention may be recommended for patients who have severe, unimproved, or continuous incontinence for 3 months at 6 months after radical prostatectomy.
Conservative or behavioral management is generally recommended during the first year after prostatectomy [33]. Pelvic floor muscle training (PFMT) is the most commonly used conservative management and is a first-line treatment that is used to restore pelvic floor or bladder function after radical prostatectomy. Treatment regimens are not yet standardized, however. Generally, PFMT is a pelvic floor muscle (PFM) contraction with various positions (lying, sitting, and standing) using tools (biofeedback, pelvic floor electrical stimulation) to increase the strength and endurance of the pelvic floor. Repeated contractions are thought to improve urinary control, through an increased support for the detrusor muscle and urethral sphincter [34]. For the accurate contraction of the PFM, the patient must learn the technique by use of specialized methods. Floratos et al. [35] reported that PFMT, using intensive verbal instructions and electromyographic biofeedback, showed objectively 91% of the overall continence rate at 6 months. If the patient did not receive instructions for PFMT, the effect was significantly lower [36]. The long-term effects of early postoperative biofeedback-PFMT are reported to be a continence rate of 96.1% among patients at postoperative month 12 [37]. In a prospective randomized controlled trial among patients with PPI for at least 1 year, PFMT with or without biofeedback and pelvic floor electrical stimulation resulted in improvement in incontinence episodes [38]. However, PFMT cannot be applied to every patient after radical prostatectomy, because patients need to be motivated and have their pelvic floor neurologically intact. Additionally, PFMT has limited benefit in patients with severe urinary incontinence. Behavioral management, such as reduction of bladder irritants, reduction of fluid intake, timed voiding, and bladder training, have also been recommended [39], but not enough evidence is available yet.
An effective pharmacologic treatment with acceptable side-effects is needed to compensate for the gap between conservative management and surgical management. Although currently there is no pharmacologic treatment approved for SUI in men, some studies of the effect of duloxetine in male SUI, which was proved to be an effective and safe treatment for women with SUI, have been reported. Duloxetine, a combined serotonin/norepinephrine reuptake inhibitor, increases the activity of the striated urethral sphincter and the effects on the excitability of pudendal motor neurons by stimulating the Onuf's nucleus [40,41]. Filocamo et al. [42] made a comparison between PFMT and duloxetine with PFMT only in the treatment of PPI and demonstrated a facilitative effect of duloxetine on early continence recovery. In a randomized, placebo-controlled, double-blind trial, which included 31 patients, 80 mg of duloxetine daily for 3 months was effective in the treatment of incontinence symptoms and improved quality of life in patients with mild to moderate PPI [43]. Larger studies investigating the efficacy and side effects of duloxetine are needed before widespread use of pharmacologic treatment.
Various substances (collagen, Teflon, silicone macroparticles, autologous fat, autologous chondrocytes, and dextranomer/hyaluronic acid copolymer) have been used for decades as bulking agents. Injection of urethral bulking agents in the urethral submucosa works by adding bulk, increasing coaptation at the level of the bladder neck and distal sphincter, and increasing the urethral lumen's resistance to flow. These are minimally invasive, cheaper treatment modalities for PPI, after conservative treatment, that do not limit future antiincontinence surgery [44]. Problems with these agents include the need for multiple injections, deterioration of effect over time, and modest success rates with low cure rates. The collagen injection success rates for PPI range from 36 to 69%, with 4 to 20% of patients reporting being dry [45-48]. Agents currently used include dextranomer/hyaluronic acid copolymer (Deflux), pyrolytic carbon microspheres (Durasphere), and polydimethylsiloxane (Macroplastique). These new agents show a slower migration without compromising the other organs, and short-term data are good. However, satisfactory long-term results required reinjections, and a high rate of complications occurred in some cases [49-51]. Bugel et al. [52] reported that Macroplastique injection showed a rapid deterioration after initial improvements, with success rates of 40% at 1 month and 26% at 12 months. Recently, autologous fibroblasts and myoblasts were introduced to reconstitute the deficient urethral sphincter, and their effects and safety have been reported [53].
Injection therapy may be useful for short-term improvement in patients with PPI who are in too poor of health for invasive surgical treatments.
Interest in the male suburethral sling procedure, which is based on the concept of passive external urethral compression, as a treatment option for PPI has been recently revived. Although long-term outcomes are unknown, the sling, which is used as a permanent material instead of a resorbable material, performs reasonably well in the intermediate term. Sling surgery is adequate for patients with mild to moderate degrees of SUI who have not had previous radiation therapy, who have adequate detrusor contractility, or who demand a less invasive procedure or a nonmechanical device, as opposed to a device such as the artificial urinary sphincter (AUS) [54]. The advantages of sling surgery compared with the AUS include no mechanical parts, no need for manual dexterity or device training, a cognitive status that enables activating and deactivating the urethral cuff, immediate efficacy, and reduced overall cost. Whereas reported revision rates owing to recurrent incontinence are quite low, longer follow-up is needed before definitive comparisons to the AUS can be made.
Several techniques for sling surgery have been introduced. Three representative sling designs, which differ in the materials used, the methods of fixation, and the position of the support, are the bone-anchored sling (BAS), the transobturator sling, and the adjustable retropubic sling.
The BAS compresses the bulbar urethra with a silicone-coated polypropylene mesh by attaching the sling to the inferior pubic rami with bone screws. The BAS improves continence by causing a degree of urethral obstruction and allowing for a better transmission of intra-abdominal pressure to the bulbar urethra [55]. The representative BAS is the InVance male sling (American Medical Systems, Minnetonka, MN, USA). The InVance sling uses a synthetic mesh positioned under the bulbar urethral via a perineal incision. It is attached to the pubic bone on both sides of the urethra by three miniature titanium screws.
Several large prospective studies have demonstrated sustained efficacy of the InVance sling with 3 to 5 years of follow-up. Carmel et al. [55] reported a case series of 45 men with PPI treated with the InVance sling. At an average of 36 months, 76% of patients were successfully treated. In a study with 42 patients, Giberti et al. [56] reported a cure rate of 62%; 8% of patients were improved, and 30% of patients had a failed treatment after an average 41 months of follow-up. Morbidity was minimal, but short-term perineal pain occurred in 16 to 19% of patients, resolving by 3 months postoperatively. Guimaraes et al. [57] reported intermediate-term results of up to 4 years with the InVance sling. Their cure rate was 65% and the improvement rate was 23% after a mean follow-up of 28 months in 62 men with PPI.
Success rates of BAS were relatively consistent in several studies, at 40 to 88%, and adverse events included acute urinary retention, infection of the perineal incision, urethral erosion, abnormal postoperative pain or paraesthesia, de novo detrusor overactivity or urinary urgency, and early loosening of one of the bone screws [58].
The effect of transobturator sling suspension for male urinary incontinence was initially reported in 2007 [59]. The retrourethral transobturator sling is passed 'outside-in' through the obturator foramen and the polypropylene mesh is sutured in place on the ventral surface of the bulbar urethra. The AdVance sling (American Medical Systems, Minnetonka, MN, USA), a kind of retrourethral transobturator sling, is designed for the relocation of the proximal urethra, under the bladder neck, with minimal extrinsic compression of the urethra. The success rate of the AdVance sling varied from 54 to 80% after 1 year of follow-up in the prospective cohort studies [60-63]. In the mid-term evaluation of the AdVance sling at a mean follow-up of 21 months, 62% of patients were cured, 16% were improved, and 22% showed no signs of improvement [64]. The investigation of urodynamic changes, which are associated with the AdVance sling, showed improvement of Valsalva leak point pressure, but the detrusor voiding pressure, postvoid residual urine volume, and maximal flow rated remained relatively unchanged [65]. A study about the complications of the AdVance sling showed that it was a safe treatment option, with the main postoperative complication being transient acute urinary retention (21.3%) and rare severe complications, such as explantation (0.9%), transection (0.4%), wound infection (0.4%), and perineal pain (0.4%) [66].
On the other hand, the inside-out transobturator male sling with polypropylene mesh (Gynemesh PS, Ethicon, Somerville, NJ, USA) has also been used for the treatment of PPI. Leruth et al. [31] reported after a median follow-up of 24 months that 49% of patients were cured, 3% were improved, and 16% were not improved.
Two adjustable sling systems: Two adjustable slings have been introduced, with the potential advantages of postoperative tightening or loosening: the REMEEX (Neomedic Inc., Terrasa, Spain) and the Argus (Promedon SA, Cordoba, Argentina).
The REMEEX system is a readjustable suburethral sling that is passed through the retropubic space; it is composed of a monofilament polypropylene mesh connected via two monofilament traction threads to a suprapubic mechanical regulator (varitensor). The regulator is a permanent subcutaneous implant over the abdominal rectus fascia, which is 2 cm above the pubis. Additionally, implant adjustment is possible, via an eternal manipulator. In a multicenter European study with 51 patients with a mean follow-up period of 32 months, 33 patients (64.7%) were cured. Twenty-five of these cured patients needed no pads; the other eight patients needed only small pads or sanitary napkins. Almost all patients needed at least one readjustment of the sling under local anesthesia. The sling had to be removed in three cases owing to urethral erosion and infection of the regulator. Intraoperative bladder perforation occurred in five patients, and mild perineal hematomas were seen in three patients. Perineal discomfort or pain was common and was treated with oral pain medication [67].
The Argus suburethral sling consists of a silicone foam pad, which is placed under the bulbar urethra (attached to the retropubically passed silicone column), and that is fixed over the rectus fascia with silicone washers. Two radiopaque silicone washers allow regulation of the desired tension. In a cohort of 48 patients with a mean follow-up of 7.5 months, Romano et al. [68] showed a cure rate of 73% and an additional 10% improvement rate. Three urethral perforations during surgery were reported, and the sling had to be removed in five patients. Seven patients had acute urinary retention, and except for one patient, in which the sling needed to be loosened, it resolved spontaneously. No severe complications were seen. Hubner et al. [69] reported 101 cases with a mean follow-up of 2.1 years. In that study, 79.2% of patients were considered to be dry, and the incontinence quality of life scale improved from a mean of 28.8 to 63.2 points after Argus sling placement. Dalpiaz et al. [70] reported mid-term complications after the placement of the Argus sling at a median follow-up of 35 months. Overall, 24 patients (83%) experienced complications, including acute urinary retention (35%) and removal of the sling (35%) owing to urethral erosion, infection, system dislocation, urinary retention, and persistent pain. Furthermore, 27% of patients complained of significant perineal pain.
Adjustable continence balloons, which are one of the most recent treatments, create passive compression of the urethra by two balloons located on either side of the urethra. The ProACT (Uromedica, Plymouth, MN, USA) is an adjustable continence therapy option and is a minimally invasive modality with a cost that is remarkably less than that of the AUS. The ProACT implantation is performed under general or spinal anesthesia through a perineal incision. The balloons are placed, one on each side of the urethra, right above the pelvic floor at the former level of the prostate after radical prostatectomy. Fluoroscopic guidance or transrectal ultrasound is used for visualization. Tubing runs from each balloon to titanium ports placed on the back of the scrotum. The balloons are filled with sterile water through these ports. At 1 month and thereafter, the balloons are refilled with 1-ml increments of this solution (maximum of 8 ml) until continence is reached. Postoperative readjustment is very simple, and only local anesthesia is necessary.
Prospective single-center study to evaluate the results of ProAct demonstrated a decrease in the median 24-hour urinary leakage (352.5 vs. 11 ml, p<0.001), a decrease in the median number of pads used per day (4.75 vs. 2.25, p=0.001), and an overall dry rate of 50% [71].
Of the 170 patients reported by Hubner and Schlarp [72], one-third became pad free. The mean number of postoperative adjustments of the balloon was 3 to 5, with some patients requiring 6 to 8 refillings. Although the success rate approximates the male sling surgery, the benefit must be weighed against the frequent need for balloon refilling and the high complication rate. The most common perioperative complications were urethral or bladder perforation, necessitating termination of the implant on the perforated side. Other complications were temporary urinary retention and device explantation as the result of balloon failure, infection, erosion, or migration. The ProACT system is not recommended for patients with prior external beam radiation therapy, because of a higher complication rate and an unsatisfactory success rate [73].
The AUS is, despite the new surgical treatment options, still the gold standard and the most effective long-term surgical treatment of male incontinence. The AUS consists of three components: the cuff, which goes around the proximal bulbar urethra; the pump, which goes inside the scrotum; and the reservoir (balloon), which holds the fluid for the device. A 4.5-cm cuff was the first cuff size, with the introduction of a 4.0-cm cuff in 1994. Currently, a 3.5-cm cuff is also available. Hudak and Morey [74] reported that the 3.5-cm cuff has become the predominant size, which is used for primary and revision AUS placement.
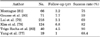
AUS has the largest body of literature reporting long-term success. The success and high patient satisfaction rates seem to outweigh the need for periodic revision, high cost, and surgical invasiveness. The success rate of the AUS procedure is still the best, when compared with that of all other available surgical treatment options for PPI. The success rates for AUS range from 59 to 90% [75-82] (Table 1). Continence rates with the AUS can vary with the definition of continence, the method of evaluation, and the length of follow-up. Nevertheless, high subjective rates of satisfaction, from 87 to 90%, are consistently reported, even without total continence [83,84].
A potential downside of the AUS is the need for periodic revisions. Revision and explantation rates, owing to mechanical failure, urethral atrophy, infection, and erosion, vary considerably among the studies, with reports of 5 to 45% and 7 to 17%, respectively [80,82]. Lai et al. [79] reported that 270 patients underwent AUS implantation, with an infection rate of 5.5%, cuff erosion rate of 6%, and an atrophy rate of 9.6%. Overall, 25% of patients required revision at 5 years. In another long-term report, Kim et al. [78] reported that 36% of patients required surgical revision or removal within 10 years, and most events occurred within the first 48 months. Revisions include replacement of the malfunctioning part, cuff replacement, repositioning or downsizing owing to urethral atrophy, and a second or tandem cuff or transcorporal cuff placement. An increased revision rate was reported for patients who received pelvic radiation but was not found in a recent series, and previous radiation therapy is therefore not a contraindication for AUS implantation [75]. AUS also showed improvement in preoperative urodynamic abnormalities in patients with PPI and concomitant urodynamic bladder dysfunction, such as detrusor overactivity, hypersensitivity, and mild loss of compliance [85].
In some patients suffering from urgency incontinence after radical prostatectomy, anticholinergic treatment is recommended as the first-line treatment for early PPI, within the first 6 to 12 months. Leach et al. [86] reported urodynamic findings in a large population of men with PPI. A total of 56% of patients had high pressure bladder dysfunction, such as detrusor overactivity and poor compliance, which contributes to the urinary incontinence. Overall treatment results demonstrated a significant decrease in pad score for men treated with anticholinergic treatment only, and 4.7% had total continence. Conservative noninvasive management, including lifestyle interventions, PFMT with or without biofeedback, and bladder training, may be helpful to improve urgency incontinence. However, the data for the conservative treatment options are much weaker for men with postprostatectomy overactive bladder and SUI than for women.
Incontinence following prostatectomy is still the most feared complication for men. Conservative therapy is recommended as an early management of PPI. If conservative therapy fails, surgical therapy options are recommended. For severe or persistent incontinence, AUS is still the gold standard of treatment and is associated with high continence and high patient satisfaction rates. In recent years, numerous minimally invasive treatment options with different success rates have been investigated. The patient demand for minimally invasive treatment options is high, and often, poorer results are accepted by the patients in order to avoid AUS. Therefore, slings can be recommended for patients with persistent mild or moderate incontinence. Also, slings can be used for patients who prefer a less invasive treatment even if the patients have severe incontinence. In the future, it will be necessary to improve our understanding of the pathophysiologic mechanisms of male PPI to develop new and potentially better treatment options.
Figures and Tables
References
1. Wu GH, Auvinen A, Yen AM, Hakama M, Tammela TL, Stenman UH, et al. The impact of interscreening interval and age on prostate cancer screening with prostate-specific antigen. Eur Urol. 2012. 61:1011–1018.
2. Djulbegovic M, Beyth RJ, Neuberger MM, Stoffs TL, Vieweg J, Djulbegovic B, et al. Screening for prostate cancer: systematic review and meta-analysis of randomised controlled trials. BMJ. 2010. 341:c4543.
3. Yoon BI, Hwang TK, Kim JC. Impact of laparoscopic radical prostatectomy on urinary incontinence and lower urinary tract symptoms. Korean J Urol. 2008. 49:134–138.
4. Kielb S, Dunn RL, Rashid MG, Murray S, Sanda MG, Montie JE, et al. Assessment of early continence recovery after radical prostatectomy: patient reported symptoms and impairment. J Urol. 2001. 166:958–961.
5. Jonler M, Madsen FA, Rhodes PR, Sall M, Messing EM, Bruskewitz RC. A prospective study of quantification of urinary incontinence and quality of life in patients undergoing radical retropubic prostatectomy. Urology. 1996. 48:433–440.
6. Sacco E, Prayer-Galetti T, Pinto F, Fracalanza S, Betto G, Pagano F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int. 2006. 97:1234–1241.
7. Penson DF, Feng Z, Kuniyuki A, McClerran D, Albertsen PC, Deapen D, et al. General quality of life 2 years following treatment for prostate cancer: what influences outcomes? Results from the prostate cancer outcomes study. J Clin Oncol. 2003. 21:1147–1154.
8. Katz G, Rodriguez R. Changes in continence and health-related quality of life after curative treatment and watchful waiting of prostate cancer. Urology. 2007. 69:1157–1160.
9. Ficazzola MA, Nitti VW. The etiology of post-radical prostatectomy incontinence and correlation of symptoms with urodynamic findings. J Urol. 1998. 160:1317–1320.
10. Porena M, Mearini E, Mearini L, Vianello A, Giannantoni A. Voiding dysfunction after radical retropubic prostatectomy: more than external urethral sphincter deficiency. Eur Urol. 2007. 52:38–45.
11. Wang R, Wood DP Jr, Hollenbeck BK, Li AY, He C, Montie JE, et al. Risk factors and quality of life for post-prostatectomy vesicourethral anastomotic stenoses. Urology. 2012. 79:449–457.
12. Nilsson AE, Schumacher MC, Johansson E, Carlsson S, Stranne J, Nyberg T, et al. Age at surgery, educational level and long-term urinary incontinence after radical prostatectomy. BJU Int. 2011. 108:1572–1577.
13. Kuehhas FE, Naegele R, Eckersberger E, Margreiter M, Herwig R, Kazzazi A, et al. Urinary continence after radical prostatectomy: the patient perspective. Can J Urol. 2011. 18:5811–5818.
14. Teber D, Sofikerim M, Ates M, Gozen AS, Guven O, Sanli O, et al. Is type 2 diabetes mellitus a predictive factor for incontinence after laparoscopic radical prostatectomy? A matched pair and multivariate analysis. J Urol. 2010. 183:1087–1091.
15. Wolin KY, Luly J, Sutcliffe S, Andriole GL, Kibel AS. Risk of urinary incontinence following prostatectomy: the role of physical activity and obesity. J Urol. 2010. 183:629–633.
16. Konety BR, Sadetsky N, Carroll PR. CaPSURE Investigators. Recovery of urinary continence following radical prostatectomy: the impact of prostate volume--analysis of data from the CaPSURE Database. J Urol. 2007. 177:1423–1425.
17. Stephenson AJ, Scardino PT, Bianco FJ Jr, DiBlasio CJ, Fearn PA, Eastham JA. Morbidity and functional outcomes of salvage radical prostatectomy for locally recurrent prostate cancer after radiation therapy. J Urol. 2004. 172(6 Pt 1):2239–2243.
18. You YC, Kim TH, Sung GT. Effect of bladder neck preservation and posterior urethral reconstruction during robot-assisted laparoscopic radical prostatectomy for urinary continence. Korean J Urol. 2012. 53:29–33.
19. Hwang JJ, Kim BY, Uchio EM. Improving urinary continence after radical prostatectomy: review of surgical modifications. Korean J Urol. 2009. 50:935–941.
20. Smither AR, Guralnick ML, Davis NB, See WA. Quantifying the natural history of post-radical prostatectomy incontinence using objective pad test data. BMC Urol. 2007. 7:2.
21. Gerullis H, Quast S, Eimer C, Bagner JW, Otto T. Sphincter lesions after radical prostatectomy-evaluation and classification. J Endourol. 2011. 25:1075–1080.
22. Lepor H, Kaci L. The impact of open radical retropubic prostatectomy on continence and lower urinary tract symptoms: a prospective assessment using validated self-administered outcome instruments. J Urol. 2004. 171:1216–1219.
23. Bauer RM, Bastian PJ, Gozzi C, Stief CG. Postprostatectomy incontinence: all about diagnosis and management. Eur Urol. 2009. 55:322–333.
24. Seckiner I, Yesilli C, Mungan NA, Aykanat A, Akduman B. Correlations between the ICIQ-SF score and urodynamic findings. Neurourol Urodyn. 2007. 26:492–494.
25. Costantini E, Lazzeri M, Bini V, Giannantoni A, Mearini L, Porena M. Sensitivity and specificity of one-hour pad test as a predictive value for female urinary incontinence. Urol Int. 2008. 81:153–159.
26. Abdel-fattah M, Barrington JW, Youssef M. The standard 1-hour pad test: does it have any value in clinical practice? Eur Urol. 2004. 46:377–380.
27. Mariotti G, Sciarra A, Gentilucci A, Salciccia S, Alfarone A, Di Pierro G, et al. Early recovery of urinary continence after radical prostatectomy using early pelvic floor electrical stimulation and biofeedback associated treatment. J Urol. 2009. 181:1788–1793.
28. Lai HH, Boone TB. Implantation of artificial urinary sphincter in patients with post-prostatectomy incontinence, and preoperative overactive bladder and mixed symptoms. J Urol. 2011. 185:2254–2259.
29. Grise P, Vautherin R, Njinou-Ngninkeu B, Bochereau G, Lienhart J, Saussine C, et al. I-STOP TOMS transobturator male sling, a minimally invasive treatment for post-prostatectomy incontinence: continence improvement and tolerability. Urology. 2012. 79:458–463.
30. Kocjancic E, Crivellaro S, Ranzoni S, Bonvini D, Gontero P, Frea B. Adjustable Continence Therapy for the treatment of male stress urinary incontinence: a single-centre study. Scand J Urol Nephrol. 2007. 41:324–328.
31. Leruth J, Waltregny D, de Leval J. The inside-out transobturator male sling for the surgical treatment of stress urinary incontinence after radical prostatectomy: midterm results of a single-center prospective study. Eur Urol. 2012. 61:608–615.
32. Schneider T, Sperling H, Rossi R, Schmidt S, Rubben H. Do early injections of bulking agents following radical prostatectomy improve early continence? World J Urol. 2005. 23:338–342.
33. Herschorn S, Bruschini H, Comiter C, Grise P, Hanus T, Kirschner-Hermanns R, et al. Surgical treatment of stress incontinence in men. Neurourol Urodyn. 2010. 29:179–190.
34. Bo K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int Urogynecol J Pelvic Floor Dysfunct. 2004. 15:76–84.
35. Floratos DL, Sonke GS, Rapidou CA, Alivizatos GJ, Deliveliotis C, Constantinides CA, et al. Biofeedback vs verbal feedback as learning tools for pelvic muscle exercises in the early management of urinary incontinence after radical prostatectomy. BJU Int. 2002. 89:714–719.
36. Manassero F, Traversi C, Ales V, Pistolesi D, Panicucci E, Valent F, et al. Contribution of early intensive prolonged pelvic floor exercises on urinary continence recovery after bladder neck-sparing radical prostatectomy: results of a prospective controlled randomized trial. Neurourol Urodyn. 2007. 26:985–989.
37. Ribeiro LH, Prota C, Gomes CM, de Bessa J Jr, Boldarine MP, Dall'Oglio MF, et al. Long-term effect of early postoperative pelvic floor biofeedback on continence in men undergoing radical prostatectomy: a prospective, randomized, controlled trial. J Urol. 2010. 184:1034–1039.
38. Goode PS, Burgio KL, Johnson TM 2nd, Clay OJ, Roth DL, Markland AD, et al. Behavioral therapy with or without biofeedback and pelvic floor electrical stimulation for persistent postprostatectomy incontinence: a randomized controlled trial. JAMA. 2011. 305:151–159.
39. Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010. 29:213–240.
40. Jost W, Marsalek P. Duloxetine: mechanism of action at the lower urinary tract and Onuf's nucleus. Clin Auton Res. 2004. 14:220–227.
41. Boy S, Reitz A, Wirth B, Knapp PA, Braun PM, Haferkamp A, et al. Facilitatory neuromodulative effect of duloxetine on pudendal motor neurons controlling the urethral pressure: a functional urodynamic study in healthy women. Eur Urol. 2006. 50:119–125.
42. Filocamo MT, Li Marzi V, Del Popolo G, Cecconi F, Villari D, Marzocco M, et al. Pharmacologic treatment in postprostatectomy stress urinary incontinence. Eur Urol. 2007. 51:1559–1564.
43. Cornu JN, Merlet B, Ciofu C, Mouly S, Peyrat L, Sebe P, et al. Duloxetine for mild to moderate postprostatectomy incontinence: preliminary results of a randomised, placebo-controlled trial. Eur Urol. 2011. 59:148–154.
44. Koski ME, Enemchukwu EA, Padmanabhan P, Kaufman MR, Scarpero HM, Dmochowski RR. Safety and efficacy of sling for persistent stress urinary incontinence after bulking injection. Urology. 2011. 77:1076–1080.
45. Sanchez-Ortiz RF, Broderick GA, Chaikin DC, Malkowicz SB, Van Arsdalen K, Blander DS, et al. Collagen injection therapy for post-radical retropubic prostatectomy incontinence: role of Valsalva leak point pressure. J Urol. 1997. 158:2132–2136.
46. Smith DN, Appell RA, Rackley RR, Winters JC. Collagen injection therapy for post-prostatectomy incontinence. J Urol. 1998. 160:364–367.
47. Klutke JJ, Subir C, Andriole G, Klutke CG. Long-term results after antegrade collagen injection for stress urinary incontinence following radical retropubic prostatectomy. Urology. 1999. 53:974–977.
48. Tiguert R, Gheiler EL, Gudziak MR. Collagen injection in the management of post-radical prostatectomy intrinsic sphincteric deficiency. Neurourol Urodyn. 1999. 18:653–658.
49. Lightner DJ, Fox J, Klingele C. Cystoscopic injections of dextranomer hyaluronic acid into proximal urethra for urethral incompetence: efficacy and adverse outcomes. Urology. 2010. 75:1310–1314.
50. Secin FP, Martinez-Salamanca JI, Eilber KS. Limited efficacy of permanent injectable agents in the treatment of stress urinary incontinence after radical prostatectomy. Arch Esp Urol. 2005. 58:431–436.
51. Imamoglu MA, Tuygun C, Bakirtas H, Yigitbasi O, Kiper A. The comparison of artificial urinary sphincter implantation and endourethral macroplastique injection for the treatment of postprostatectomy incontinence. Eur Urol. 2005. 47:209–213.
52. Bugel H, Pfister C, Sibert L, Cappele O, Khalaf A, Grise P. Intraurethral macroplastic injections in the treatment of urinary incontinence after prostatic surgery. Prog Urol. 1999. 9:1068–1076.
53. Mitterberger M, Marksteiner R, Margreiter E, Pinggera GM, Frauscher F, Ulmer H, et al. Myoblast and fibroblast therapy for post-prostatectomy urinary incontinence: 1-year followup of 63 patients. J Urol. 2008. 179:226–231.
54. Castle EP, Andrews PE, Itano N, Novicki DE, Swanson SK, Ferrigni RG. The male sling for post-prostatectomy incontinence: mean followup of 18 months. J Urol. 2005. 173:1657–1660.
55. Carmel M, Hage B, Hanna S, Schmutz G, Tu le M. Long-term efficacy of the bone-anchored male sling for moderate and severe stress urinary incontinence. BJU Int. 2010. 106:1012–1016.
56. Giberti C, Gallo F, Schenone M, Cortese P, Ninotta G. The bone anchor suburethral synthetic sling for iatrogenic male incontinence: critical evaluation at a mean 3-year followup. J Urol. 2009. 181:2204–2208.
57. Guimaraes M, Oliveira R, Pinto R, Soares A, Maia E, Botelho F, et al. Intermediate-term results, up to 4 years, of a bone-anchored male perineal sling for treating male stress urinary incontinence after prostate surgery. BJU Int. 2009. 103:500–504.
58. Welk BK, Herschorn S. The male sling for post-prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int. 2012. 109:328–344.
59. Rehder P, Gozzi C. Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol. 2007. 52:860–866.
60. Cornel EB, Elzevier HW, Putter H. Can advance transobturator sling suspension cure male urinary postoperative stress incontinence? J Urol. 2010. 183:1459–1463.
61. Rehder P, Mitterberger MJ, Pichler R, Kerschbaumer A, Glodny B. The 1 year outcome of the transobturator retroluminal repositioning sling in the treatment of male stress urinary incontinence. BJU Int. 2010. 106:1668–1672.
62. Cornu JN, Sebe P, Ciofu C, Peyrat L, Beley S, Tligui M, et al. The AdVance transobturator male sling for postprostatectomy incontinence: clinical results of a prospective evaluation after a minimum follow-up of 6 months. Eur Urol. 2009. 56:923–927.
63. Gill BC, Swartz MA, Klein JB, Rackley RR, Montague DK, Vasavada SP, et al. Patient perceived effectiveness of a new male sling as treatment for post-prostatectomy incontinence. J Urol. 2010. 183:247–252.
64. Cornu JN, Sebe P, Ciofu C, Peyrat L, Cussenot O, Haab F. Mid-term evaluation of the transobturator male sling for post-prostatectomy incontinence: focus on prognostic factors. BJU Int. 2011. 108:236–240.
65. Davies TO, Bepple JL, McCammon KA. Urodynamic changes and initial results of the AdVance male sling. Urology. 2009. 74:354–357.
66. Bauer RM, Mayer ME, May F, Gratzke C, Buchner A, Soljanik I, et al. Complications of the AdVance transobturator male sling in the treatment of male stress urinary incontinence. Urology. 2010. 75:1494–1498.
67. Sousa-Escandon A, Cabrera J, Mantovani F, Moretti M, Ioanidis E, Kondelidis N, et al. Adjustable suburethral sling (male remeex system) in the treatment of male stress urinary incontinence: a multicentric European study. Eur Urol. 2007. 52:1473–1479.
68. Romano SV, Metrebian SE, Vaz F, Muller V, D'Ancona CA, Costa DE Souza EA, et al. An adjustable male sling for treating urinary incontinence after prostatectomy: a phase III multicentre trial. BJU Int. 2006. 97:533–539.
69. Hubner WA, Gallistl H, Rutkowski M, Huber ER. Adjustable bulbourethral male sling: experience after 101 cases of moderate-to-severe male stress urinary incontinence. BJU Int. 2011. 107:777–782.
70. Dalpiaz O, Knopf HJ, Orth S, Griese K, Aboulsorour S, Truss M. Mid-term complications after placement of the male adjustable suburethral sling: a single center experience. J Urol. 2011. 186:604–609.
71. Kjær L, Fode M, Norgaard N, Sonksen J, Nordling J. Adjustable continence balloons: clinical results of a new minimally invasive treatment for male urinary incontinence. Scand J Urol Nephrol. 2012. 46:196–200.
72. Hubner WA, Schlarp OM. Treatment of incontinence after prostatectomy using a new minimally invasive device: adjustable continence therapy. BJU Int. 2005. 96:587–594.
73. Lebret T, Cour F, Benchetrit J, Grise P, Bernstein J, Delaporte V, et al. Treatment of postprostatectomy stress urinary incontinence using a minimally invasive adjustable continence balloon device, ProACT: results of a preliminary, multicenter, pilot study. Urology. 2008. 71:256–260.
74. Hudak SJ, Morey AF. Impact of 3.5 cm artificial urinary sphincter cuff on primary and revision surgery for male stress urinary incontinence. J Urol. 2011. 186:1962–1966.
75. Gomha MA, Boone TB. Artificial urinary sphincter for post-prostatectomy incontinence in men who had prior radiotherapy: a risk and outcome analysis. J Urol. 2002. 167(2 Pt 1):591–596.
76. Perez LM, Webster GD. Successful outcome of artificial urinary sphincters in men with post-prostatectomy urinary incontinence despite adverse implantation features. J Urol. 1992. 148:1166–1170.
77. Yang JB, Lee YS, Han DH, Lee KS. Efficacy and safety of artificial urinary sphincter for stress urinary incontinence after prostate surgery. Korean J Urol. 2009. 50:854–858.
78. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008. 179:1912–1916.
79. Lai HH, Hsu EI, Teh BS, Butler EB, Boone TB. 13 years of experience with artificial urinary sphincter implantation at Baylor College of Medicine. J Urol. 2007. 177:1021–1025.
80. Gousse AE, Madjar S, Lambert MM, Fishman IJ. Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol. 2001. 166:1755–1758.
81. Montague DK. The artificial urinary sphincter (AS 800): experience in 166 consecutive patients. J Urol. 1992. 147:380–382.
82. Trigo Rocha F, Gomes CM, Mitre AI, Arap S, Srougi M. A prospective study evaluating the efficacy of the artificial sphincter AMS 800 for the treatment of postradical prostatectomy urinary incontinence and the correlation between preoperative urodynamic and surgical outcomes. Urology. 2008. 71:85–89.
83. Haab F, Trockman BA, Zimmern PE, Leach GE. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of follow up. J Urol. 1997. 158:435–439.
84. Litwiller SE, Kim KB, Fone PD, White RW, Stone AR. Post-prostatectomy incontinence and the artificial urinary sphincter: a long-term study of patient satisfaction and criteria for success. J Urol. 1996. 156:1975–1980.
85. Afraa TA, Campeau L, Mahfouz W, Corcos J. Urodynamic parameters evolution after artificial urinary sphincter implantation for post-radical prostatectomy incontinence with concomitant bladder dysfunction. Can J Urol. 2011. 18:5695–5698.
86. Leach GE, Trockman B, Wong A, Hamilton J, Haab F, Zimmern PE. Post-prostatectomy incontinence: urodynamic findings and treatment outcomes. J Urol. 1996. 155:1256–1259.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download