Abstract
Purpose
To evaluate the efficacy of photoselective vaporization of the prostate (PVP) with the 120 W Greenlight high performance system (HPS) laser for the treatment of benign prostatic hyperplasia (BPH) with intravesical prostatic protrusion (IPP).
Materials and Methods
This study was conducted on 389 BPH patients who underwent PVP with the 120 W HPS laser from April 2009 to August 2011. The patients were divided into groups according to IPP: group I was defined as IPP of 0 to 5 mm (n=216), group II as IPP of 5 to 10 mm (n=135), and group III as IPP above 10 mm (n=38). Prostate volume, prostate-specific antigen, International Prostate Symptom Score (IPSS), maximal urinary flow rate (Qmax), and postvoid residual volume (PVR) were assessed and checked at postoperative 1, 3, 6, and 12 months.
Results
There was a significant difference in the mean prostate size in each group (p<0.05). The preoperative total IPSS score, IPSS voiding symptom score, and quality of life score were not significantly different. However, the IPSS storage symptom score was significantly different between groups 1 and 2 and group 3. IPSS scores, Qmax, and PVR at postoperative 1, 3, 6, and 12 months showed significant improvement compared with preoperative values.
Conclusions
The degree of IPP can affect storage symptoms. However, there is no significant correlation between the degree of IPP and postoperative results. Also, the degree of IPP does not affect short- and long-term PVP results. Proper elimination of bladder outlet obstruction is important for symptomatic relief.
Benign prostatic hyperplasia (BPH) is a common problem in aging males [1] and the most common cause of bladder outlet obstruction (BOO) in men over 50 years old [2]. BPH is known to be associated with lower urinary tract symptoms (LUTS) and acute urinary retention [3,4]. However, several studies have suggested that it is not the prostate volume alone that causes LUTS, but rather the extent of protrusion of the enlarged prostate lobe into the bladder [5].
Intravesical prostatic protrusion (IPP) is a gross structural morphologic change due to the development of prostatic adenoma. It is induced by the enlargement of the lateral and median lobes. BPH with a mildly enlarged prostate and high IPP can cause obstruction by creating a 'ball-valve' effect and abnormal movement of the bladder due to the inhibition of the funnel effect of the bladder neck at voiding [6-8]. Some studies have implied the correlation of ultrasonically measured IPP and LUTS related to BPH. For example, Tan and Foo [9] discovered that the outcomes of a voiding trial correlated with the degree of IPP. Chia et al. [10] suggested IPP to be a parameter for predicting BOO because of its good correlation with the results of conventional pressure-flow study.
The current gold standard of removing a BOO due to BPH is a transurethral resection of the prostate (TURP). Recently, however, various lasers and advanced techniques have been applied. As a result, laser photoselective vaporization of the prostate (PVP), a minimally invasive surgical technique, has been replacing conventional TURP.
PVP has been reported to be a safe and effective technique for removing an enlarged prostate. In short- and long-term follow-up studies, the postoperative results, including symptom improvement, were similar to TURP, and reoperation risks and complications such as retrograde ejaculations were similar to or lower than TURP [11]. Because of its safety and effectiveness, PVP can be used with patients who take oral anticoagulant medications [12].
As mentioned before, laser PVP is a safe and effective technique. However, technical difficulty remains, especially with BPH patients who have severe IPP or a high bladder neck. These difficulties might affect the surgical outcomes.
The aim of this study was to determine the efficacy of PVP using the 120 W Greenlight high performance system (HPS) laser for the treatment of BPH groups according to the degree of IPP.
From April 2009 to August 2011, this study was conducted on patients who visited a urologic outpatient clinic because of LUTS and underwent TRUS (transrectal ultrasonography), uroflowmetry, and measurement of postvoid residual volume (PVR), prostate-specific antigen (PSA), and International Prostate Symptom Score (IPSS). The research protocol was approved by the Catholic Medical Center Institutional Review Board. Operation indications were persistent LUTS regardless of proper medication with an a-blocker or 5a-reductase inhibitor, refusal of medical treatment, and persistent hematuria originating from the prostate. Patients with urologic tumors, uncontrolled diabetes, neurogenic bladder including detrusor overactivity, urinary tract infection, or bladder stones that could affect voiding were excluded. Patients with a PSA value over 4.0 ng/ml underwent a TRUS-guided extended prostate biopsy. In these patients, only patients with pathologically proven BPH were enrolled in this study.
The prostate was assessed by TRUS by moving the sagittal scan of the ultrasound probe both horizontally and longitudinally and examining the bladder neck for protrusion of the prostate into the bladder. IPP was measured from images of the prostate obtained from TRUS by using a midline sagittal image and drawing a line from the anterior to posterior intersections of the bladder base and tip of the IPP. For more precise IPP measurement, the vertical distance from the tip of the protrusion to the circumference of the bladder at the base of the prostate gland was assessed by one urologist.
According to the grading system suggested by Nose et al. [13], cutoffs of IPP were set at 5 mm and 10 mm or greater. Bladders with IPP of 5 mm or less were assigned to group 1, 5 to 10 mm to group 2, and greater than 10 mm to group 3.
IPSS with quality of life (QoL), maximal urinary flow rate (Qmax), and PVR were used for pre- and postoperative comparative variables. During the operation, operation time, laser exposure time, and the amount of laser energy were evaluated. All patients underwent assessment of IPSS, Qmax, and PVR at 1, 3, 6, and 12 months after the operation.
Statistical analysis was performed by using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). A paired t-test was used to analyze the pre- and postoperative variables in the patients. A repeated-measures analysis of variance was used to analyze the correlations between groups. All valuables were presented as the mean with the standard deviation. A p-value of less than 0.05 was set as the threshold for statistical significance.
A total of 389 men participated in the study. The patients' mean age was 72 years (range, 52 to 88 years). Transrectal ultrasonic IPP grading was performed in all patients. Of the men studied, 216 had an IPP of 0 to 5 mm (group 1), 135 had an IPP of 5 to 10 mm (group 2), and 38 had an IPP of 10 mm or more (group 3) (Table 1).
The mean age of each group was 70.81±7.99 years in group 1, 70.88±8.64 years in group 2, and 74.89±9.66 years in group 3. There were no significant differences in age or PSA level between the groups (Table 1).
The mean prostate volume acquired from TRUS was analyzed and compared among the groups. The prostate volumes of group 1, group 2, and group 3 were significantly different. The preoperative total IPSS score, voiding symptom score, storage symptom score, and QoL score were analyzed and there were no significant differences except for the storage symptom score. There was a significant difference in the storage symptom scores between group 1 (8.5±5.1) and group 3 (10.8±4.9) and between group 2 (9.0±4.5) and group 3 (10.8±4.9) (p<0.05). However, there was no significant difference in the storage symptom score between group 1 and group 2 (p>0.05) (Table 1).
The operation time, laser exposing time, and total energy were analyzed, and there were no significant differences between the groups (Table 1).
There were no intraoperative or immediate postoperative complications due to uncontrollable gross hematuria.
In the time frame of 1, 3, 6, and 12 months after the operation, all variables were reevaluated and compared with the preoperative data. In group 1, the total IPSS score, the voiding symptom score, and the storage symptom score had significantly improved at 1 month postoperatively compared with the preoperative data (Figs. 1, 2, 3). Qmax, PVR, and the QoL score at 1 month following the operation also showed similar significant improvement when compared with the preoperative data (Figs. 4, 5, 6). These improvements were maintained for 12 months after the operation. In the analysis of group 2 and group 3, there were similar postoperative improvements compared with the preoperative data (p<0.05).
At 1 month after the operation, the clinical indexes of group 1 were compared with the clinical indexes of group 2 and group 3. No significant differences were found in the intergroup analysis, including for the total IPSS score, storage symptom score, voiding symptom score, QoL, Qmax, and PVR. These results were sustained at 3, 6, and 12 months after the operation (p<0.05).
During the 12-month follow-up period, none of patients in the three groups developed hematuria, urethral stricture, infection, or any other complication. Small numbers of patients (n=14) complained of mild dysuria, which improved with conservative care and proper medications.
In the preoperative comparison of the IPSS, the storage symptom scores were significantly different between groups 1 and 2 and group 3. Group 3, which had more severe IPP, had a higher IPSS storage symptoms score. This was due to the "ball-valve" effect. Our study demonstrated that voiding symptoms, storage symptoms, and QoL were improved after 120 W Greenlight HPS PVP in BPH patients with IPP. Both Qmax and PVR were improved following the operation. Also, these improved states were maintained for 12 months after the operation regardless of degree of IPP.
Recently, several studies have reported the importance of anatomical factors in evaluating men with LUTS [7,8]. IPP represents the median and lateral lobes of a prostate that have protruded into the bladder and causes a ball-valve type of obstruction and disruption of the funnel effect of the bladder neck, which increases urethral resistance [8]. In addition, the presence of median lobe enlargement causes dyskinetic movement at the time of micturition [7]. With severe IPP, the prostatic enlargement causes the bladder outlet to narrow and changes the shape of the internal urethral orifice. To open a compressed urethra, stronger detrusor contractile force is needed, which aggravates the ball-valve effect [14]. Detrusor overactivity and low bladder compliance are the manifestation of an impaired detrusor as a result of BOO [14]. Moreover, there is a higher risk of detrusor impairment and lower bladder compliance with more severe IPP. Ochiai and Kojima [15] emphasized the importance of bladder weight and prostatic configuration in the determination of intravesical obstruction. These anatomical configurations of the prostate, in particular the grade of IPP, could affect voiding [8].
In more detail, this effect could affect bladder wall thickness. Bladder wall thickening increases the extracellular collagen and nerve thickening, thereby inducing storage symptoms by activating the unmyelinated C nerve fibers, which are absent in normal bladder [16]. After the Greenlight HPS PVP, these storage symptom scores decreased in all groups. These findings are underpinned by the results of other reports showing that laser therapy is effective for reducing overactive bladder symptoms because the laser can vaporize the entire urothelium and submucosal tissue of the prostate urethra and bladder neck [17]. PVP denervates the afferent neurons responsible for initiating involuntary detrusor muscle contraction [18]. Furthermore, in our study, the preoperative difference between group 1, group 2, and group 3 was improved similarly. These results suggest that proper elimination of BOO could induce favorable outcomes, even in patients with severe IPP.
Detrusor overactivity is observed in about 50% of BOO patients [19]. Also, these overactive bladder symptoms have been found to be related to storage symptoms rather than voiding symptoms, especially after TURP [20]. These symptoms could be easily found by using an IPSS questionnaire. Chia et al. [10] reported the relationship between IPSS and IPP. They measured IPP through abdominal sonography and concluded that IPP affects voiding symptoms more than storage symptoms. In our study, however, IPP had a relationship with the storage symptom score rather than the voiding symptom score. This would be the case because the storage symptom score of the IPSS is underestimated compared with the voiding symptom score. We measured IPP through TRUS, and IPP showed a significant correlation with the storage symptom score. It may be that the IPP not only created the BOO and voiding symptoms but also aggravated the storage symptoms by lengthening the prostatic urethra and irritating the bladder trigonal area.
IPP can be measured by transabdominal ultrasonography or TRUS. Transabdominal ultrasonography can be used for patients who have a history of anal surgery or rectal disease. Transabdominal ultrasonography is less invasive than TRUS. For accurate measurement, the bladder should be filled with the proper volume of urine. Too much urine in the bladder can compress the IPP and too little urine can make IPP measurement difficult [21]. TRUS is more invasive than transabdominal ultrasonography. However, it does not require bladder filling; thus, more accurate IPP measurement is possible [22].
In this study, IPP was measured with TRUS and the relation with the preoperative storage symptom score and IPP was affirmed. We suggest that IPP measurement with TRUS would complement the deficiencies of the IPSS in a BPH patient with LUTS symptoms. To verify this, a prospective study would need to be carried out rather than a retrospective study.
In our study, in addition to the storage symptom score, voiding symptom scores, total IPSS scores, and QoL scores were significantly improved after the operation. These improvements were compared among each group and there were no intergroup differences after the operation. According to our results, preoperative IPSS storage symptoms were affected by IPP and postoperative IPSS storage symptoms were significantly improved in all IPP groups. We suggest that these findings were the result of the method used to resolve the BOO, that is, laser techniques.
The technical issue of HPS laser PVP is that it is difficult to effectively vaporize the prostate, especially in patients with a high bladder neck, severe IPP causing difficulty in recognizing the ureteral orifice, and bladder neck bleeding during the vaporization. These difficulties might lead to incomplete vaporization and induce unfavorable results. Hence, HPS laser PVP is generally recognized to be more difficult for effectively removing IPP than is conventional TURP. In the HPS laser PVP technique and training recommendation, gentle fingertip movements of the laser fiber and cystoscope are recommended, and progressive smoothening of the bladder neck contour is needed to avoid ureteral orifice injury [23]. Effective bladder neck vaporization can be achieved through the use of these techniques and can lead to favorable results.
Qmax and PVR are objective parameters that can be monitored after the elimination of BOO. In group 1, the Qmax had improved after the operation with time. The results at postoperative 1 month showed marked improvement compared with the preoperative state, and the improvements remained over 12 months. This finding was similar for group 2 and group 3. The PVR showed similar results also. PVR improved over time after the operation, and the difference was significant in all groups (p<0.05).
According to these results, we can assume that proper elimination of BOO will improve the subjective and objective parameters, regardless of the volume of prostate.
Our study had several limitations. It did not have a long follow-up time and was a retrospective study. Although our findings are statistically significant, they may not satisfactorily explain the actual mechanism. We propose that this study serve as the initiation of a larger and longer validation study of the importance of prostatic configuration.
The degree of IPP can affect preoperative storage symptoms. However, there is no significant correlation between the degree of IPP and postoperative variables after prostate vaporization. Also, the degree of IPP does not affect the short- and long-term results of PVP. Proper elimination of BOO is important for symptomatic relief.
Figures and Tables
FIG. 1
International Prostate Symptom Score (IPSS). Preop, preoperation. a:p<0.05 compared with preoperative score.

FIG. 2
International Prostate Symptom Score (IPSS). Preop, preoperation. a:p<0.05 compared with preoperative score.
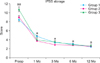
FIG. 3
International Prostate Symptom Score (IPSS). Preop, preoperation. a:p<0.05 compared with preoperative score.
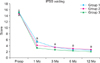
FIG. 4
International Prostate Symptom Score (IPSS) quality of life (QoL). Preop, preoperation. a:p<0.05 compared with preoperative score.
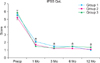
FIG. 5
Maximal Urinary Flow Rate (Qmax). Preop, preoperation. a:p<0.05 compared with preoperative score.
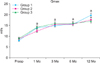
FIG. 6
Postvoid residual volume (PVR). Preop, preoperation. a:p<0.05 compared with preoperative score.
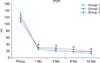
TABLE 1
Baseline characteristics of each patient group

Values are presented as mean±SD (range) or mean±SD.
Group I, IPP of 0 to 5 mm (n=216); Group II, IPP of 5 to 10 mm (n=135); Group III, IPP above 10 mm (n=38); IPP, intravesical prostatic protrusion; PSA, prostate-specific antigen; IPSS,International Prostate Symptom Score; QoL, quality of life.
a:p<0.05 compared with group I, b:p<0.05 compared with group II, c:p<0.05 compared with group III.
References
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.
2. Chapple CR, Roehrborn CG. A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol. 2006. 49:651–658.
3. Girman CJ, Jacobsen SJ, Guess HA, Oesterling JE, Chute CG, Panser LA, et al. Natural history of prostatism: relationship among symptoms, prostate volume and peak urinary flow rate. J Urol. 1995. 153:1510–1515.
4. Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997. 158:481–487.
5. Lieber MM, Jacobson DJ, McGree ME, St Sauver JL, Girman CJ, Jacobsen SJ. Intravesical prostatic protrusion in men in Olmsted County, Minnesota. J Urol. 2009. 182:2819–2824.
6. Lim KB, Ho H, Foo KT, Wong MY, Fook-Chong S. Comparison of intravesical prostatic protrusion, prostate volume and serum prostatic-specific antigen in the evaluation of bladder outlet obstruction. Int J Urol. 2006. 13:1509–1513.
7. Kuo HC. Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology. 1999. 54:90–96.
8. Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology. 2007. 70:1096–1099.
9. Tan YH, Foo KT. Intravesical prostatic protrusion predicts the outcome of a trial without catheter following acute urine retention. J Urol. 2003. 170(6 Pt 1):2339–2341.
10. Chia SJ, Heng CT, Chan SP, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 2003. 91:371–374.
11. Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004. 172(4 Pt 1):1404–1408.
12. Ruszat R, Wyler S, Forster T, Reich O, Stief CG, Gasser TC, et al. Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol. 2007. 51:1031–1038.
13. Nose H, Foo KT, Lim KB, Yokoyama T, Ozawa H, Kumon H. Accuracy of two noninvasive methods of diagnosing bladder outlet obstruction using ultrasonography: intravesical prostatic protrusion and velocity-flow video urodynamics. Urology. 2005. 65:493–497.
14. Styles RA, Neal DE, Griffiths CJ, Ramsden PD. Long-term monitoring of bladder pressure in chronic retention of urine: the relationship between detrusor activity and upper tract dilatation. J Urol. 1988. 140:330–334.
15. Ochiai A, Kojima M. Correlation of ultrasound-estimated bladder weight with ultrasound appearance of the prostate and postvoid residual urine in men with lower urinary tract symptoms. Urology. 1998. 51:722–729.
16. Dinis P, Silva J, Ribeiro MJ, Avelino A, Reis M, Cruz F. Bladder C-fiber desensitization induces a long-lasting improvement of BPH-associated storage LUTS: a pilot study. Eur Urol. 2004. 46:88–93.
17. Donovan JL, Peters TJ, Neal DE, Brookes ST, Gujral S, Chacko KN, et al. A randomized trial comparing transurethral resection of the prostate, laser therapy and conservative treatment of men with symptoms associated with benign prostatic enlargement: the CLasP study. J Urol. 2000. 164:65–70.
18. Housami F, Abrams P. Persistent detrusor overactivity after transurethral resection of the prostate. Curr Urol Rep. 2008. 9:284–290.
19. Van Venrooij GE, Van Melick HH, Eckhardt MD, Boon TA. Correlations of urodynamic changes with changes in symptoms and well-being after transurethral resection of the prostate. J Urol. 2002. 168:605–609.
20. Seki N, Yuki K, Takei M, Yamaguchi A, Naito S. Analysis of the prognostic factors for overactive bladder symptoms following surgical treatment in patients with benign prostatic obstruction. Neurourol Urodyn. 2009. 28:197–201.
21. Yuen JS, Ngiap JT, Cheng CW, Foo KT. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol. 2002. 9:225–229.
22. Mariappan P, Brown DJ, McNeill AS. Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. J Urol. 2007. 178:573–577.
23. Muir G, Gomez Sancha F, Bachmann A, Choi B, Collins E, de la Rosette J, et al. Techniques and training with GreenLight HPS 120-W laser therapy of the prostate: position paper. Euro Urol Suppl. 2008. 7:370–377.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download