Abstract
Purpose
Extracorporeal Shock Wave Lithotripsy (ESWL) has shown successful outcomes for ureteral stones. We investigated predictive factors for failure of ESWL for treating ureteral stones.
Materials and Methods
A total of 153 patients who underwent ESWL between July 2006 and July 2009 for ureteral stones diagnosed by non-enhanced spiral computed tomography were divided into two groups: (group A, stone size ≤10 mm; and group B, stone size >10 mm). The failure was defined as remnant stones >4 mm. We assessed age, sex, body mass index, stone size, laterality, location, skin-to-stone distance (SSD), Hounsfield unit, and the presence of secondary signs (hydronephrosis, renal enlargement, perinephric fat stranding, and tissue rim sign). We analyzed predictive factors by using logistic regression in each group.
Results
The success rates were 90.2% and 68.6% in group A and B, respectively. In the univariate analysis of each group, stone size, SSD, and all secondary signs showed statistically significant differences in terms of the outcome of ESWL (p<0.05). In the multivariate logistic regression, stone size (odds ratio [OR], 50.005; 95% confidence interval [CI], 6.207 to 402.852) was an independent predictive factor in group A. The presence of perinephric fat standing (OR, 77.634; 95% CI, 1.349 to 446.558) and stone size (OR, 19.718; 95% CI, 1.600 to 243.005) were independent predictive factors in group B.
Extracorporeal shockwave lithotripsy (ESWL) has been considered as a first-line treatment for ureteral stones for the past 20 years [1]. The success rate of ESWL in the treatment of ureteral stones is about 80 to 90% [2]. Some patients whose stones may not be fragmented by repeated ESWL will require other surgical interventions. Failure of ESWL is more common with ureteral stones larger than 10 mm [3]. The success rate is influenced by stone factors (stone size, location, composition, degree of obstruction), clinical factors (symptom severity, patient's expectations, associated infection, solitary kidney, abnormal ureteral anatomy), and technical factors (available equipment, cost) [4]. However, it is not certain which factors influence the outcome of ESWL [5-8].
Recently, several studies have reported the incidence of secondary signs and their influence in ESWL treatment [9-12]. However, whether secondary signs affect the outcome in ESWL treatment remains controversial. Thus, we investigated the predictive factors of ESWL outcome, including secondary signs, in the treatment of ureteral stones.
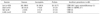
A total of 153 patients who underwent ESWL between July 2006 and July 2009 for ureteral stones that were diagnosed by non-enhanced spiral computed tomography (NESCT) were included in this retrospective study. The inclusion criteria were stone size >4 mm and stones that were solitary and radiopaque on the pretreatment plain radiography. Patients with urinary tract infections, blood coagulation disorders, ureteral stricture, neurogenic bladder, or polycystic kidney were excluded. We divided the patients into two groups (group A, stone size ≤10 mm; group B, stone size >10 mm) and assessed age, sex, body mass index (BMI), stone size, laterality, location, skin-to-stone distance (SSD), Hounsfield unit (HU), and presence of secondary signs (hydronephrosis, renal enlargement, perinephric fat stranding, and tissue rim sign) in each group (Table 1).
The BMI was measured for each patient by dividing the patient's weight in kilograms by height in meters squared. The SSD was measured on NESCT by three distances from the stone to the skin (0°, 45°, and 90°). The average SSD was measured from these values and was recorded as the representative SSD for each stone. The HU for each stone was determined on the pretreatment NESCT. Non-enhanced helical images were obtained by using a 5-mm collimation width from the top of the kidneys to the level of the pubic symphysis. Three regions of interest (ROI) were analyzed in the images showing the stones in the largest dimension. All measurements were made with a similar-sized ROI (2.0±0.5 mm2). The HU average of three ROIs represented the HU for that stone. Secondary signs included the presence or absence of hydronephrosis, renal enlargement, perinephric fat stranding, and tissue rim sign (Fig. 1). Hydronephrosis was distinguished by visualization of the dilated renal pelvocaliceal system. Renal enlargement was detected as an increase in the thickness of the renal parenchyma or an increase in the length of the kidney in acute obstruction. Perinephric fat stranding was defined as the stranding of adipose tissue around the kidney. Tissue rim sign was recognized as the observation of the annular soft tissue caused by edematous ureteral wall surrounding the stones [13]. All radiologic factors were reviewed by one specialized uroradiologist.
ESWL was performed by using an electroconductive lithotriptor (Sonolith Praktis, EDAP TMS, Vaulx-en-Velin, France). The generator power was started at 60% and increased stepwise to 100%. A maximum of 3,000 shockwaves (range, 1,500 to 3,000; median, 2,500) were delivered to a maximal power of 20 to 24 kV at 120 shocks/min during one session. The stones were fragmented under fluoroscopic guidance, and the number of shockwaves and energy level were recorded. The result of treatment was evaluated by plain radiography at 1 or 2 weeks after each ESWL. When there was a large fragment with a long diameter >4 mm, ESWL was tried repeatedly until each fragment became smaller than 4 mm. The failure of ESWL was defined as remnant stones larger than 4 mm at 3 months after the first session.
The data were analyzed to identify clinical and radiologic factors associated with treatment failure. Univariate analysis was used to individually assess the association between the various factors and outcomes. Thereafter, the significantly associated variables were tested with multivariate logistic regression analysis to identify the independent predictors of treatment failure. Statistical analysis was performed by using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Values of p<0.05 were considered statistically significant.
A total of 153 patients with ureteral stones were analyzed. The patients' mean age was 54.5±11.78 years (range, 34 to 74 years) in group A and 55.5±13.28 years (range, 32 to 79 years) in group B. The mean stone size was 6.1±1.36 mm (range, 4.1 to 10.0 mm) and 14.3±4.65 mm (range, 10.1 to 22.0 mm) in each group. The success rate was 90.2% and 68.6%, respectively (Table 1).
The overall success rate was 83.0% (n=127) and the failure rate was 17.0% (n=26). Patients in whom ESWL failed underwent auxiliary procedures. Twenty-five patients with remnants after ESWL underwent ureteroscopic removal of stone and 1 patient underwent open ureterolithotomy (Table 2). We observed a complication rate of 3.2% (n=5), including acute pyelonephritis (n=3, 1.9%) that was successfully treated by percutaneous nephrostomy catheterization with antibiotics and a subcapsular hematoma (n=2, 1.3%) that resolved spontaneously. A static steinstrasse was observed in 3 patients and analgesics were required in 5 patients for 1 day for post-ESWL pain.
In the univariate analysis, age, sex, BMI, laterality, location, and HU were not significantly different in terms of outcome of ESWL (Table 3). The mean stone size in the success and failure groups, respectively, was 5.9±1.27 mm vs. 7.5±1.43 mm in group A (p<0.001) and 12.2±2.15 mm vs. 19.1±4.15 mm in group B (p<0.001). The mean SSD in the success and failure groups, respectively, was 102.4±12.88 mm vs. 110.8±5.66 mm in group A (p=0.043) and 97.8±12.97 mm vs. 107.9±13.02 mm in group B (p=0.013) (Table 3). All the secondary signs showed statistically significant differences in terms of outcome of ESWL (Table 3).
In the multivariate logistic regression, stone size (odds ratio [OR], 50.005; 95% confidence interval [CI], 6.207 to 402.852) was an independent predictive factor for failure of ESWL in group A. Perinephric fat standing (OR, 77.634; 95% CI, 1.349 to 446.558) and stone size (OR, 19.718; 95% CI, 1.600 to 243.005) were independent predictive factors in group B (Table 4).
Since its introduction in the early 1980s, ESWL has become a safe and accepted treatment modality for ureteral stones [1]. The success rate of ESWL in the treatment of ureteral stones is about 80 to 90% [2]. Many studies have demonstrated that the consistency, size, shape, location, and HU of ureteral stones and BMI may be predictors of the outcome of ESWL [4-8].
Concerning stone size, a larger size is associated with a higher risk for failure of treatment of urinary tract stones. Recent studies have shown that stone size is an independent predictor of the stone-free rate after ESWL [14-17]. It has been reported that patients with stones >10 mm more frequently fail to be rendered stone-free by ESWL [18]. In the 2007 American Urological Association/European Association of Urology guideline, ureteral stones were classified as either less than or greater than 10 mm. At all locations in the ureter, the treatment outcome for stones less than 10 mm was superior to that for stones greater than 10 mm [4]. Specifically, for stones in the distal ureter, the stone-free rate for stones less than 10 mm treated by SWL was 86%, compared with a 74% stone-free rate for those greater than 10 mm [4]. In our series, we divided the patients into two groups and evaluated their outcomes and predictive factors. The success rates were 90.2% in the group with a stone size ≤10 mm (group A) and 68.6% in the group with a stone size >10 mm (group B). The multivariate analysis revealed that stone size was an independent predictor of failure of ESWL in each group.
A positive correlation exists between SSD and BMI when examining all upper tract stones. BMI and SSD are certainly interrelated, but body fat distribution varies between by gender and race [19] and cannot be reliably used as a surrogate marker for SSD. The utility of BMI in predicting successful ESWL is variable. For example, Pareek et al. [8] found BMI to be a significant predictor of success. Conversely, in another study, BMI failed to predict successful ESWL outcomes, whereas SSD remained a significant predictor [20]. In our series, BMI was not a significant predictor of failure of ESWL. We suggest that the effect of BMI is probably related to the distance of the stone from the skin, which reflects the shockwave path in the body. BMI may not truly reflect central body fat distribution, which is probably the main factor affecting SSD. Therefore, SSD is probably a more direct measurement of the effect of body build on ESWL outcome than is BMI.
Many investigators have reported that SSD is a significant predictor in ureteral stones. Wiesenthal et al. [21] suggested that SSD was a significant predictor of lithotripsy success for ureteral stones. In the multivariate analysis, SSD >110 mm (OR, 0.49; 95% CI, 0.31 to 0.78) was a significant predictor of outcome. Perks et al. [22] also supported this finding. They reported that SSD of <9 cm (OR: 2.8; 95% CI: 1.1-7.2) can predict SWL success. In our series, SSD was a significant predictor of treatment outcome in the univariate analysis (<1.0 cm group, p=0.043; >1.0 cm group, p=0.013), but was not a significant predictor in the multivariate analysis (<1.0 cm group, p=0.082; >1.0 cm group, p=0.110). We may not have had enough data to distinguish the body fat distribution (range, 81.4 to 124.1 mm), and additional evidence from larger trials may reveal the importance of SSD in the management of ureteral stones.
The attenuation value of ureteral stones on axial computed tomography images has been studied as a predictor of fragmentation efficiency [8]. However, because these values differ according to the size of the ROI and portion in the same stone, the use of these values in the management of ureteral stones is still problematic. In our series, HU was not a significant predictor in the univariate analysis (p>0.05). We suggest that the small sample size and short range of HU (n=153, 617.2 to 982.5 HU) may have prevented accurate statistical comparison of the stone composition with the attenuation value.
A correlation between stone attenuation and stone fragility was first demonstrated in vitro. As the attenuation value of calcium stones increases, a greater number of shockwaves are needed for fragmentation [23]. Likewise, in a clinical retrospective review, patients with calculi > 750 HU were 10.5 times as likely to need ≥3 SWL sessions as were those with calculi of ≤750 HU [24]. Joseph et al. [7] reported a 95% success rate for calculi <1,000 HU vs. 55% for stones >1,000 HU (p<0.01). Several investigators have since shown that ESWL is more likely to fail for patients with renal calculi >750 to 1,000 HU and these patients should be considered for other treatment modalities [6-8,24].
Whether secondary signs in patients with ureteral stones affect outcome in ESWL treatment remains controversial. Ege et al. [25] reported the incidence of secondary signs and their influence on patient management. The most reliable signs indicating necessary endoscopic removal or lithotripsy were hydroureter, hydronephrosis, periureteral edema, and unilateral renal enlargement.
On the other hand, Boulay et al. [26] evaluated 99 patients and retrospectively analyzed the presence, size, and location of ureteral stones and the presence and severity of secondary signs of obstruction. A significant difference in stone size was found between patients who were treated conservatively and those who underwent a urological procedure (3.3±1.3 mm vs. 7.0±6.2 mm, p<0.1). The presence and severity of secondary signs of obstruction were not significantly different between the two groups and did not affect treatment. Those authors concluded that stone size alone correlated with the patient's treatment and outcome. In another study, Seitz et al. [27] reported secondary signs before laser ureterolithotripsy preoperatively did not correlate these with stone-free rates. The presence of secondary signs (renal enlargement, perinephric stranding, ureteral dilation, ureteral rim sign) could not predict intraoperatively verified stone impaction or stone-free rates.
Perinephric fat stranding is defined as linear areas of soft tissue attenuation in the perinephric space, which can result from any acute process or injury to the kidney. The changes in the perinephric space in the presence of urinary stones are thought to result from adaptation of the kidney to obstruction. Immediately after acute ureteral obstruction, the intraluminal pressure of the collecting system increases and reaches 3 to 5 times normal pressure [13]. The escape of urine into the renal interstitium (pyelotubular backflow), across the renal pelvis into the renal sinus (pyelosinus backflow), or into the lymphatic system (pyelolymphatic backflow) or the renal venous system (pyelovenous backflow) plays important roles in decompression of the intraluminal pressure [28]. As proposed by Kunin [29], lymphatic flow in the perinephric space results from elevated intrarenal venous pressure, and venous stasis, pyelosinus, and pyelovenous backflow may contribute to perinephric stranding [28]. Unilateral perinephric stranding is probably the manifestation of increased pressure in the collecting system in the early phase of ureteral obstruction. In our series, perinephric fat stranding was an independent predictor in group B (stone size >10 mm). Other secondary signs were not significant. All of the secondary signs are caused by ureteral obstruction; however, not all of these represent the degree of ureteral obstruction. We suggest that the perinephric fat stranding reflects a condition to maintain the balance between pressure in the collecting system and ureteral wall resistance around the stones. Despite increased pressure in the collecting system, the degree of obstruction was too severe in group B. In this condition, the outcomes of ESWL were probably less successful than in the group without perinephric fat stranding. Although the mechanism of perinephric fat stranding may be similar in patients with smaller stone sizes, perinephric fat stranding was not significant in group A. We speculate that the obstruction is more easily resolved in patients with smaller stone sizes. Thus, perinephric fat stranding may be a secondary sign that more readily reflects the degree of ureteral obstruction in the case of large stones.
Figures and Tables
FIG. 1
The non-enhanced computed tomography scan images of secondary signs. (A) Hydronephrosis of the right kidney. (B) Renal enlargement and perinephric fat stranding of the left kidney (arrowhead). (C) Tissue rim sign of the left ureter (arrow).

References
1. Chaussy C, Schmiedt E, Jocham D, Brendel W, Forssmann B, Walther V. First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. J Urol. 1982. 127:417–420.
2. Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. The American Urological Association. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997. 158:1915–1921.
3. Robert M, Delbos O, Guiter J, Grasset D. In situ piezoelectric extracorporeal shock wave lithotripsy of ureteric stones. Br J Urol. 1995. 76:435–439.
4. Lingeman JE, Matlaga BR. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Surgical management of upper urinary tract calculi. Campbell-Walsh urology. 2010. 10th ed. Philadelphia: Saunders;1375–1377.
5. Erturk E, Herrman E, Cockett AT. Extracorporeal shock wave lithotripsy for distal ureteral stones. J Urol. 1993. 149:1425–1426.
6. Pareek G, Armenakas NA, Fracchia JA. Hounsfield units on computerized tomography predict stone-free rates after extracorporeal shock wave lithotripsy. J Urol. 2003. 169:1679–1681.
7. Joseph P, Mandal AK, Singh SK, Mandal P, Sankhwar SN, Sharma SK. Computerized tomography attenuation value of renal calculus: can it predict successful fragmentation of the calculus by extracorporeal shock wave lithotripsy? A preliminary study. J Urol. 2002. 167:1968–1971.
8. Pareek G, Armenakas NA, Panagopoulos G, Bruno JJ, Fracchia JA. Extracorporeal shock wave lithotripsy success based on body mass index and Hounsfield units. Urology. 2005. 65:33–36.
9. Seitz C, Fajkovic H, Waldert M, Tanovic E, Remzi M, Kramer G, et al. Extracorporeal shock wave lithotripsy in the treatment of proximal ureteral stones: Does the presence and degree of hydronephrosis affect success? Eur Urol. 2006. 49:378–383.
10. Kim HS, Jang SW, Jeong YB, Kim YG, Kim JS. The usefulness of unenhanced helical computerized tomography in patients with urinary calculi. Korean J Urol. 2003. 44:796–800.
11. Song DW, Jeong TY, Lee SI, Kim DJ. Predicting factors for spontaneous passage of ureteral calculi based on unenhanced helical CT findings. Korean J Urol. 2008. 49:1094–1099.
12. Kang YI, Moon HY, Kim CS. Relationship between the success of extracorporeal shock wave lithotripsy (ESWL) and the degree of hydronephrosis when treating patients with upper ureteral stones. Korean J Urol. 2007. 48:422–427.
13. Türkbey B, Akpinar E, Ozer C, Turkbey EB, Eken V, Karçaaltincaba M, et al. Multidetector CT technique and imaging findings of urinary stone disease: an expanded review. Diagn Interv Radiol. 2010. 16:134–144.
14. Shiroyanagi Y, Yagisawa T, Nanri M, Kobayashi C, Toma H. Factors associated with failure of extracorporeal shock-wave lithotripsy for ureteral stones using Dornier lithotripter U/50. Int J Urol. 2002. 9:304–307.
15. Abdel-Khalek M, Sheir K, Elsobky E, Showkey S, Kenawy M. Prognostic factors for extracorporeal shock-wave lithotripsy of ureteric stones--a multivariate analysis study. Scand J Urol Nephrol. 2003. 37:413–418.
16. Argyropoulos AN, Tolley DA. Failure after shockwave lithotripsy: is outcome machine dependent? Int J Clin Pract. 2009. 63:1489–1493.
17. Hatiboglu G, Popeneciu V, Kurosch M, Huber J, Pahernik S, Pfitzenmaier J, et al. Prognostic variables for shockwave lithotripsy (SWL) treatment success: no impact of body mass index (BMI) using a third generation lithotripter. BJU Int. 2011. 108:1192–1197.
18. Kim HH, Lee JH, Park MS, Lee SE, Kim SW. In situ extracorporeal shockwave lithotripsy for ureteral calculi: investigation of factors influencing stone fragmentation and appropriate number of sessions for changing treatment modality. J Endourol. 1996. 10:501–505.
19. Rush E, Plank L, Chandu V, Laulu M, Simmons D, Swinburn B, et al. Body size, body composition, and fat distribution: a comparison of young New Zealand men of European, Pacific Island, and Asian Indian ethnicities. N Z Med J. 2004. 117:U1203.
20. Ng CF, Siu DY, Wong A, Goggins W, Chan ES, Wong KT. Development of a scoring system from noncontrast computerized tomography measurements to improve the selection of upper ureteral stone for extracorporeal shock wave lithotripsy. J Urol. 2009. 181:1151–1157.
21. Wiesenthal JD, Ghiculete D, D'A Honey RJ, Pace KT. Evaluating the importance of mean stone density and skin-to-stone distance in predicting successful shock wave lithotripsy of renal and ureteric calculi. Urol Res. 2010. 38:307–313.
22. Perks AE, Schuler TD, Lee J, Ghiculete D, Chung DG, D'A Honey RJ, et al. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology. 2008. 72:765–769.
23. Saw KC, McAteer JA, Fineberg NS, Monga AG, Chua GT, Lingeman JE, et al. Calcium stone fragility is predicted by helical CT attenuation values. J Endourol. 2000. 14:471–474.
24. Gupta NP, Ansari MS, Kesarvani P, Kapoor A, Mukhopadhyay S. Role of computed tomography with no contrast medium enhancement in predicting the outcome of extracorporeal shock wave lithotripsy for urinary calculi. BJU Int. 2005. 95:1285–1288.
25. Ege G, Akman H, Kuzucu K, Yildiz S. Acute ureterolithiasis: incidence of secondary signs on unenhanced helical CT and influence on patient management. Clin Radiol. 2003. 58:990–994.
26. Boulay I, Holtz P, Foley WD, White B, Begun FP. Ureteral calculi: diagnostic efficacy of helical CT and implications for treatment of patients. AJR Am J Roentgenol. 1999. 172:1485–1490.
27. Seitz C, Memarsadeghi M, Fajkovic H, Tanovic E. Secondary signs of non-enhanced CT prior to laser ureterolithotripsy: is treatment outcome predictable? J Endourol. 2008. 22:415–418.
28. Takahashi N, Kawashima A, Ernst RD, Boridy IC, Goldman SM, Benson GS, et al. Ureterolithiasis: can clinical outcome be predicted with unenhanced helical CT? Radiology. 1998. 208:97–102.
29. Kunin M. Bridging septa of the perinephric space: anatomic, pathologic, and diagnostic considerations. Radiology. 1986. 158:361–365.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download