Abstract
Purpose
During laparoscopic partial cystectomy (LPC), lesion identification is essential to help to determine the appropriate bladder incisions required to maintain adequate resection margins. The inability to use tactile senses makes it difficult for surgeons to locate lesions during laparoscopic surgery. Endoscopic India ink marking techniques are often used in laparoscopic gastroenterological surgery. We present our experience with performing LPC with India ink during the surgical resection of various bladder lesions.
Materials and Methods
LPC with cystoscopic fine needle tattooing was performed on 10 patients at our institute. Tattooing was performed at 1- to 2-cm intervals approximately 1 cm away from the outer margin of the lesion with enough depth (the deep muscle layer) under cystoscopic guidance. LPC was performed by the transperitoneal approach. The clinical courses and pathologic results were analyzed.
Results
All LPC with cystoscopic tattooing cases were performed successfully. The mean patient age was 39.1 years. The mean operative time was 130.5 minutes, and the mean estimated blood loss was 93 ml. The mean hospital stay was 13.1 days, and the mean duration of indwelling Foley catheterization was 10.7 days. There were no significant intraoperative or postoperative complications except 1 case of delayed urinary leak and 1 case of delayed wound healing. The pathological diagnosis included 1 urachal cancer, 1 urachal remnant, 4 urachal cysts, 2 pheochromocytomas, and 2 inflammatory masses. All specimens showed adequate surgical margins.
Partial cystectomy is an excellent method for bladder preservation. The procedure entails removing the full thickness of the bladder wall in a selected area for malignant and benign diseases of the bladder [1]. In partial cystectomy, resection with adequate surgical margins is essential.
Laparoscopic partial cystectomy (LPC) was first described by Nezhat and Nezhat [2] in 1993. The utilization of these approaches has subsequently expanded. The technique has been reported to be safe and efficacious. LPC minimizes the risks of complications related to radical cystectomy while preserving the bladder [3]. However, the inability to utilize tactile sense makes it hard for surgeons to locate lesions during laparoscopic surgery. As a result, identifying and demarcating suspicious areas remain problematic. If the tumor is not readily apparent from laparoscopic views, additional aids such as intraoperative cystoscopy should be used [4]. A safe and effective method is essential to overcome this challenge, and cystoscopic tattooing may assist in successfully guiding partial cystectomies.
Endoscopic India ink marking techniques are often used as a component of laparoscopic gastroenterological surgery for the intraoperative location of polyps and early stage neoplasms. In previous studies, the use of tattooing for the localization of colorectal lesions by use of laparoscopic approaches was reported to have been effective in over 90% of cases [5,6].
We report our experience in 10 LPC cases using cystoscopic tattooing with India ink. To our knowledge, this is the first reported series from a single institution.
Ten patients underwent LPC with cystoscopic fine needle tattooing by a single surgeon at our institution. For preoperative imaging, computed tomography (CT) scans and cystoscopy were conducted to assess the primary lesion. The CT scans demonstrated solitary, small bladder masses and no abnormalities in the upper urinary tract. No lymphadenopathy or visceral or bony metastasis was detected. Cystoscopy revealed lesions at the dome or posterior wall of the bladder in all patients.
After confirming no urinary leakage by cystogram on the 8th day after the operation, the urethral Foley catheter was removed. The clinical results and pathologic outcomes were evaluated retrospectively.
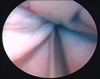
While under general anesthesia, all patients were placed in the lithotomy position. A well-lubricated 17.5 Fr cystoscope was inserted into the bladder. With India ink, tattooing was performed 1 cm away from the outer margin of the lesion with adequate depth into the deep muscle layer. An India ink solution was injected with a 23 G 350-mm needle (Deflux, Q-med AB, Uppsala, Sweden) (Fig. 1).
The patient was placed in a 30 degree Trendelenburg position. LPC using the transperitoneal approach was performed with 3 or 4 trocars. A Veress needle was used to create pneumoperitoneum and was inserted at a point 2 cm superior to the umbilicus where a 12-mm camera port was positioned. Another 12-mm trocar and one 5-mm trocar were placed in the right and left lower quadrant of the abdomen. An additional 5-mm trocar was placed medial to the right anterior superior iliac spine when required. After bladder filling with 200 ml of normal saline, the peritoneum was incised in a lateral direction until the medial umbilical ligament on either side, at the level of the inguinal canal, and to the cranial direction toward the umbilicus, forming an inverted 'V'. This dissection was followed caudally, in an antegrade manner, to enter the prevesical space of Retzius. The anterior wall of the bladder was then mobilized. After identifying the tattooed area around the mass of the dome site, the bladder wall was incised by using monopolar electrocautery or ultrasonic cutting shears following tattooing in the deflated state of the bladder (Fig. 2). An EndoCatch (Autusuture, Covidien, Mansfield, MA, USA) device was introduced to entrap the specimen and was placed in the right iliac fossa. The bladder was closed in two layers by watertight running sutures made with 2-0 Vicryl, and no urine leakage was detected after filling the bladder. The specimen was removed through an extension of the camera trocar site, and a Jackson Pratt drain (Easy Medicare, Incheon, Korea) was positioned in the prevesical space.
All cases of LPC with the cystoscopic tattooing technique are summarized in Table 1. All procedures were performed successfully without open conversion. The cohort comprised 1 man and 9 women, and the patients' mean age was 39.1 years (range, 20 to 65 years). All laparoscopic procedures were performed by the transperitoneal approach with the use of 3 or 4 trocars. Mean operative time, including tattooing, was 130.5 minutes (range, 110 to 175 minutes). The mean estimated blood loss was 93 ml (range, 30 to 250 ml). The mean duration of indwelling Foley catheterization was 10.7 days (range, 6 to 24 days). The mean hospital stay was 13.2 days (range, 9 to 38 days). There were no significant intraoperative or postoperative complications, but delayed urine leakage and delayed wound healing occurred separately and resolved spontaneously.
In most cases the tattoo was visible under laparoscopy except in one case that required cystoscopy to retrace the lesion during surgery. On the specimens, the tattoo was clearly visible in all patients. The pathological diagnosis included 1 urachal cancer, 1 urachal remnant, 4 urachal cysts, 2 pheochromocytomas, 2 inflammatory masses (vesico-enteric fistula, vesico-vaginal fistula). There were no positive surgical margins in the pathologic examinations. No recurrence was detected during the 18-month follow-up period.
LPC was initially performed for vesical endometriosis and was subsequently expanded to include malignant conditions [7,8]. The development of the laparoscopic technique allowed LPC to be performed more routinely. Its advantages include smaller incisions, minimal invasiveness of the procedure, reduced post-operative pain, faster recovery, and shorter hospitalization compared with open partial cystectomy [9,10]. LPC is performed in cases of benign bladder conditions, such as leiomyoma, pheochromocytoma, and endometriosis, and also in malignant bladder conditions and urachal remnants [4,10,11].
However, identification of the exact location of the tumor may be difficult from outside the bladder. Intraoperative localization of these tumors during laparoscopy is difficult for many reasons given that the laparoscopist is unable to palpate the lesion during the operation [12,13]. As a result, different methods such as intraoperative cystoscopy have been introduced to overcome identification challenges. As a useful technique, Abdel-Hakim et al. [14] reported that masses could be located by inflating and deflating the bladder with air during robot-assisted LPC. The use of intraoperative real-time transrectal ultrasound guidance was also reported to be helpful in patients whose tumors were lodged within a para-ureteral diverticulum [4]. Our method to solve this problem was to use an injection needle for mucosal tattooing by use of cystoscopy before the laparoscopic procedure. The tattoo method eliminates the need for intraoperative cystoscopic incision or repeated bladder filling.
Tattooing with India ink is a method first reported for colonic surgery in 1975 by Ponsky and King [15]. The safety and efficacy of this method was reported in other studies [6,12,13,16-21]. The absence of an inflammatory reaction even after 10 years as reported by McArthur et al. [6] is reassuring. India ink tattooing has been used for decades to tattoo skin without risks of incurring toxicity, and its usage in tattooing of the gastrointestinal tract has been reported to be safe [18-21]. In our experience, there was no toxicity or complications associated with the use of India ink in the bladder.
The presence of tattooing during surgery helped to target lesions in most of our patients. Tattooing of the lesions led to reduced operative time and improved the excision of tumors located submucosally or those too small to be recognized easily. The tattoo was not seen during the operation in 1 case. As a result, repeat intraoperative cystoscopy was performed to retrace the lesion. A second injection of India ink was administered to the bladder wall under laparoscopy. When tattooing is not visible, repeat tattooing may be helpful to ensure adequate visualization of appropriate resection margins.
The pathologic diagnosis for the patient in our study included benign (urachal remnant and urachal cyst, fistulae) and malignant (urachal cancer and pheochromocytoma) lesions. Adequate resection margins were confirmed by pathologic examination.
Cystoscopic tattooing with India ink in LPC is safe and feasible for variable bladder pathologies. Tattooing is a simple and effective technique for locating bladder lesions. This technique can help to determine the appropriate surgical margin during LPC without the need for additional complicated procedures.
Figures and Tables
References
1. Sweeney P, Kursh ED, Resnick MI. Partial cystectomy. Urol Clin North Am. 1992. 19:701–711.
2. Nezhat CR, Nezhat FR. Laparoscopic segmental bladder resection for endometriosis: a report of two cases. Obstet Gynecol. 1993. 81(5 Pt 2):882–884.
3. Mariano MB, Tefilli MV. Laparoscopic partial cystectomy in bladder cancer--initial experience. Int Braz J Urol. 2004. 30:192–198.
4. Colombo JR Jr, Desai M, Canes D, Frota R, Haber GP, Moinzadeh A, et al. Laparoscopic partial cystectomy for urachal and bladder cancer. Clinics (Sao Paulo). 2008. 63:731–734.
5. Feingold DL, Addona T, Forde KA, Arnell TD, Carter JJ, Huang EH, et al. Safety and reliability of tattooing colorectal neoplasms prior to laparoscopic resection. J Gastrointest Surg. 2004. 8:543–546.
6. McArthur CS, Roayaie S, Waye JD. Safety of preoperation endoscopic tattoo with india ink for identification of colonic lesions. Surg Endosc. 1999. 13:397–400.
7. Ferzli G, Wenof M, Giannakakos A, Raboy A, Albert P. Laparoscopic partial cystectomy for vesical endometrioma. J Laparoendosc Surg. 1993. 3:161–165.
8. Nezhat C, Nezhat F, Nezhat CH, Nasserbakht F, Rosati M, Seidman DS. Urinary tract endometriosis treated by laparoscopy. Fertil Steril. 1996. 66:920–924.
9. Kozlowski PM, Mihm F, Winfield HN. Laparoscopic management of bladder pheochromocytoma. Urology. 2001. 57:365.
10. Tai HC, Chung SD, Wang SM, Chueh SC, Yu HJ. Laparoscopic partial cystectomy for various bladder pathologies. BJU Int. 2007. 100:382–385.
11. Geol H, Kim DW, Kim TH, Seong YK, Cho WY, Kim SD, et al. Laparoscopic partial cystectomy for schwannoma of urinary bladder: case report. J Endourol. 2005. 19:303–306.
12. Allam ME, Mehta D, Zelen J, Fogler R. Posterior wall gastric leiomyoma: endoscopic tattooing facilitates laparoscopic resection. JSLS. 1998. 2:83–84.
13. Aboosy N, Mulder CJ, Berends FJ, Meijer JW, Sorge AA. Endoscopic tattoo of the colon might be standardized to locate tumors intraoperatively. Rom J Gastroenterol. 2005. 14:245–248.
14. Abdel-Hakim AM, El-Feel A, Abouel-Fettouh H, Saad I. Laparoscopic vesical diverticulectomy. J Endourol. 2007. 21:85–89.
15. Ponsky JL, King JF. Endoscopic marking of colonic lesions. Gastrointest Endosc. 1975. 22:42–43.
16. Askin MP, Waye JD, Fiedler L, Harpaz N. Tattoo of colonic neoplasms in 113 patients with a new sterile carbon compound. Gastrointest Endosc. 2002. 56:339–342.
17. Arteaga-Gonzalez I, Martín-Malagon A, Fernandez EM, Arranz-Duran J, Parra-Blanco A, Nicolas-Perez D, et al. The use of preoperative endoscopic tattooing in laparoscopic colorectal cancer surgery for endoscopically advanced tumors: a prospective comparative clinical study. World J Surg. 2006. 30:605–611.
18. Lane KL, Vallera R, Washington K, Gottfried MR. Endoscopic tattoo agents in the colon. Tissue responses and clinical implications. Am J Surg Pathol. 1996. 20:1266–1270.
19. Hyman N, Waye JD. Endoscopic four quadrant tattoo for the identification of colonic lesions at surgery. Gastrointest Endosc. 1991. 37:56–58.
20. Nizam R, Siddiqi N, Landas SK, Kaplan DS, Holtzapple PG. Colonic tattooing with India ink: benefits, risks, and alternatives. Am J Gastroenterol. 1996. 91:1804–1808.
21. Shatz BA, Weinstock LB, Swanson PE, Thyssen EP. Long-term safety of India ink tattoos in the colon. Gastrointest Endosc. 1997. 45:153–156.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download