Abstract
Purpose
Animal tumor models are important for the evaluation of novel therapeutic modalities. Since the initial report of an orthotopic bladder tumor model, several modifications have been proposed to improve the tumor take rate. Here we compared the HCl-pretreated and electrocauterization-pretreated orthotopic murine bladder tumor models.
Materials and Methods
MBT-2 murine bladder cancer cells were transurethrally implanted in the bladder of syngeneic C3H/He mice. The mice were divided into three groups according to pretreatment methods (electrocautery, HCl, and control group) and were subjected to pretreatment before instillation of MBT-2 tumor cells into the bladder. Mice were sacrificed on day 21, and bladders were harvested, weighed, and examined histopathologically.
Results
The tumor take rate of the control, electrocautery, and HCl groups was 0%, 54%, and 100%, respectively. The tumor take rate of the HCl group was significantly higher than that of the control group (p<0.01) and the electrocautery group (p=0.01). Pathologic reports revealed that all established bladder tumors were high-grade papillary urothelial carcinomas.
The gold standard of treatment for patients with non-muscle-invasive bladder cancer is transurethral resection. However, the high rate of recurrence or progression presents a major problem despite current intravesical chemotherapy and immunotherapy treatments. It is necessary to evaluate novel intravesical treatment strategies capable of providing improved efficacy and lower toxicity.
Animal cancer models are important for the evaluation of new treatment modalities [1,2]. A suitable bladder tumor model that resembles human disease is essential for evaluation [3]. Orthotopic bladder tumor models simulate the local cancer environment and resemble the behavior of human disease. An ideal orthotopic model should be easy to perform and should allow a high tumor take rate [4].
Soloway [5] described the first transplantable orthotopic bladder tumor model. Since this initial report, several modifications have been proposed to improve the technique and increase the success rate of orthotopic bladder tumor implantation to tumor take rates of 30 to 100% [4,6,7]. Here we compared the tumor take rate of hydrochloric acid (HCl)-pretreated and electrocauterization-pretreated orthotopic murine bladder tumor models.
The MBT-2 murine bladder cancer cell line was originally provided by Dr. Koh (Korea Advanced Institute of Science and Technology, Daejeon, Korea). MBT-2 is a poorly differentiated murine bladder cancer cell line derived from a transplantable N-[4-(5-nitro-2-furyl)-2-thiazolyl] formamide-induced bladder cancer in a female C3H/He mouse. The cells were cultured in Roswell Park Memorial Institute-1600 medium with 10% fetal bovine serum (KDR Biotech Co., Seoul, Korea) and 100 µg/ml streptomycin (Chong Kun Dang, Seoul, Korea) in a 5% CO2 atmosphere at 37℃. The culture medium was replaced every other day, and subculture was performed when the cellular confluence reached 90%. Cells were harvested from subconfluent cultures by trypsinization and were washed in serum-free medium. Single cell suspensions with >90% cell viability were determined by Trypan blue exclusion. The cells were resuspended in phosphate-buffered saline (PBS; KDR Biotech Co.) before injection.
Six-week-old female C3H/He mice were purchased from Orient Bio Inc. (Seongnam, Korea) and raised for 2 weeks. All animal experimental procedures were approved by the Kangbuk Samsung Hospital Animal Care and Use Committee.
Animals were divided into three groups: control group, electrocautery group, and HCl group. The control group had 5 mice, whereas the electrocautery and HCl groups had 11 mice each. Mice were anesthetized with 0.02 ml/100 g intramuscular injection of a 1:2 mixture of tiletamine/zolazepam (Zoletil-50, Virbac, Carros cedex, France) and xylazine HCl (Rompun, Bayer Korea Ltd, Seoul, Korea). Intramuscular injection of 20 mg/kg of cefotetan (Yamatetan, Jeil Pharmaceutical Co., Seoul, Korea) was repeated every 12 hours for 3 days after inoculation.
After anesthesia, a 24-gauge intravenous catheter was inserted into the bladder through the urethra. MBT-2 cells (1.2×106) in 50 µl of medium were instilled. The urethra was then ligated immediately after catheter removal by use of 4-0 silk. The cells were left to dwell within the bladder for 1 hour, followed by removal of the urethral ligature to allow voiding.
After anesthesia, a 24-gauge intravenous catheter was inserted into the bladder through the urethra. A metal electrode was inserted in the bladder through the catheter, and the tip of the electrode contacted the bladder mucosa. With the animal on a grounding plate, a monopolar electrocautery current was applied for 1 second. The electrode was removed and 1.2×106 MBT-2 cells were instilled. The urethra was ligated immediately to allow the cells to dwell in the bladder for 1 hour before voiding, as described for the control mice.
After anesthesia, a 24-gauge intravenous catheter was inserted into the bladder through the urethra and 30 µl of 0.1 N HCl was injected into the bladder through the catheter. The acid solution was allowed to remain in the bladder for 15 seconds before replacement with 30 µl of 0.1 N NaOH for 15 seconds. The bladder was then drained and flushed with sterile PBS. MBT-2 cells (1.2×106) in 50 µl of medium were instilled and the urethra was ligated immediately to allow the cells to dwell in the bladder for 1 hour before voiding as described for the control mice.
On day 21, all mice were sacrificed by CO2 euthanasia. No mice had died due to complications during the experimental period. Each bladder was harvested, weighed, and subjected to histopathological examination. The presence or absence of tumors was noted, along with the morphology and tumor size and weight. The tumor volume was determined by using the formula for a rational ellipse (0.5236×l×w×h) [8]. Tissue from bladders was stained with hematoxylin-eosin for histologic examination. Statistical analyses were carried out by using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) for Windows. Differences in tumor volume and weight between the two groups were compared by using Student's t-test, and the tumor take rate was compared by using the Pearson chi-square test. A p-value<0.05 was considered to be statistically significant.
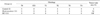
In the control group, a single cell suspension of 1.2×106 MBT-2 cells instilled into the bladder did not result in tumor establishment. In contrast, bladder tumors were established in 6 of 11 mice in the electrocautery group and 11 of 11 mice in the HCl group. The tumor take rate of the electrocautery (54%, p=0.03) and HCl (100%, p<0.01) groups were higher than that of the control group (0%). Between two experimental groups, the tumor take rate of the HCl group was significantly higher than that of electrocautery group (p=0.01) (Table 1).
The average tumor volume of the electrocautery and HCl groups were 221.55±118.63 mm3 and 268.52±171.14 mm3. There was no statistic difference between two groups (p=0.35) (Fig. 1).
The average tumor weight of the electrocautery (243.2±91.1 mg) and HCl (278.5±179.9 mg) groups also did not differ significantly (p=0.40).
The pathologic reports for all the established bladder tumors were high grade papillary urothelial carcinoma, same as MBT-2 cell line. In the electrocautery group, all the established tumors were limited to the mucosal and submucosal layer (pT1). In the HCl group, tumors from nine mice were limited to the mucosal and submucosal layer (pT1), whereas two showed invasion into the muscular layer (pT2) (Table 1) (Fig. 2).
Treatment for localized bladder cancer includes transurethral tumor resection. Despite intravesical immunotherapy or chemotherapy, up to 70% of patients with superficial bladder cancer develop recurrent tumors. Novel therapeutic agents are needed to improve the outlook of bladder cancer treatment.
Animal cancer models are important for evaluating the effects of different therapeutic interventions [1,2]. A suitable bladder tumor model should resemble human disease in both histology and behavior [3]. Thus, the tumor should grow intravesically and should consist of pure urothelial cancer cells (transitional cells). Furthermore, non-muscle-invasive tumors are preferable, because 70 to 80% of human bladder tumors are non-muscle-invasive. In addition, the establishment of the model should be technically easy to develop within a reasonable time period.
Currently, there are three fundamental murine bladder tumor models: chemically induced bladder cancer [9-12], the xenograft model (transplantation of human transitional cell carcinoma (TCC) into immunodeficient mice) [13-15], and the syngeneic tumor model (transplantation of carcinogen-induced bladder cancer cells into syngeneic, immunocompetent mice) [5,16-19]. Chemical induction of primary bladder tumors requires several months, with both TCC and squamous carcinoma being induced, and tissues other than urothelium also being transformed [20-23]. The xenograft model, which uses immunodeficient nude mice, is compromised in its ability to develop an adequate immune reaction to an immunological stimulus [24]. In the syngeneic tumor model, the heterotopic tumor model is not suitable owing to its dissimilarities in biological behavior compared to the clinical disease [3].
The orthotopic bladder tumor model resembles the human situation resulting from seeding of viable tumor cells to the bladder mucosa. [3,4]. However, the orthotopic technique cannot guarantee a high tumor take rate in usual settings. The bladder mucosa and the GAG layer act as natural protective layers against external insults, and this may result in a poor tumor take rate [4,25].
Soloway [5] described the first transplantable orthotopic bladder tumor model. With the administration of N-methyl-N-nitrosourea before tumor instillation, they reported a tumor take rate of about 60%. However, only extravesically implanted tumors were obtained with this technique [6]. Several modifications have been proposed to improve the techniques and the success rate of orthotopic bladder tumor implantation. Shapiro et al. [6] reported a tumor take rate of about 60% with electrocauterization-induced mucosal injury before tumor instillation. In this modification, extravesical tumors were reduced to 24%. Similar results were reported by Sindhwani et al. [26], who described a 73% tumor take rate and about 30% extravesical tumors with electrocautery pretreatment. Pretreatment with HCl/KOH resulted in a tumor take rate of about 80 to 90%, with about 20% extravesical tumors [27,28].
In the HCl pretreatment model, it may be possible to expose the entire bladder wall to acid, leading to extensive mucosal injury. Chan et al. [4] reported a high mortality rate and extensive bladder wall inflammation in the HCl pretreatment group. The high mortality rate of this model is a serious pitfall, however, and the presence of extensive inflammation decreases the similarity of the model to human disease, because a considerable portion of the human bladder wall remains grossly normal during transurethral resection. We note that there are some technical differences between the previously reported HCl pretreatment model and the model we reported here. Chan et al. [4] filled the bladder with 100 µl of 0.1 N HCl solution, whereas we used 30 µl. Also, they did not use antibiotic agents. In our experiment, the HCl pretreatment group experienced no mortality, and microscopic examination revealed the absence of inflammation or ulceration in the bladder. Several other reports have also described the absence of a high mortality or morbidity rate in HCl pretreatment models [27-29]. Thus, the high mortality rate and extensive mucosal injury did not seem to be correlated with HCl pretreatment, but may rather reflect technical issues that could be corrected with certain procedural modifications and cautions.
In our study, the HCl pretreatment group showed a 100% tumor take rate with 18% muscle invasion, which was superior to both the control and the electrocautery pretreatment groups. The tumor take rate was superior to those in previous reports, and the low muscle invasion rate was comparable to that reported in other studies.
The orthotopic murine bladder cancer model is ideal for the evaluation of novel intravesical therapy. But, on account of the low tumor take rate, several modifications have been proposed. On the basis of our findings, we suggest that the HCl pretreatment model is the preferable murine bladder cancer model for evaluating further therapeutic interventions.
Figures and Tables
FIG. 1
Gross images of the bladder in each experimental group. (A) Normal bladder from the control group. (B) Bladder tumor from the electrocautery group. (C) Bladder tumor from the HCl group.

FIG. 2
(A) An example from the electrocautery group. The tumor invades into the submucosa but does not involve proper muscle. The tumor shows a solid growth pattern with high-grade urothelial carcinoma cells (H&E, ×100). (B) An example from the HCL group. The tumor shows a solid infiltrative growth pattern with high-grade urothelial carcinoma cells. The tumor invades into the proper muscle. (H&E, ×100).

References
1. Ratliff TL. Role of animal models in understanding intravesical therapy with bacille Calmette-Guerin. Clin Infect Dis. 2000. 31:Suppl 3. S106–S108.
2. McCue PA, Gomella LG, Veltri RW, Marley GM, Miller MC, Lattime EC. Development of secondary structure, growth characteristics and cytogenetic analysis of human transitional cell carcinoma xenografts in scid/scid mice. J Urol. 1996. 155:1128–1132.
3. Xiao Z, McCallum TJ, Brown KM, Miller GG, Halls SB, Parney I, et al. Characterization of a novel transplantable orthotopic rat bladder transitional cell tumour model. Br J Cancer. 1999. 81:638–646.
4. Chan ES, Patel AR, Smith AK, Klein JB, Thomas AA, Heston WD, et al. Optimizing orthotopic bladder tumor implantation in a syngeneic mouse model. J Urol. 2009. 182:2926–2931.
5. Soloway MS. Intravesical and systemic chemotherapy of murine bladder cancer. Cancer Res. 1977. 37(8 Pt 2):2918–2929.
6. Shapiro A, Kelley DR, Oakley DM, Catalona WJ, Ratliff TL. Technical factors affecting the reproducibility of intravesical mouse bladder tumor implantation during therapy with Bacillus Calmette-Guerin. Cancer Res. 1984. 44:3051–3054.
7. Horinaga M, Harsch KM, Fukuyama R, Heston W, Larchian W. Intravesical interleukin-12 gene therapy in an orthotopic bladder cancer model. Urology. 2005. 66:461–466.
8. Janik P, Briand P, Hartmann NR. The effect of estrone-progesterone treatment on cell proliferation kinetics of hormone-dependent GR mouse mammary tumors. Cancer Res. 1975. 35:3698–3704.
9. Soloway MS. Single and combination chemotherapy for primary murine bladder cancer. Cancer. 1975. 36:333–340.
10. Williams PD, Murphy GP. Experimental bladder tumor induction, propagation, and therapy. Urology. 1976. 8:39–42.
11. Park HS, Cheon J, Yoon DK, Koh SK, Kim HK. The changes of histopathology, proliferation activity, and nuclear DNA content N-butyl-N-(4-hydroxybuty1) nitrosamine (BBN) induced bladder cancer in rats. Korean J Urol. 1995. 36:683–691.
12. Jin JH, Lee GH, Kim HJ. Chemopreventive effect of aspirin on N-Butyl-N-(4-hydroxybutyl) nitrosamine induced preneoplastic lesions in rat bladder. Korean J Urol. 2001. 42:631–635.
13. Hubbell HR, Kvalnes-Krick K, Carter WA, Strayer DR. Antiproliferative and immunomodulatory actions of beta-interferon and double-stranded RNA, individually and in combination, on human bladder tumor xenografts in nude mice. Cancer Res. 1985. 45:2481–2486.
14. Huland H, Otto U, von Paleske A. Chemotherapy and human bladder carcinoma transplanted into NMRI nu/nu mice. J Urol. 1985. 134:601–606.
15. Russell PJ, Raghavan D, Gregory P, Philips J, Wills EJ, Jelbart M, et al. Bladder cancer xenografts: a model of tumor cell heterogeneity. Cancer Res. 1986. 46(4 Pt 2):2035–2040.
16. Ratliff TL, Gillen D, Catalona WJ. Requirement of a thymus dependent immune response for BCG-mediated antitumor activity. J Urol. 1987. 137:155–158.
17. Hudson MA, Ritchey JK, Catalona WJ, Brown EJ, Ratliff TL. Comparison of the fibronectin-binding ability and antitumor efficacy of various mycobacteria. Cancer Res. 1990. 50:3843–3847.
18. Lee KE, Weiss GH, O'Donnell RW, Cockett AT. Reduction of bladder cancer growth in mice treated with intravesical Bacillus Calmette Guerin and systemic interleukin 2. J Urol. 1987. 137:1270–1273.
19. Lee SJ, Chung CE, Kim SW, Lee CB, Kang SH, Cho YH, et al. Efficacy of paclitaxel-loaded bioadhesive drug deliver system based on glyceryl monooleate nanoparticle in an orthotopic murine bladder cancer model. Korean J Urol. 2004. 45:817–822.
20. Erturk E, Cohen SM, Price JM, Bryan GT. Pathogenesis, histology, and transplantability of urinary bladder carcinomas induced in albino rats by oral administration of N-(4-(5-nitro-2-furyl)-2-thiazolyl)formamide. Cancer Res. 1969. 29:2219–2228.
21. Erturk E, Price JM, Morris JE, Cohen S, Leith RS, Von Esch AM, et al. The production of carcinoma of the urinary bladder in rats by feeding N-[3-(5-nitro-2-furyl)-2-thiazolyl]formamide. Cancer Res. 1967. 27:1998–2002.
22. Herman CJ, Vegt PD, Debruyne FM, Vooijs GP, Ramaekers FC. Squamous and transitional elements in rat bladder carcinomas induced by N-butyl-N-4-hydroxybutyl-nitrosamine (BBN). A study of cytokeratin expression. Am J Pathol. 1985. 120:419–426.
23. Oyasu R, Samma S, Ozono S, Bauer K, Wallemark CB, Homma Y. Induction of high-grade, high-stage carcinomas in the rat urinary bladder. Cancer. 1987. 59:451–458.
24. Gunther JH, Jurczok A, Wulf T, Brandau S, Deinert I, Jocham D, et al. Optimizing syngeneic orthotopic murine bladder cancer (MB49). Cancer Res. 1999. 59:2834–2837.
25. Parsons CL, Stauffer C, Schmidt JD. Impairment of antibacterial effect of bladder surface mucin by protamine sulfate. J Infect Dis. 1981. 144:180.
26. Sindhwani P, Hampton JA, Baig MM, Keck R, Selman SH. Curcumin prevents intravesical tumor implantation of the MBT-2 tumor cell line in C3H mice. J Urol. 2001. 166:1498–1501.
27. Chin J, Kadhim S, Garcia B, Kim YS, Karlik S. Magnetic resonance imaging for detecting and treatment monitoring of orthotopic murine bladder tumor implants. J Urol. 1991. 145:1297–1301.
28. Satoh H, Morimoto Y, Arai T, Asanuma H, Kawauchi S, Seguchi K, et al. Intravesical ultrasonography for tumor staging in an orthotopically implanted rat model of bladder cancer. J Urol. 2007. 177:1169–1173.
29. Siemens DR, Austin JC, See WA, Tartaglia J, Ratliff TL. Evaluation of gene transfer efficiency by viral vectors to murine bladder epithelium. J Urol. 2001. 165:667–671.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download