Abstract
Purpose
To assess the clinical reliability of the Bosniak IIF category and to determine the proper radiologic follow-up duration and intervals for category IIF complex renal cysts.
Materials and Methods
We studied 201 patients with category IIF renal cysts from January 1996 to January 2011. Renal cyst progression to category III was defined as an increase in complexity of the cyst in follow-up radiologic studies. We monitored radiologic changes and progression of renal cysts during the follow-up period and analyzed the pathologic results of those patients who were treated surgically.
Results
At a mean follow-up of 20 months, only 14 cases (7%) showed evidence of progression to stage III, with a mean time to progression of 11 months (range, 3 to 65 months). There were no significant differences in age, gender, cyst size, or change in cyst size between the progressive and non-progressive groups. Of 12 cases treated surgically, 10 cases (83.3%) showed renal cell carcinoma with pT1 stage, and there was no recurrence during postoperative follow-up of 23 months. Of the 187 patients without radiologic progression, 23 cases were treated surgically, and all of them showed benign cysts.
Conclusions
The IIF category showed significant clinical reliability by a low rate of radiologic progression and a high rate of malignancy in the radiologic progressive group but a low rate of malignancy in the non-progressive group. Although it is hard to decide on a proper follow-up duration because of the variable time to progression, too frequent follow-up study seems to be unnecessary considering that most malignant cases were of a low stage.
Renal cysts are common lesions. More than 50% of the population aged 50 years and older has renal cysts [1], and most simple renal cysts do not require further evaluation or intervention because they are harmless [2]. Due to advances in and the widespread use of abdominal ultrasonography, abdominal computed tomography (CT), and magnetic resonance imaging (MRI) as diagnostic tools [3], the incidence of complex renal cysts and cystic renal cell carcinoma has increased in recent years. Advanced imaging studies have brought early diagnosis and early treatment as a result. However, they have also brought unnecessary surgeries and post-operative complications for benign renal cysts. Therefore, it is very important to differentiate cystic renal cell carcinoma from benign renal cysts during the pre-operative work-up [3]. Abdominal CT or MRI studies are used to differentiate between simple renal cysts and cystic renal malignancies. However, it is still a major challenge to recognize the differences between them.
Bosniak suggested a classification system for complex renal cysts in 1986 [4], and his classification system is the one most widely used to evaluate renal cysts [2]. Cysts are classified into four different levels for patient management: simple renal cysts (category I), benign renal cysts with complications but not in need of surgery (category II), potentially malignant renal cysts in need of surgery (category III), and cystic renal cell carcinomas (category IV) [3]. However, the controversy and difficulty lies in those complex cystic renal masses that lie between Bosniak II and III [2,5]. To address this problem and based on the clinical experience of Bosniak, the IIF categorization was first suggested in 1993 for lesions that are more complex than a category II cyst but are still thought to be benign and require only serial imaging to confirm stability [6,7].
Presently, there is a consensus that radiologic surveillance with intervention upon increasing complexity is a safe and effective protocol for managing category IIF lesions [8], but the proper radiologic follow-up duration and intervals for these lesions remain unproven. Some reports of the clinical outcomes of category IIF complex renal cysts in Western countries have been published [8], but no reports in Korea have been published. Therefore, we retrospectively evaluated the pathological and clinical outcomes of category IIF complex renal cysts to assess the clinical reliability of the IIF category and to determine the proper radiologic follow-up duration and intervals for these lesions.
After institutional review board approval was received, from January 1996 to January 2011, patients were identified retrospectively from a urology billing database by using diagnostic codes for renal cysts, renal masses, and renal neoplasms as well as from a preexisting radiology database by using the key words Bosniak and cyst. A total of 5,946 patients were diagnosed with cystic renal disease. Among them, 278 patients were diagnosed with category IIF cysts by CT imaging. Seventy-seven were not included in the study owing to a lack of radiologic follow-up, leaving 201 patients for the final analysis.
Diagnosis of all the patients was done by using a kidney spiral CT protocol or an abdominal-pelvic contrast CT protocol. The CT examinations that took place at our institution were performed by using a 4-channel LightSpeed QX/I MDCT scanner (GE Medical Systems, Milwaukee, WI, USA) or a 16-channel Sensation 16 MDCT scanner (Siemens Medical System, Erlangen, Germany). In the abdominal pelvic contrast CT protocol, after unenhanced images were acquired, arterial phase and delayed phase scanning were performed. In the kidney spiral CT protocol, unenhanced images were acquired first after the patients ingested E-Z-CAT oral contrast agent (2% barium sulfate suspension) 30 minutes before the examination. Then, corticomedullary images were acquired 30 seconds after bolus injection of Ultravist 300 (iopromide) or Lopamiro 300 (iopamidol) (Braco, Milano, Italy) intravenous contrast material into the antecubital vein with the aorta, renal artery, and renal cortex highlighted. The section thickness was 2.5 to 5.0 mm and the total amount of contrast material was a maximum of 160 ml at a rate of 3 ml/s. Early excretory phase scans were obtained approximately 120 to 150 seconds after contrast injection when the vena cava and the renal vein were highlighted and the renal pelvis began contrast pooling.
Category IIF lesions were defined as those being more complex than a category II cyst but still thought to be benign and to require only serial imaging to confirm stability [6,7]. They could contain an increased number of septa or have minimal thickening of the wall or septa, and whether there was measurable enhancement of these structures was often uncertain [9]. All category IIF lesions were diagnosed by a single uroradiologist.
Upon chart review, follow-up radiologic and pathologic data were recorded. The radiologic data were surveyed for date of radiologic study, change in lesion size, and interval change in complexity. Cyst progression was defined as an increase in cyst complexity diagnosed by the radiologist, but an increase in cyst size was not considered progression.
Differences between the radiologic progressive group and non-progressive group were compared. Patients received surgical treatment due to progression into category III, and this group included those who did not have progression but underwent surgery on their own account. Their pathological outcomes were recorded, including benign or malignant histology, histological subtype, and pathological stage. Marsupialization was included in the procedure for those in the non-progressive group who underwent surgery. Fluid cytology and cyst wall were tested by marsupialization to determine whether the cysts were benign or malignant.
To analyze the differences between the radiologic progressive group and the non-progressive group, Student's t-test was used for continuous variables, and chi-square test was used for categorical variables. A p-value less than 0.05 was considered statistically significant. Data were analyzed by using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA).
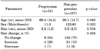
The clinical characteristics of all patients are shown in Table 1. During the mean follow-up period of 20 months (range, 1 to 141 months; median, 12 months), 154 cysts (77%) showed no changes in size, 35 (17%) increased in size, and 12 (6%) decreased in size. Fourteen cases (7%) showed renal cyst progression and the mean time to progression was 11 months (range, 3 to 65 months; median, 6 months). There were no significant differences between the progressive group and the non-progressive group with regard to age (p=0.948), gender (p=0.292), size of cyst (p=0.534), or change in size during follow-up (p=0.494) (Table 2).
Among 14 patients with radiologic progression, 2 of 14 cases refused surgery; the remaining 12 cases were treated surgically. Ten cases (83.3%) were found to be malignant (Fig. 1). Of these malignant cases, six were T1a and four were T1b. Six of the tumors had clear cell histology, three had a papillary histology, and one had chromophobe histology (Table 3). A representative case with radiologic progression is described in Fig. 1. All of the 10 patients with malignancy were found with no post-operative recurrence for an average of 23 months (range, 3 to 48 months; median, 18 months).
Of the 187 patients without radiologic progression, 23 cases were treated surgically. Two patients had lesions that increased only in size (1.4 to 1.8 cm and 13.7 to 14.8 cm) and underwent surgery on their own account. Three patients underwent a nephrectomy while being treated surgically for other disease. The remaining 18 cases were treated surgically owing to the patient's request: 13 cases by nephrectomy and 10 by renal cyst marsupialization. All 23 patients who underwent surgery were reported to have benign cysts. No post-operative malignant changes were observed for an average of 30 months (range, 1 to 84 months; median, 32 months).
The Bosniak classification system is used to diagnose and manage complex renal cysts. If the category IIF designation of the Bosniak classification system is accurate, it can be used to predict minimal progression in category IIF lesions and a low malignancy rate [8]. In our study, during the mean follow-up period of 20 months, 14 cases (7%) showed renal cyst progression. The mean time to progression was 11 months (range, 3 to 65 months; median, 6 months). This is slightly lower than the 14.8% progression rate in an evaluation of radiologic follow-up of 81 category IIF lesions with a median follow-up of 15 months [8]. Also, 23 cases without progression were treated surgically in our study and all of them were reported as benign cysts. The malignancy rate in surgically treated category IIF lesions is historically 0 to 25%, but the previous studies reporting these values were done in very small populations [10,11]. This supports the clinical reliability of the Bosniak IIF category. The malignancy rate in surgically treated category III lesions is historically 25 to 100% [8]. If all historically reported category III lesions with a pathologically proven diagnosis are summed, there is an overall 51% malignancy rate [12]. In our study, 12 of 14 cases of progression were treated surgically except for the two cases who refused surgery; 10 (83.3%) of these 12 cysts were found to be malignant. The malignancy rate in this study was higher than the historically reported malignancy rate. This further supports the clinical reliability of the Bosniak IIF category.
No clear guidelines concerning the proper radiologic follow-up duration and intervals have been proposed, but if increasing complexity is found by continuous radiologic studies, exploratory surgery is recommend to rule out malignancy [8]. Most category IIF patients are not surgically treated; therefore, additional follow-up studies are needed to confirm that the cysts in these patients remain stable and benign. In our study, the average time to progression was 11 months (range, 3 to 65 months; median, 6 months). The longest progression time of 65 months (5.4 years) indicates that follow-up studies should be performed for at least 5 years. This is because renal cysts show a slow growth pattern [9].
It can be argued that category IIF cysts should be surgically removed, for example, in young patients who do not want more follow-up studies [9]. However, surgery is not necessary for all patients; in our study, all 23 patients who underwent surgery had benign cysts. Most cases of malignancy in surgically treated progressive groups are low-stage renal cell carcinoma. The prognosis of these carcinomas is satisfactory compared with other renal malignancies owing to the low metastatic rate [13-16]. Therefore, delayed diagnosis of several malignancies did not have severe consequences or adversely affect patients' outcome. Thus, for elderly patients in poor physical condition, follow-up study is recommended rather than surgery. For young patients, too frequent follow-up study would be unnecessary.
This study had a few limitations. Because our study was retrospective and the cases were collected over 10 years, the radiologic studies were performed on a variety of helical and conventional CT scanners. In addition, the type and amount of intravenous contrast material also varied. Second, intervention was influenced by clinical parameters such as patient age and physical condition. Although the Bosniak classification system is based on imaging findings, it can add variability to managing cases by affecting clinical parameters. Lastly, the sample size was small because some patients moved away or transferred to another hospital, resulting in follow-up loss. Additional patients and a prolonged follow-up period are needed in future studies.
We could confirm the clinical reliability of the IIF category on the basis of the fact that the category IIF patients showed a low radiologic progression rate (7%), and those patients who progressed to category III had a high malignancy rate (83.3%), whereas a low rate (0%) of malignancy was found in the non-progressive group. Although it is hard to decide on a proper follow-up duration because of the variable time to progression, too frequent follow-up study would be unnecessary considering that most malignant cases were of a low stage. Nevertheless, our study has the advantage of a large cohort in which all cases were collected from a single institution. To our knowledge, this study is the first study to evaluate the pathological and clinical outcomes of category IIF complex renal cysts in Korean patients.
Figures and Tables
 | FIG. 1A 69-year-old man with a category IIF cystic lesion in the right kidney. (A) Initial contrast-enhanced transverse computed tomography scan depicts a 2.8-cm cystic mass that contains multiple minimally smooth thickening of septa. (B) On follow-up 9 months later, the cystic renal mass contains grossly thickened and irregular septa in which there is measurable enhancement (white arrow). On the basis of these findings, the lesion was reclassified as a category III cyst. (C) The patient underwent radical nephrectomy and the lesion was found to be a pT1 stage conventional renal cell carcinoma with focal hemorrhage (H&E, ×400). |
References
1. Kissane JM. The morphology of renal cystic disease. Perspect Nephrol Hypertens. 1976. 4:31–63.
2. Kim JC. Usefulness of the Bosniak classification in cystic renal mass on CT. J Korean Radiol Soc. 1999. 40:555–562.
3. Park HS, Jeong KS, Cheon J, Yoon DK, Jeong KB. The clinical significance of Bosniak classification in cystic renal masses: usefulness of preoperative computerized tomography in cystic renal masses. Korean J Urol. 1994. 35:498–503.
4. Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986. 158:1–10.
5. Siegel CL, McFarland EG, Brink JA, Fisher AJ, Humphrey P, Heiken JP. CT of cystic renal masses: analysis of diagnostic performance and interobserver variation. AJR Am J Roentgenol. 1997. 169:813–818.
6. Bosniak MA. Problems in the radiologic diagnosis of renal parenchymal tumors. Urol Clin North Am. 1993. 20:217–230.
7. Bosniak MA. Diagnosis and management of patients with complicated cystic lesions of the kidney. AJR Am J Roentgenol. 1997. 169:819–821.
8. O'Malley RL, Godoy G, Hecht EM, Stifelman MD, Taneja SS. Bosniak category IIF designation and surgery for complex renal cysts. J Urol. 2009. 182:1091–1095.
9. Israel GM, Bosniak MA. Follow-up CT of moderately complex cystic lesions of the kidney (Bosniak category IIF). AJR Am J Roentgenol. 2003. 181:627–633.
10. Graumann O, Osther SS, Osther PJ. Characterization of complex renal cysts: a critical evaluation of the Bosniak classification. Scand J Urol Nephrol. 2011. 45:84–90.
11. Smith AD, Remer EM, Cox KL, Lieber ML, Allen BC, Shah SN, et al. Bosniak category IIF and III cystic renal lesions: outcomes and associations. Radiology. 2012. 262:152–160.
12. Curry NS, Cochran ST, Bissada NK. Cystic renal masses: accurate Bosniak classification requires adequate renal CT. AJR Am J Roentgenol. 2000. 175:339–342.
13. Bielsa O, Lloreta J, Gelabert-Mas A. Cystic renal cell carcinoma: pathological features, survival and implications for treatment. Br J Urol. 1998. 82:16–20.
14. Smaldone MC, Uzzo RG. Active surveillance: a potential strategy for select patients with small renal masses. Future Oncol. 2011. 7:1133–1147.
15. Eble JN, Bonsib SM. Extensively cystic renal neoplasms: cystic nephroma, cystic partially differentiated nephroblastoma, multilocular cystic renal cell carcinoma, and cystic hamartoma of renal pelvis. Semin Diagn Pathol. 1998. 15:2–20.
16. Murad T, Komaiko W, Oyasu R, Bauer K. Multilocular cystic renal cell carcinoma. Am J Clin Pathol. 1991. 95:633–637.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download