Abstract
Purpose
Typically in Korea, for a standard dose (0.4 mg) of tamsulosin, two low doses (0.2 mg) are administered. The aim of this study was to evaluate and compare the efficacy of tamsulosin (0.2 mg and 0.4 mg) and alfuzosin (10 mg) in the treatment of lower ureteral stones.
Materials and Methods
A total of 141 patients presenting with a single 4- to 10-mm sized lower ureteral stone were randomly assigned to 4 groups. Patients in group 1 (n=41) and group 2 (n=30) received an oral dose of 0.2 mg tamsulosin once and twice daily, respectively, and patients in group 3 (n=36) received a daily oral dose of 10 mg alfuzosin. Patients in group 4 (n=34) received trospium chloride only. The spontaneous passage of stones, the stone expulsion time, and adverse effects were evaluated.
Results
There were no significant differences in patient background, including age, sex, BMI, stone size, stone side, and symptom duration. The spontaneous stone passage rate through the ureter was higher and the stone expulsion time was faster in groups 1, 2, and 3 than in group 4. There were no statistically different changes in groups 1, 2, and 3. The adverse effects observed in all groups were comparable and were mild.
Patients with urinary tract stones account for 20% of urology inpatients [1]. Urinary tract stones remain common, affecting up to 5% of people worldwide [2]. The prevalence of urinary tract stone disease in Korea is steadily rising.
The location (upper, mid, and lower) and size of the stone as well as stone composition and complications are determining factors in the treatment of urinary stones. Treatments are divided into three broad groups: 1) observation and medical therapy, 2) shock wave lithotripsy (SWL) and ureteroscopy, and 3) open surgery, laparoscopic stone removal, or percutaneous antegrade ureteroscopy. Urolithiasis treatment has been shifting to less invasive therapies such as SWL or ureteroscopy. Despite improved treatment, however, the rate of recurrence of urinary tract stones remains high. Tomson [3] reported a 67% and 75% recurrence of urolithiasis within 9 years and 25 years, respectively. Fifty percent of those with urinary tract stones will experience one or more recurrences. Therefore, the initial treatment is very important; no remaining stones should be present and ureteral injury, sepsis, and infection should not occur as a result of the intervention.
For stones 5 to 10 mm in size, analysis of groups yielded an estimate that 47% would pass spontaneously [4]. Various studies of efficient stone expulsion have been done for increasing the stone expulsion rate. The 2007 Guideline for Management of Ureteral Calculi of The American Urological Association (AUA) and the European Association of Urology (EAU) guideline recommend watchful waiting with medical treatment for patients with a stone <10 mm in diameter and well-controlled pain [4].
Currently, non-selective α-blockers such as alfuzosin (10 mg daily) and doxazosin (4 mg daily) and α-1a and α-1d selective α-blockers such as tamsulosin (0.4 mg daily) are used for the spontaneous expulsion of lower ureteral stones or to facilitate stone removal after SWL [5-7]. In Korea and Japan, only tamsulosin 0.2 mg is produced and the administration of the total daily dose of tamsulosin is achieved by the use of two doses of 0.2 mg. This regimen is more onerous and expensive than the use of a single 0.2-mg daily dose and adverse effects such as retrograde ejaculation can be increased. Adverse effects such as dizziness, orthostatic hypotension, headache, and fatigue may occur by taking nonselective α-blockers.
Presently, we compared the impact of 0.2 mg tamsulosin with that of 0.4 mg tamsulosin and 10 mg alfuzosin in patients with lower ureteral stones of 4 to 10 mm in diameter and with controlled pain, with the aim of clarifying the treatment regimen that is superior for spontaneous stone expulsion.
Patients presenting with only one single lower ureteral stone, 4 to 10 mm in size, at the emergency department or urologic clinic at our institution were evaluated for study participation in a prospective manner between September 2008 and June 2011. Patients were enrolled upon diagnosis with normal renal function that did not require hospitalization and intervention for stone removal. The patients were excluded if they met any of following criteria: 1) urinary tract infection, 2) moderate or severe hydronephrosis, 3) hypotension, 4) single kidney, 5) bilateral ureteral stones, 6) history of previous surgery on the ipsilateral ureter, 7) currently taking an α-blocker, steroid, or calcium channel blocker, 8) renal insufficiency, 9) <18 years of age, and 10) pregnant or lactating woman. A total of 156 patients were enrolled and 15 patients were excluded. The randomization list was generated by using the permuted block method and was concealed from the patient-enrolling investigators (confined with a doctor assisting in the procedure but not participating in the study). When a patient met the inclusion and exclusion criteria, the assigned treatment was disclosed.
A total of 141 patients were classified into four treatment groups. All patients received an initial treatment of 90 mg diclofenac by intramuscular injection and 5 mg cimetropium bromide by intravenous injection, with a second dose after 30 minutes or 1 hour if necessary. All patients received trospium chloride (50 mg, tablet) every 8 hours until their next visit. Patients in group 1 (n=41) and group 2 (n=30) received an oral dose of 0.2 mg tamsulosin once or twice daily, respectively. Patients in group 3 (n=36) received a daily oral dose of 10 mg alfuzosin. Patients in group 4 (n=34) received trospium chloride.
Before the treatment, urinalysis, blood urea nitrogen, creatinine level, plain kidney ureter and bladder radiographs (KUB), intravenous pyelogram (IVP), or ultrasound views of the kidney, ureter, and bladder were obtained for all patients. If the stone was not identified exactly, unenhanced computed tomography (CT) was obtained. Similar measurements for stones 5 to 10 mm and 2 to 13 mm in size have been reported between non-contrast spiral CT and plain KUB for distal ureteral stones [8,9]. Therefore, we evaluated stone location and size by using KUB images and noncontrast CT.
Follow-up visits were performed on days 7, 14, 21, and 28. At each follow-up visit, the spontaneous passage of stones, the stone expulsion time, and side effects were evaluated and every patient underwent a plain KUB, ultrasonography, urinalysis, and determination of serum creatinine. Also, patients were asked to observe for stone passage during urination; if they had not noticed stone expulsion with a stone-free ureter, the mean date between the date of the last positive image study and the most recent follow-up was recorded.
The study medications were discontinued after spontaneous stone expulsion, intervention, or at the end of the study period. No expulsion of the stone at the end of the study and intervention before the end of the study as the result of uncontrolled pain or other serious events were considered failed therapy.
Statistical analysis was performed by using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) software. One-way analysis of variance was used to compare continuous variables between the four groups, and different continuous variables between the two groups were tested by using Student's t-test. Nominal parameters were analyzed by using Pearson's chi-square and Fischer's exact test. A p-value<0.05 was considered significant.
The mean stone size was 5.49±1.31 mm for group 1, 5.73±1.57 mm for group 2, 5.81±1.26 mm for group 3, and 5.59±1.44 mm for group 4. There were no statistically significant differences between the four groups with respect to age, sex, body mass index, stone size, stone localization, or symptom duration. The demographic data are summarized in Table 1.
The calculi passed through the ureter spontaneously in 32 patients in group 1 (78.0%), 23 patients in group 2 (76.7%), 27 patients in group 3 (75.0%), and 16 patients in group 4 (47.1%). A statistically significant difference was noted between groups 1 and 4 (p=0.008), groups 2 and 4 (p=0.021), and groups 3 and 4 (p=0.026), whereas no significant difference was recorded between groups 1 and 2 (p=1.000), groups 1 and 3 (p=0.793), and groups 2 and 3 (p=1.000). The demographic data are summarized in Table 2.
The mean time to stone expulsion was 8.47±5.51 days in group 1, 7.82±5.08 days in group 2, 8.22±5.96 days in group 3, and 13.56±6.49 days in group 4. A statistically significant difference was noted between groups 1 and 4 (p=0.007), groups 2 and 4 (p=0.004), and groups 3 and 4 (p=0.009), whereas no significant difference was recorded between groups 1 and 2 (p=0.661), groups 1 and 3 (p=0.870), and groups 2 and 3 (p=0.803). The demographic data are summarized in Table 2.
No severe complications were recorded in the four groups. Two patients (4.9%) in group 1 and two patients (6.7%) in group 2 recorded retrograde ejaculation. One patient (2.4%) in group 1, one patient (3.3%) in group 2, and two patients (5.6%) in group 3 recorded one episode of orthostatic hypotension that did not require suspension of the therapy. There were no statistically significant differences between the groups in terms of retrograde ejaculation, orthostatic hypotension, headache, dizziness, diarrhea, fatigue, nausea, or vomiting (p>0.05). The demographic data are summarized in Table 3. During the course of the study, none of the patients experienced intractable pain, fever, or severe hydronephrosis that required urgent intervention. A total of 43 patients who did not pass the stone within 4 weeks were treated by using SWL or ureteroscopy.
Various treatment options are considered for the management of lower ureteral stones, including open ureterolithotomy, ureteroscopic lithotripsy (URS), and SWL. According to the 2007 Guideline for the Management of Ureteral Calculi of the AUA and the EAU guideline, URS stone-free rates were significantly better than SWL rates for distal ureteral stones ≤10 mm and >10 mm [4]. The availability of this modality and physician experience were considered. Complications such as sepsis, stricture, ureteral injury, and urinary tract infection are the most relevant complications.
Spontaneous stone passage was often reported without active treatment including URS and SWL. One study reported spontaneous expulsion in 25 to 53% of cases for distal ureteral stones 5 to 10 mm in diameter [10]. Another study reported spontaneous passage of 68% of stones <5 mm in diameter and 47% of stones 5 to 10 mm in diameter [5]. Ureteric calculi more than 10 mm in diameter should be removed by emergency URS or medical expulsion treatment (MET), because large calculi tend to impact in the ureter and are unlikely to migrate in the distal region [11]. More distal stones are more likely to pass spontaneously, and Miller and Kane [12] reported that the interval to stone passage was highly variable and dependent on stone size and location. The hazard of expulsion at any time was 3-fold higher for stones located at the ureterovesical junction than for those in the distal part of the ureter [13]. Accordingly, the most important factors in predicting the likelihood of spontaneous stone expulsion are stone size and stone location [14].
The ureter demonstrates two continuous thin muscle layers with a loosely spiraled internal layer and a more tightly spiraled external layer. In the lower third of the ureter, a third outer longitudinal layer is present. The lower ureter is composed of transitional epithelium, a connective tissue layer, and three layers of smooth muscle [15]. Ureteral peristalsis is initiated by spontaneous activity of the renal pelvis pacemaker cell and is essentially regulated by the myogenic mechanism and neurogenic factors; thereafter, electrical and mechanical activities are conducted to inactive distal regions [16]. The α-adrenoceptor pathway was first described in the human ureter in the 1970s [17]. Activation of α1-adrenoceptors leads to ureteral contraction via activation of phospholipase C, which in turn leads to the formation of second messengers (inositol triphosphanate [IP3] and diacylglycerol [DAG]). IP3 is involved in the mobilization of calcium from the sarcoplasmic reticulum, whereas DAG increases calcium influx across the cell membrane via the activation of protein kinase C [18]. Thus, the histologic characteristics of the three smooth muscle layers in the lower ureter and the more dense innervation of the lower ureter than the upper and mid ureter have become subjects of research interest.
The stimulation of the α1-receptors in the incomplete or complete ureteral obstruction by ureteral calculi increases the force of ureteral contraction and the frequency of ureteral peristalsis. Thus, a blockade of α1-receptors inhibits basal tone, reduces peristaltic amplitude and frequency, and decreases intra-luminal pressure. α-blockers also induce an increase in the intra-ureteral pressure gradient around the stones that helps in stone expulsion [19]. Patients who elect for an attempt at MET, such as the use of an α-blocker, should have well-controlled pain, no clinical evidence of sepsis, and adequate renal functional reserve. The patients should be followed with periodic imaging studies to monitor stone position and to assess for hydronephrosis or severe adverse effects. If the outcome of this treatment is not satisfactory, active stone removal modalities like URS or SWL should be required [4]. Follow-up at 7, 14, 21, and 28 days with blood test, urine test, and radiologic test should be practiced for such serious conditions. It is very important that the patient be advised of the attendant risk including the associated side effects of treatment modalities like URS, SWL, and MET, and that MET should be performed.
Medical treatments using nonselective α-blockers for spontaneous stone expulsion have been reported. Agrawal et al. [20] reported that for stones ≤ 1 cm, 10 mg alfuzosin results in a 35% increase in the stone expulsion rate, decreased expulsion time, and good control of colic pain compared with a control group. Pedro et al. [5] reported good pain control and stone expulsion time compared with a control group by using alfuzosin but found no significant difference in the stone expulsion rate between the afluzosin and control groups (73.5% vs. 77.1%). In the latter study, it is possible that the high rate of stone expulsion in the control group was unrelated to the effect of alfuzosin but rather reflected the small size of the stones in both groups (4.08 mm and 3.83 mm). In our study, the alfuzosin group displayed a 27.9% increased stone expulsion rate compared with the control group (p=0.026).
The α-1d receptor has the highest density in the distal ureter [18]. Tamsulosin, which is a selective α-1a and α-1d blocker, is a commonly used α-blocker for the medical treatment of ureteric stones. Al-Ansari et al. [21] reported that 0.4 mg tamsulosin produced a 26% increased stone expulsion rate and decreased stone expulsion time. Resim et al. [7] reported that the same dose of tamsulosin produced an insignificantly increased rate of stone expulsion (13.3%) and decreased colic episodes and pain. Hermanns et al. [13] reported no significant difference in the expulsion rate between the group using 0.4 mg tamsulosin and the control group (86.7% vs. 88.9%, respectively). However, these results involved small-sized stones (mean, 3.8 mm) in both groups, similar to the study of Pedro et al. [5].
In Korea and Japan, 0.2 mg tamsulosin is taken orally twice daily to achieve the affects attributed to 0.4 mg tamsulosin. This regimen is expensive and onerous and adverse effects such as retrograde ejaculation and fatigue can be increased. In our country, 0.2 mg tamsulosin is used for control of symptoms of benign prostatic hyperplasia; because the α-1d receptor is more dense in the lower ureter, we used the same dose of tamsulosin for MET. Yoon et al. [22] reported that the use of 0.2 mg tamsulosin produced a 25.7% increased stone expulsion rate and decreased expulsion time for 3 days for stones <10 mm in diameter. In two other studies, 0.2 mg tamsulosin resulted in increased stone migration and an increased stone expulsion rate [23,24]. However, studies that have compared tamsulosin 0.2 mg and 0.4 mg are not much more prevalent than those that have compared a nonselective α-blocker and tamsulosin. In particular, to our knowledge, the present study is the first direct comparison of 10 mg alfuzosin, 0.2 mg tamsulosin, and 0.4 mg tamsulosin in the management of lower ureteral calculi.
Comparison between the two tamsulosin doses and the 10-mg alfuzosin dose revealed no significant differences in expulsion rate or expulsion time. The expulsion time observed in this study was shorter than reported previously [25]. The higher expulsion rate observed with 0.2 mg tamsulosin compared with 0.4 mg tamsulosin was likely not a statistical error caused by the small numbers of subjects, but rather that the lower dose of tamsulosin was sufficient to lower ureteral peristalsis.
Similar to a previous study [26], all groups treated in this study with 0.2 mg tamsulosin, 0.4 mg tamsulosin, and 10 mg alfuzosin displayed no differences in postural hypotension. There were also no differences in dizziness, headache, and fatigue in these groups, which is also consistent with other studies [7,18,20]. Although tamsulosin has been linked to a higher incidence of retrograde ejaculation than the non-selective α-blocker alfuzosin [20], in our study, there was no significant difference in abnormal ejaculation between the groups. Whether the current result is real is debatable. The short-term nature of this study and the less frequent sexual behavior of urinary stone patients may have confounded the findings.
When a single ureteral stone remains after 28 days of medical treatment, URS, SWL, and a second cycle of MET can be used for stone removal. A second cycle of tamsulosin therapy in nonresponders to a first cycle of MET may not significantly improve the expulsion rate [27]. Hubner et al. [28] reported that a maximum observation period of 30 days was chosen because a longer period could increase the complication rate by 20%. Thus, we advocate the need for aggressive stone removal such as URS or SWL when the first cycle of MET has failed.
The use of tamsulosin doses of 0.2 mg and 0.4 mg and of 10 mg alfuzosin for MET of single lower ureteral stones of 4 to 10 mm in diameter proved to be safe and effective as demonstrated by the increased stone expulsion rate, decreased expulsion time, and no significantly different adverse effects. We confirm that a first cycle of MET with 0.2 mg tamsulosin is safe and effective and can be considered as an option in the management of a single lower ureteral stone.
Figures and Tables
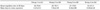
TABLE 3
Adverse effects observed in patients

Values are presented as number (%).
Group 1, tamsulosin 0.2 mg once; Group 2, tamsulosin 0.2 mg twice; Group 3, alfuzosin 10 mg; Group 4, control group.
Statistical significance was analyzed by the Pearson's chi-square and Fischer's exact test. There were no statistically significant differences in any groups.
References
1. Jo MK, Kwak C, Park SK, Yoo KY, Kang DH, Kim HH, et al. Prevalence and epidemiological characteristics of urolithiasis for adults aged 40-79 in Seoul, Korea. Korean J Urol. 2000. 41:367–374.
2. Parmar MS. Kidney stones. BMJ. 2004. 328:1420–1424.
3. Tomson CR. Prevention of recurrent calcium stones: a rational approach. Br J Urol. 1995. 76:419–424.
4. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007. 178:2418–2434.
5. Pedro RN, Hinck B, Hendlin K, Feia K, Canales BK, Monga M. Alfuzosin stone expulsion therapy for distal ureteral calculi: a double-blind, placebo controlled study. J Urol. 2008. 179:2244–2247.
6. Resorlu B, Bozkurt OF, Senocak C, Unsal A. Effectiveness of doxazosin in the management of lower ureteral stones in male and female patients. Int Urol Nephrol. 2011. 43:645–649.
7. Resim S, Ekerbicer H, Ciftci A. Effect of tamsulosin on the number and intensity of ureteral colic in patients with lower ureteral calculus. Int J Urol. 2005. 12:615–620.
8. Narepalem N, Sundaram CP, Boridy IC, Yan Y, Heiken JP, Clayman RV. Comparison of helical computerized tomography and plain radiography for estimating urinary stone size. J Urol. 2002. 167:1235–1238.
9. Parsons JK, Lancini V, Shetye K, Regan F, Potter SR, Jarrett TW. Urinary stone size: comparison of abdominal plain radiography and noncontrast CT measurements. J Endourol. 2003. 17:725–728.
10. Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. The American Urological Association. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997. 158:1915–1921.
11. Giannarini G, Autorino R. Recommending medical expulsive therapy for distal ureteric calculi: a step back? Eur Urol. 2009. 56:413–415.
12. Miller OF, Kane CJ. Time to stone passage for observed ureteral calculi: a guide for patient education. J Urol. 1999. 162(3 Pt 1):688–690.
13. Hermanns T, Sauermann P, Rufibach K, Frauenfelder T, Sulser T, Strebel RT. Is there a role for tamsulosin in the treatment of distal ureteral stones of 7 mm or less? Results of a randomised, double-blind, placebo-controlled trial. Eur Urol. 2009. 56:407–412.
14. Sur R, Marguet C, Priminger G. Management of ureteral calculi. AUA Update. 2006. 25:161–171.
15. Flanigan RC. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Urothelial tumors of the upper urinary tract. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;1641–1642.
16. Lang RJ, Exintaris B, Teele ME, Harvey J, Klemm MF. Electrical basis of peristalsis in the mammalian upper urinary tract. Clin Exp Pharmacol Physiol. 1998. 25:310–321.
17. Malin JM Jr, Deane RF, Boyarsky S. Characterisation of adrenergic receptors in human ureter. Br J Urol. 1970. 42:171–174.
18. Sigala S, Dellabella M, Milanese G, Fornari S, Faccoli S, Palazzolo F, et al. Evidence for the presence of alpha1 adrenoceptor subtypes in the human ureter. Neurourol Urodyn. 2005. 24:142–148.
19. Ahmed AA, Al-sayed AS. Tamsulosin versus alfuzosin in the treatment of patients with distal ureteral stones: prospective, randomized, comparative study. Korean J Urol. 2010. 51:193–197.
20. Agrawal M, Gupta M, Gupta A, Agrawal A, Sarkari A, Lavania P. Prospective randomized trial comparing efficacy of alfuzosin and tamsulosin in management of lower ureteral stones. Urology. 2009. 73:706–709.
21. Al-Ansari A, Al-Naimi A, Alobaidy A, Assadiq K, Azmi MD, Shokeir AA. Efficacy of tamsulosin in the management of lower ureteral stones: a randomized double-blind placebo-controlled study of 100 patients. Urology. 2010. 75:4–7.
22. Yoon WY, Jeong TY, Lee SI, Kim DJ. Effect of tamsulosin and dichlozid on the expected treatment of ureteral calculi. Korean J Urol. 2009. 50:1213–1218.
23. Kang DI, Cho WY, Kim TH, Chung JM, Park J, Yoon JH, et al. Effect of tamsulosin 0.2 mg on the short-term treatment of urinary stones: multicenter, prospective, randomized study. Korean J Urol. 2009. 50:586–590.
24. Kaneko T, Matsushima H, Morimoto H, Tsuzaka Y, Homma Y. Efficacy of low dose tamsulosin in medical expulsive therapy for ureteral stones in Japanese male patients: a randomized controlled study. Int J Urol. 2010. 17:462–465.
25. Lojanapiwat B, Kochakarn W, Suparatchatpan N, Lertwuttichaikul K. Effectiveness of low-dose and standard-dose tamsulosin in the treatment of distal ureteric stones: a randomized controlled study. J Int Med Res. 2008. 36:529–536.
26. Mondaini N, Giubilei G, Ungar A, Gontero P, Cai T, Gavazzi A, et al. Alfuzosin (10 mg) does not affect blood pressure in young healthy men. Eur Urol. 2006. 50:1292–1296.
27. Porpiglia F, Vassino D, Volpe A, Renard J, Cracco C, Ragni F, et al. Is there a role for a second cycle of medical expulsive therapy with tamsulosin in patients with distal ureteral stones? Eur Urol Suppl. 2007. 6:116.
28. Hubner WA, Irby P, Stoller ML. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993. 24:172–176.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download