Abstract
Purpose
The transobturator adjustable tape (TOA) sling operation is an effective procedure that allows for correction of postoperative incontinence or obstruction through adjustment of the mesh tension. During the operation, the outer cylinder of a ballpoint pen was used for proper mesh placement with less dissection. We evaluated the efficacy and safety of the TOA sling operation with the use of the outer cylinder of a ballpoint pen.
Materials and Methods
A total of 127 consecutive women with stress urinary incontinence underwent the TOA sling operation with the use of the outer cylinder of a ballpoint pen. The preoperative evaluations included a stress cough test, urodynamic study, and questionnaires related to quality of life. The mesh tension was adjusted 1 day after the operation. Postoperative evaluation was done at 1 month and included a stress cough test, uroflowmetry, questionnaires, and asking about satisfaction. At 1 year, we evaluated the patients with a stress cough test and by asking about their satisfaction with the procedure.
Results
The overall cure rate was 95.3% at 1 month and 96.8% at the 1-year follow-up. Postoperative adjustment of the mesh tension was done for 22 patients (17.3%). Eight patients needed increased tension for remaining stress urinary incontinence, and 14 patients needed reduced tension for urinary obstruction. The maximal flow rate was decreased significantly. However, the residual urine volume was not increased significantly. The total score on the questionnaires increased significantly.
Stress urinary incontinence (SUI) is an involuntary leakage of urine with increased intraabdominal pressure caused by weakness of the pelvic floor musculature, including the bladder neck and proximal urethra, or intrinsic sphincter deficiency. SUI is the most common form of urinary incontinence in women, and about 21% of middle-aged Korean women suffer from SUI [1]. SUI adversely affects the quality of life (QoL) and well-being of approximately 15% of the female population [2]. The treatment options for SUI include retropubic suspensions and slings, transobturator tape procedures, injectable bulking agents, and artificial urinary sphincter placement [3]. Delorme [4] described an attempt to reduce the morbidity of retropubic needle passage, an alternative approach with a transobturator tape (TOT). Despite the high success rate of the midurethral sling procedure (average, 86.8 to 91%), a subset of patients remains refractory to this treatment [5,6]. Several risk factors for tape failure are recognized, of which commonly cited factors are obesity, internal sphincter deficiency, aging, previous anti-incontinence surgery, concurrent prolapse surgery, hypoestrogenism, preoperative anticholinergic use, neurological disorders, and comorbidities typical of elderly individuals, such as hypertension, diabetes, and dementia [7-9]. Recently, poor surgical technique and tape placement too close to the bladder neck were noted as risk factors for midurethral tape failure [10].
It is difficult to apply the correct degree of tension during the TOT procedure. When the tape is too loose, incontinence persists. On the other hand, when the tape is too tight, urinary obstruction occurs. However, tension adjustment is difficult with this method. Thus, the transobturator adjustable tape (TOA) sling operation is an effective procedure that allows for correction of postoperative incontinence or obstruction through adjustment of mesh tension. Additionally, for proper mesh placement with less dissection, we used the outer cylinder of a ballpoint pen during the TOA sling operation. Here we evaluate the efficacy and safety of the TOA sling operation with the use of the outer cylinder of a ballpoint pen.
The patients consisted of 127 consecutive women who underwent the implantation of the TOA sling (A.M.I TOA Sling, A.M.I GmbH, Feldkirch, Austria) at our institution.
All patients were given a routine preoperative workup, including history taking, physical examination, and stress cough test, a urodynamic study including uroflowmetry and post-void residual (PVR) urine measurement, and questionnaires related to quality of life (Korean-IQoL). The Korean-IQoL contains 22 items, each with a five-point Likert-type response scale, yielding a total score and three subscale scores. The symptom of SUI divided a grade by Stamey symptom grade. We checked pelvic organ prolapse by use of the pelvic organ prolapse quantification system.
The operation was done under general or spinal anesthesia by 1 experienced surgeon. The patient was placed in the dorsal lithotomy position with the legs in hyperflexion. After palpation of the obturator foramen, a puncture incision was made at the level of the clitoris. For precise mesh positioning, the anatomical urethral length was measured by using a Foley catheter. A small vertical vaginal incision was then created over the midurethra after hydrodissection using saline, and dissection was carried out laterally to the ischiopubic ramus. The outer cylinder of a ballpoint pen was introduced in the tunnel that was previously dissected. A curved tunneler then allowed perforation of the mesh through the obturator foramen. The tunneler was guided by the outer cylinder of the ballpoint pen at the anterior vaginal wall instead of the surgeon's finger (Figs. 1, 2). Inspection was carried out at this point to exclude inadvertent penetration of the vaginal fornix or associated urinary structures. The synthetic material was then attached to the tunneler and brought out through the inner thigh stab wound. The procedure was repeated on the contralateral side. Tension was set on the tape by passing a clamp between the tape and urethra such that a surgical clamp could be passed easily between these two structures. Excess material was then cut at the skin puncture site and the incisions were closed. The exposed string at the inguinal area was used to increase the tension when incontinence persisted. The exposed string at the vagina wall was used to decrease the tension when bladder outlet obstruction occurred. The uroflowmetry and provocation test (stair up-down and fast walking after bladder filling with 200 ml normal saline) were done 1 day after surgery. If incontinence remained, the mesh was tightened by pulling up the inguinal strings on each lateral side. If the maximum flow rate was less than 10 ml/s and residual urine was more than 50 ml, tension was released by pulling down on one cross-side of the vaginal strings.
Postoperative follow-up was performed at 1 week, 1 month, and 1 year after the operation. At 1 week, a physical examination was done for detection of early complications. At 1 month, the evaluation consisted of a stress cough test, uroflowmetry, residual urine volume measurement, and the questionnaires (Korean-IQoL). We asked the patients about their satisfaction with the procedure and any postoperative problems. At the 1-year follow-up, the evaluations consisted of a stress cough test and asking about patient satisfaction. Some patients allowed uroflowmetry, residual urine volume measurement, and the questionnaires (Korean-IQoL). The cure rate was made up of the two aspects of objective and subjective outcomes. Objective cure was defined as a negative result on the stress cough test and a nonobstructive voiding pattern. Subjective cure was defined as satisfaction and an increased total score on the Korean-IQoL. Statistical analysis of the data was performed by using paired t-tests. IBM SPSS ver. 18.0 (IBM Co., New york, NY, USA) was used for the data analysis. Statistical significance was set at p<0.05.
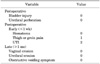
A total of 127 women underwent the TOA sling procedure with use of the outer cylinder of a ballpoint pen. The mean age of the population was 56.6 years, mean parity was 3.1, mean body mass index was 25.3 kg/m2, and urethral length was 2.8 cm. Forty-two women had urge urinary incontinence (33.1%) (Table 1). The mean operation time (skin incision to last suture time) was 11.3 minutes. Postoperative adjustment of the mesh tension was done for 22 patients (17.3%). Eight patients (6.3%) needed increased tension because of remaining SUI, and 14 patients (11.0%) needed reduced tension for urinary obstruction at 1 day after the operation. The objective and subjective results were evaluated at 1 month after surgery. The negative cough test rate was 99.2%. The obstructive voiding pattern (maximum flow rate <10 ml/s and residual volume >50 ml) was observed in 3.9% of patients. The satisfaction rate was 95.3% and the percentage of women with an increased Korean-IQoL score was 92.8% (Table 2). The satisfaction rate was 96.8% at the 1-year follow up (60 patients satisfied with operation out of 62 patients). Five patients complained of persistent urge incontinence with no SUI, but there was no de novo urgency or urge incontinence. The maximal flow rate was decreased significantly at the 1-month follow-up (p<0.001). However, the residual urine volume was not increased significantly (p=0.390). The total score of the questionnaires (IQoL) was increased significantly (p=0.027) (Table 3). No perioperative complications occurred. Postoperative complications occurred in three patients (2.4%) at the 1-week follow-up. Thigh pain occurred in 1 patient and was resolved spontaneously within 1 month. Urinary tract infection that was cured by antibiotics occurred in 2 patients (Table 4).
The sling operation is the most frequently used method in the surgical treatment of urinary incontinence. The tension-free vaginal tape (TVT) procedure presented by Ulmsten et al. [11] is a representative sling operation. However, there have been reports of complications of bladder perforation, major bleeding, and damage to the internal organs [12]. Delorme et al. [13] reported that the TOT procedure, which uses an obturator foramen to pass through the tape, is more convenient and efficient than the TVT procedure and has a low risk of bladder perforation and also has fewer complications. De Laval [14] further improved the TOT procedure. The inside-out TVT obturator (TVT-O) procedure passes the needle from the inside of the vagina through the thigh and into the tape. In 2006, the TVT-secur sling became available. Although there is no skin incision for pulling out the sling, the procedure is based on the usual midurethral polypropylene tape support, which it is accepted as an easy and safe technique [15].
The two most frequent problems after stress incontinence surgery are persistence of incontinence and voiding dysfunction, both of which are related to how loose or how tight the tape is implanted [16]. Too little tension can result in continued incontinence; too much tension can cause urinary obstruction. Based on the integral theory, which states that SUI results from defective urethral support, the tape consists of a piece of Prolene mesh that is loosely placed under the urethra to effectively recreate the pubourethral ligament [17,18]. However, despite its tension-free nature, studies have shown that the tape causes postoperative voiding dysfunction in 2.8 to 14% of patients [19]. The published surgical results of the TOT procedure indicate a high success rate of 86.8 to 91% [5,6]. The usual reason for midurethral sling failure is misplacement of the suburethral tape or inadequate tension on the tape [20]. To date, various surgical methods that allow adjustment of the tension, which in turn corrects urinary incontinence or retention, have been introduced. These include the REMEEX system, the adjustable transvaginal tape, and the TOA. In the TOA procedure, loosening of the mesh results in increased urine flow and decreased residual urine. Tightening of the mesh results in continence. Thus, TOA can improve results by allowing the correction of postoperative urinary incontinence or retention. We performed an evaluation at postoperative day 1 after removal of the Foley catheter. Evaluation for persistent urinary incontinence included the cough test, stair up-down test, and fast walking for 5 minutes after filling with 200 ml normal saline. If the test results indicated that incontinence was present, the tension was released from the mesh by pulling up the pubic strings on each lateral side approximately 1 cm. Evaluation for bladder outlet obstruction was conducted by uroflowmetry with residual urine volume measurement using ultrasound. If the maximum flow rate was less than 10 ml/s and residual urine volume was more than 50 ml, tension was released from the mesh by pulling down on one cross-side of the vaginal strings approximately 1 cm. We evaluated persistent urinary incontinence or urinary retention at 1 day after tension control. Most patients' symptoms were controlled with one adjustment of the mesh tension. Two patients underwent adjustment twice.
Lee et al. [21] noted that the overall long-term (6-year follow up) cure rate for urinary incontinence with the TVT procedure was 83.0% with a satisfaction rate of 80.1%, and the 1-year cure rate was 93.4%. Maroto et al. [22] noted in their results of the TOA procedure that 90% of the patients were objectively stress continent, 6.5% of the patients had considerable improvement, and 3.5% of the patients experienced failure during the mean follow-up period of 24.7 months. In another study, Youn et al. [23] noted that 95% of the patients were objectively stress continent and subjectively satisfied at postoperative 3 months. In our study, we did not exclude patients with urge incontinence. Nevertheless, the rate of objective cure (negative cough test) was high, as was the rate of subjective cure (satisfaction).
Many questionnaires for the assessment of QoL in urinary incontinence are being used internationally after proper linguistic validation; typical questionnaires include the I-QoL and the King's Health Questionnaire [24]. In our study, we used Korean-IQoL. A total of 69 women completed both preoperative and postoperative Korean-IQoL questionnaires. The total score on the Korean-IQoL increased significantly in 64 of 69 women.
Abdel-Fattah et al. [25] reported the results of comparing 'inside-out' versus 'outside-in' TOT in the management of urodynamic stress incontinence. They found no significant differences in patient-reported and objective cure rates between 'inside-out' and 'outside-in' TOT. The perioperative complication rates were not significantly different between the groups, except for a higher rate of vaginal angle perforation associated with the 'outside-in' Totaris, which was attributed mainly to the need for more dissection with this technique. A number of studies have suggested a high risk of postoperative groin pain with the 'inside-out' TVT-O treatment, with a range of 15 to 24% and with as many as 4.7% of patients complaining of long-term pain [26,27]. But and Faganelj [28] found the 'inside-out' TVT-O approach to be significantly more painful than the 'outside-in' Monarc approach during the operation and for up to 6 hours postoperatively [28].
We used the outer cylinder of a ballpoint pen instead of a finger for guidance of the curved tunneler. The diameter of the outer cylinder of the ballpoint pen was 1.1 cm, which was smaller than the diameter of the surgeon's finger (about 1.6 cm) (Fig. 1). We consider that the minimum length for vaginal wall incision was the length of the minimum triangle that surrounded each circle of the ballpoint pen and finger. Therefore, the incision length of the outer cylinder of the ballpoint pen needed to be 1.9 cm and the incision length of the surgeon's finger needed to be 2.77 cm by use of the formula of tan 30° (needed length=diameter/tan 30°). For proper placement of the midurethral sling, the minimal incision of the outer cylinder of the ballpoint pen suggested the accurate position of the mesh and prevented dislocation of the mesh, both of which are advantages. Also, the minimal dissection reduced injury to the vaginal wall, which reduced bleeding, inflammation, and wall perforation.
In our study, early postoperative complications occurred in only 3 cases at the 1-week follow-up and no late postoperative complications occurred.
A limitation of this study was the lack of a comparative group that underwent the traditional transobturator sling procedure. We compared our results with those for the traditional transobturator sling procedure indirectly by comparison with the studies of others.
The TOA allows adjustment of the tension applied during the intervention and permits postoperative correction of incontinence or obstruction. The subjective and objective results of the present study were excellent compared with outcomes of the traditional transobturator sling procedure. We conclude that proper mesh placement with less dissection and tension adjustment by use of the outer cylinder of a ballpoint pen can improve the success rate in patients undergoing the TOA sling operation for SUI.
Figures and Tables
FIG. 2
The curved tunneller perforated through obturator foramen guided by outer of the ball point pen.

TABLE 1
Clinical characteristics of patients treated with transobturator adjustable tape sling operation

References
1. Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010. 29:213–240.
2. Minassian VA, Stewart WF, Wood GC. Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol. 2008. 111(2 Pt 1):324–331.
3. Dmochowski RR, Blaivas JM, Gormley EA, Juma S, Karram MM, Lightner DJ, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010. 183:1906–1914.
4. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001. 11:1306–1313.
5. Lee KS, Han DH, Choi YS, Yum SH, Song SH, Doo CK, et al. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: 1-year followup. J Urol. 2007. 177:214–218.
6. Waltregny D, Reul O, Mathantu B, Gaspar Y, Bonnet P, de Leval J. Inside out transobturator vaginal tape for the treatment of female stress urinary incontinence: interim results of a prospective study after a 1-year minimum followup. J Urol. 2006. 175:2191–2195.
7. Glazener CM, Lapitan MC. Urodynamic investigations for management of urinary incontinence in adults. Cochrane Database Syst Rev. 2002. (3):CD003195.
8. Barber MD, Kleeman S, Karram MM, Paraiso MF, Ellerkmann M, Vasavada S, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol. 2008. 199:666.e1–666.e7.
9. Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002. 21:261–274.
10. Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Bartuzi A, et al. Tape fixation: an important surgical step to improve success rate of anti-incontinence surgery. J Urol. 2011. 186:180–184.
11. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:81–85.
12. Choi SK, Yun JM, Lee YS. Early clinical outcome and complications of tension free vaginal tape procedure in stress incontinent women. Korean J Urol. 2001. 42:589–593.
13. Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004. 45:203–207.
14. de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003. 44:724–730.
15. Tartaglia E, Delicato G, Baffigo G, Signore S, Corvese F, Perla A, et al. Third-generation tension-free tape for female stress urinary incontinence. J Urol. 2009. 182:612–615.
16. Nitti VW, Carlson KV, Blaivas JG, Dmochowski RR. Early results of pubovaginal sling lysis by midline sling incision. Urology. 2002. 59:47–51.
17. Lee YS, Lee HN, Lee KS. The evolution of surgical treatment for female stress urinary incontinence: era of mid-urethral slings. Korean J Urol. 2010. 51:223–232.
18. Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl. 1990. 153:7–31.
19. Moore C, Paraiso MF. Voiding dysfunction after the tension-free vaginal tape procedure. Curr Urol Rep. 2005. 6:356–359.
20. Lee SY, Lee YS, Lee HN, Choo MS, Lee JG, Kim HG, et al. Transobturator adjustable tape for severe stress urinary incontinence and stress urinary incontinence with voiding dysfunction. Int Urogynecol J. 2011. 22:341–346.
21. Lee JH, Cho MC, Oh SJ, Kim SW, Paick JS. Long-term outcome of the tension-free vaginal tape procedure in female urinary incontinence: a 6-year follow-up. Korean J Urol. 2010. 51:409–415.
22. Maroto JR, Gorraiz MO, Bueno JJ, Perez LG, Bru JJ, Chaparro LP. Transobturator adjustable tape (TOA) permits to correct postoperatively the tension applied in stress incontinence surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009. 20:797–805.
23. Youn CS, Shin JH, Na YG. Comparison of TOA and TOT for treating female stress urinary incontinence: short-term outcomes. Korean J Urol. 2010. 51:544–549.
24. Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997. 104:1374–1379.
25. Abdel-Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H, Young D, et al. Randomised prospective single-blinded study comparing 'inside-out' versus 'outside-in' transobturator tapes in the management of urodynamic stress incontinence: 1-year outcomes from the E-TOT study. BJOG. 2010. 117:870–878.
26. Collinet P, Ciofu C, Costa P, Cosson M, Deval B, Grise P, et al. The safety of the inside-out transobturator approach for transvaginal tape (TVT-O) treatment in stress urinary incontinence: French registry data on 984 women. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:711–715.
27. Lim J, Cornish A, Carey MP. Clinical and quality-of-life outcomes in women treated by the TVT-O procedure. BJOG. 2006. 113:1315–1320.
28. But I, Faganelj M. Complications and short-term results of two different transobturator techniques for surgical treatment of women with urinary incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:857–861.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download