Abstract
Purpose
Transobturator approaches to midurethral sling surgery are one of the most commonly performed operations for female stress urinary incontinence throughout the world. However, very few results of randomized clinical trials of transobturator midurethral sling surgery (MONARC vs. TVT-O) for the treatment of female urinary incontinence have been reported. In this study, we compared the 3-year follow-up cure rates of these two procedures.
Materials and Methods
From July 2006 to June 2008, 74 patients who had undergone MONARC (35 patients) or TVT-O (39 patients) were included in the study and were analyzed prospectively. The mean follow-up duration of both groups was 39.2 months. Preoperative and postoperative evaluations included physical examination, uroflowmetry and postvoid residual measurement, involuntary urine loss with physical activity, and urinary symptoms. Cure of female urinary incontinence was defined as patient report of no loss of urine upon physical activity. The patients' satisfaction after treatment was rated as very satisfied, satisfied, equivocal, and unsatisfied. Very satisfied and satisfied were considered as the satisfied rate.
Results
There were no significant differences in preoperative patient characteristics, postoperative complications, or success rate between the two groups. The cure rate of the MONARC and TVT-O groups was 85.7% and 84.6%, respectively. The patient satisfaction (very satisfied, satisfied) rate of the MONARC and TVT-O groups was 82.8% and 82.1%, respectively.
Stress urinary incontinence (SUI) is the most common type of urinary incontinence in females, in which the involuntary leakage of urinary flow occurs as abdominal pressure increases and the bladder neck opens, caused by hyperkinesia of the urethra and dysfunction of the urethral sphincter. In Korea, 37.8% of women suffer from SUI, and there is increasing interest in improved quality of life for patients, leading to aggressive treatment strategies [1].
Retropubic suburethral tension-free vaginal tape (TVT) has revolutionized the treatment of SUI [2,3]. The technique, which is effective, is nonetheless associated with a risk of complications [4]. Complications related to the retropubic access route, such as wound infection, urethral infection, hematoma, bladder perforation, gastrointestinal injury, and vascular or nerve injury, can occur, and in serious condition can be fatal [2,5]. In 2001, a surgical technique similar to TVT but that reduced the complication rate by replacing the retropubic route with the transobturator route was proposed. Delorme [6] was the first to describe the method of subobturator suburethral suspension known as outside-in. More recently, the transobturator route has been used, inside-out, with the technique reported by de Leval [7]. The most commonly used methods are the MONARC (outside-in, MONARC subfascial hammock, American Medical Systems Inc., Minnetonka, MN, USA) and the TVT-O (inside-out, TVT obturator system, Ethicon Inc., New Brunswick, NJ).
The author's experience with transobturator suburethral slings for the surgical correction of SUI, MONARC versus TVT-O, is reported herein with the aim of confirming the efficacy and safety of the two methods.
From July 2006 to June 2008, 74 female patients with SUI who underwent the transobturator route procedure at our hospital were included in this randomized, prospective, observational study. A total of 35 patients underwent the MONARC procedure and 39 patients underwent the TVT-O procedure.
Preoperatively, patients had a history of voiding symptoms such as frequency, urgency, and urge incontinence. Frequency was defined as needing to void more than 8 times a day; urgency was defined as having a sudden, compelling urge to urinate; and urge incontinence was defined as a leakage of urine due to bladder muscles that contract inappropriately, also showing symptoms of urgency.
All patients also underwent history taking, pelvic examination, urinalysis, culture test, uroflowmetry, postvoid residual, Q-tip test, stress test, and urodynamic study including Valsalva leak point pressure (VLPP). Through the preoperative physical examination and urodynamic studies, patients with neurogenic bladder, pelvic organ prolapse, suspected intrinsic sphincter deficiency, or a past history of radical pelvic surgery were excluded.
The procedure was performed by a single surgeon, and patients underwent one of the two techniques in accordance with the scheduling order (MONARC and TVT-O, in alternation). Cystoscopy was performed to ensure that there was no injury to the bladder during the procedure. After checking for any bladder injury, we inserted a Foley catheter. On postoperative day 1, we removed the catheter and residual volume was measured after spontaneous voiding. Following the postoperative period, urinary incontinence status and patient satisfaction were examined through an interview and physical examination in an outpatient setting. Patients were considered to be cured if they had no symptoms of urinary incontinence after the procedure, were considered to be improved if urinary incontinence was improved after the procedure and no more treatment was necessary, and were considered to be unchanged if the patient reported maintenance of urinary incontinence and was unsatisfied with the result of surgery. The term success rate indicated the sum of the cure and improvement rates. Cure was defined as the absence of any episodes of involuntary urine leakage during stressful activities and a stress test. Improvement was defined as a significant reduction in urine leakage, such that it did not require further treatment. The satisfaction score was classified into "very satisfied," "satisfied," "equivocal," and "unsatisfied" on the basis of the patient's subjective symptoms; very satisfied and satisfied were combined as the satisfied rate. We also checked on postoperative frequency, urgency, urge incontinence, or any other new voiding symptoms such as urge urination. Uroflowmetry and postvoid residual (PVR) were also measured.
Statistical analysis of the data was performed by using Student's t-test and chi-square test, for which SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used. A p-value of <0.05 was considered statistically significant.
The MONARC and TVT-O patient groups had a mean age of 55.1±10.63 years (range, 35 to 79 years) and 54.4±10.13 years (range, 31 to 79 years), respectively. The mean follow-up period was 39.2±3.1 months (range, 32 to 44 months) in the MONARC group and 39.2±2.4 months (range, 34 to 45 months) in the TVT-O group. The characteristics of the patients are summarized in Table 1. There were no significant differences between the two groups.
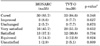
At 3 years of follow-up, the surgical cure rates were 85.7% (30/35) in the MONARC group and 84.6% (33/39) in the TVT-O group. Although the cure rate was slightly higher in the MONARC group, the difference between the groups was not statistically significant. In the MONARC group, five patients showed incontinence postoperatively. Three of them showed improvement and two were unchanged. Six patients in the TVT-O group showed incontinence postoperatively. Three of them showed improvement and three were unchanged. Following the MONARC and TVT-O procedures, the rates of satisfaction were 82.8% (29/35) and 82.1% (32/39), respectively. Patient's satisfaction did not differ significantly between the groups (Table 2). The surgical cure rate decreased year after year (Table 3).
In terms of uroflowmetry and PVR, the mean postoperative maximal flow rate (MFR, ml/s) in the MONARC and TVT-O groups was 22.9±10.2 ml/s and 22.1±10.6 ml/s, respectively. The mean postoperative PVR in the MONARC and TVT-O groups was 23.5±44.1 ml and 23.9±54.2 ml. There were no statistically significant observable differences between the two groups in postoperative residual urine. Also, there were no significant complications related to MONARC or TVT-O. Two cases of voiding difficulty, a case of vaginal discharge, and a case of dyspareunia were observed in the MONARC group. In the TVT-O group, there were three cases of voiding difficulty, one of dyspareunia, and one of pain in the thighs. No bladder perforation or urethral injury was reported in either group. There were no statistically significant between-group differences for any complications (Table 4).
A variety of modalities have been implemented for the management of female SUI, such as conservative treatment, drug treatment, and surgical treatment, and it is known that surgical treatment is the most effective [8]. Following the initial reports by Ulmsten et al. [2] on a new surgical procedure to treat SUI, the TVT procedure gained worldwide diffusion due both to its mini-invasiveness and to its high success rates. Through assessment by use of strict objective and subjective outcome measures, cure rates of 85% have been reported, with another 5 to 10% showing significant improvement [9], and preliminary analysis of the 7-year results of Nilsson et al. [10] indicates a cure rate of 81%.
However, because the TVT trocar is directed from the vagina to the retropubic area in an essentially blind manner, it can cause bladder injuries and rare but life-threatening injuries to the bowels or large vessels [11,12]. Because most of these complications seem to be related to the penetration of the retropubic space, a new surgical procedure that retains the same mid-urethra position as that of TVT while maintaining or even improving efficacy by reducing or eliminating the complications related to the penetration of the retropubic space has been invented.
The transobturator type technique is simpler, easy to learn, and has shorter operative and hospitalization times. Also, the long-term record of this technique is positive enough that it is the most widely used procedure. Delorme [6] and Delorme et al. [13] reported in two articles that MONARC is a safe and effective surgical procedure for the treatment of female SUI, with a 90.6% cure rate and a 9.4% improvement rate at 1 year of follow-up. Jeong et al. [14] reported that the surgical cure rate was 84.8% (28/33) and the rate of patient satisfaction was 78.8% in the MONARC group. A study by Costa et al. [15] confirmed the hypothesis that MONARC may dramatically reduce intraoperative complications by avoiding the retropubic space, indicating an overall complication rate of 2.2% (bladder perforation, urethral perforations, and number of vaginal lateral perforations). This rate is far lower than that reported with TVT, which can be up to 15% [16]. However, complications such as urethral or bladder perforation, vascular damage, and vaginal erosion are still reported.
Waltregny et al. [17] reported a prospective study of TVT-O implantation in 53 patients. The recovery rate was 94.3% at the 6-month time point. Only one case was considered a failure. The only complications consisted of transient pain for a few patients. Two patients underwent tape section due to chronic retention and imperious urges to urinate. Rader et al. [18] reported 106 cases of TVT-O implantationx. The objective recovery rate was 91.5% with 4.7% improvements and 3.8% failures. De novo imperious urges to urinate were observed in 3.8% of cases. One patient required tape repositioning due to complete retention.
Voiding difficulties with retention problems and de novo urge symptoms are the other complications that are most frequently associated with anti-incontinence operations. Whereas the traditional incontinence operation had an incidence rate of more than 30% [9], TVT has shown postoperative voiding difficulties of transient urine retention in 8 to 17% of patients [19-21] and urgency in 5 to 15% of patients [5,20,21]. Delorme [6] reported no postoperative voiding difficulties in his research on the use of the transobturator approach. In this study, one patient (2.9%) in the MONARC group experienced transient voiding difficulty. It has been hypothesized that, with the retropubic approach, the U-shaped sling kinks the urethra, whereas with the obturator approach, the sling is positioned more horizontally, thus reestablishing more natural lateral support and thereby decreasing the risk of postoperative voiding difficulties [11].
Liapis et al. [22] have reported that after 1 year of follow-up the rate of complete recovery of the MONARC and TVT-O procedures is 90% and 87% each. Lee et al. [23] reported that after 1 year of follow-up on 100 Korean SUI patients the rate of complete recovery was 92% and 86% each. On the other hand, Debodinance [24] reported that after follow-up on 100 patients who underwent MONARC or TVT-O, the rate of complete recovery was 90% and 94% each, which means that the rate of complete recovery was a bit higher with the TVT-O procedure. In this study, at 1 year of follow-up, the complete recovery rate of patients in MONARC group was 91.4% and that of the TVT-O group was 89.7%. At 3 years of follow-up, the complete recovery of the MONARC and TVT-O groups was 85.7% and 84.6% each, the improvement rate was 94.3% and 92.3% each, and there were no significant differences between the MONARC and TVT-O groups.
The outside-in technique necessitates more marked periurethral dissection because a finger must be used to locate the tip of the ancillary in contact with the ischiopubic branch. The method does not prevent vesical complications even though they are less numerous than with the retropubic technique. The technique may be accompanied by urethral lesions, which, while rare, are known to be more difficult to manage than is a vesical lesion [15,25]. In the results of a multicenter study, Costa et al. [15] also reported that out of 183 patients who underwent surgery based on the outside-in method, 1 and 2 showed perforation of the urinary bladder and damage to the urethra, respectively. In contrast, the inside-out technique does not require extensive dissection and apart from the risk of delivering a direct wound to the bladder or urethra during scissor dissection, it is not possible to secondarily wound the bladder or urethra with the ancillary thanks to the metal guide system. It is generally known that after TVT-O patients do not need cystoscopy because the technique does not pass through the Retzius space and therefore is less likely to cause bladder perforation. However, when the tip of an apparatus is inserted obliquely and in the wrong direction, it could cause bladder perforation. We carried out cystoscopy for every surgery and found no additional complications.
Although the inside-out method is known to have a lower risk of nerve or blood vessel damage, the procedure must be conducted carefully because the distance between the obturator canal, which has many obturator vessels and obturator nerves to pass by, and the tunnel instrument is short (TVT-O, 19 mm vs. MONARC, 27 mm) [26,27]. In a study conducted on seven cadavers, Spinosa et al. [28] showed a dangerous proximity between the trajectory of TVT-O and the pudendal vascular pedicle, whereas there was a safety margin of over 3 cm with the transobturator type outside-in technique. Hemorrhagic complications can occur intraoperatively during needle insertion. There was about a 2 to 4% rate in five studies of TVT [29]. The transobturator suburethral approach has been introduced to minimize the risk of complications arising from the retropubic passage of the needle. No significant bleeding or hematoma complication has been reported [30].
In this study, there were no intraoperative complications and no urethral, bladder, bowel, or vascular injuries. The complications reported consisted of recalcitrant pain and adductor muscle deficiency creating a risk of disorders of gait and standing and preventing crossing of the legs. One case of pain causing transient discomfort was observed in this study.
Figures and Tables
TABLE 2
Postoperative comparisons of cure rate and satisfaction rate between patients who underwent MONARC and TVT-O
References
1. Choo MS, Ku JH, Oh SJ, Lee KS, Paick JS, Seo JT, et al. Prevalence of urinary incontinence in Korean women:an epidemiologic survey. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:1309–1315.
2. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:81–85.
3. Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001. 12:Suppl 2. S5–S8.
4. Debodinance P, Delporte P, Engrand JB, Boulogne M. Tension-free vaginal tape (TVT) in the treatment of urinary stress incontinence: 3 years experience involving 256 operations. Eur J Obstet Gynecol Reprod Biol. 2002. 105:49–58.
5. Boustead GB. The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2002. 89:687–693.
6. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001. 11:1306–1313.
7. de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003. 44:724–730.
8. Kim TH, Kwon JK, Lee SY, Kim TH. The comparision of the short term result of transobturator and retropubic mid urethral slings in the female stress urinary incontinence. J Korean Continence Soc. 2007. 11:131–136.
9. Nilsson CG. Latest advances in TVT tension-free support for urinary incontinence. Surg Technol Int. 2004. 12:171–176.
10. Nilsson CG, Falconer C, Rezapour M. Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004. 104:1259–1262.
11. Ansquer Y, Marcollet A, Yazbeck C, Salomon L, Poncelet C, Thoury A, et al. The suburethral sling for female stress urinary incontinence: a retropubic or obturator approach? J Am Assoc Gynecol Laparosc. 2004. 11:353–358.
12. Kuuva N, Nilsson CG. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand. 2002. 81:72–77.
13. Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004. 45:203–207.
14. Jeong MY, Kim SJ, Kim HS, Koh JS, Kim JC. Comparison of efficacy and satisfaction between the TVT-SECUR® and MONARC® procedures for the treatment of female stress urinary incontinence. Korean J Urol. 2010. 51:767–771.
15. Costa P, Grise P, Droupy S, Monneins F, Assenmacher C, Ballanger P, et al. Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T.O.T.) Uratape: short term results of a prospective multicentric study. Eur Urol. 2004. 46:102–106.
16. Lebret T, Lugagne PM, Hervé JM, Barré P, Orsoni JL, Yonneau L, et al. Evaluation of tension-free vaginal tape procedure. Its safety and efficacy in the treatment of female stress urinary incontinence during the learning phase. Eur Urol. 2001. 40:543–547.
17. Waltregny D, Reul O, Bonnet P, de Leval J. Inside-out transobturator vaginal tape (TVT-O): short-term results of a prospective study. Neurourol Urodyn. 2004. 23:428–429.
18. Rader JL, Lucente VR, Murphy M. Transobturator TVT (TVT-O) "Inside out" suburethral sling for the treatment of stress urinary incontinence (SUI): early clinical experience. Int Urogynecol J Pelvic Floor Dysfunct. 2005. 16:Suppl 2. S102.
19. Ulmsten U. The basic understanding and clinical results of tension-free vaginal tape for stress urinary incontinence. Urologe A. 2001. 40:269–273.
20. Soulié M, Cuvillier X, Benaïssa A, Mouly P, Larroque JM, Bernstein J, et al. The tension-free transvaginal tape procedure in the treatment of female urinary stress incontinence: a French prospective multicentre study. Eur Urol. 2001. 39:709–714.
21. Arunkalaivanan AS, Barrington JW. Randomized trial of porcine dermal sling (Pelvicol implant) vs. tension-free vaginal tape (TVT) in the surgical treatment of stress incontinence: a questionnaire-based study. Int Urogynecol J Pelvic Floor Dysfunct. 2003. 14:17–23.
22. Liapis A, Bakas P, Creatsas G. Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:185–190.
23. Lee KS, Choo MS, Lee YS, Han JY, Kim JY, Jung BJ, et al. Prospective comparison of the 'inside-out' and 'outside-in' transobturator-tape procedures for the treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:577–582.
24. Debodinance P. Trans-obturator urethral sling for the surgical correction of female stress urinary incontinence: outside-in (Monarc) versus inside-out (TVT-O). Are the two ways reassuring? Eur J Obstet Gynecol Reprod Biol. 2007. 133:232–238.
25. Krauth JS, Rasoamiaramanana H, Barletta H, Barrier PY, Grisard-Anaf M, Lienhart J, et al. Sub-urethral tape treatment of female urinary incontinence--morbidity assessment of the trans-obturator route and a new tape (I-STOP): a multi-centre experiment involving 604 cases. Eur Urol. 2005. 47:102–106.
26. Kim YJ, Huh JS, Song HJ. Clinical outcome of tension-free transobturator suburethral tape (inside-out TVT-O) procedure for the treatment of stress urinary incontinence: the two years follow-up. J Korean Continence Soc. 2007. 11:145–150.
27. Achtari C, McKenzie BJ, Hiscock R, Rosamilia A, Schierlitz L, Briggs CA, et al. Anatomical study of the obturator foramen and dorsal nerve of the clitoris and their relationship to minimally invasive slings. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:330–334.
28. Spinosa JP, Dubuis PY, Riederer B. Chirurgie de l'incontinence urinaire à l'effort féminine par voie transobturatrice: dehors dedans ou dedans dehors? Etude anatomique comparative. Prog Urol. 2005. 15:1–7.
29. Richards SR, Balaloski SP. Vulvar hematoma following a transobturator sling (TVT-O). Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:672–673.
30. Wang AC, Lin YH, Tseng LH, Chih SY, Lee CJ. Prospective randomized comparison of transobturator suburethral sling (Monarc) vs suprapubic arc (Sparc) sling procedures for female urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:439–443.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download