Abstract
Purpose
Historically, it was thought that hemorrhagic complications were increased with transrectal ultrasound-guided prostate biopsies (TRUS biopsy) of patients receiving anticoagulation/antiplatelet therapy. However, the current literature supports the continuation of anticoagulation/antiplatelet therapy without additional morbidity. We assessed our experience regarding the continuation of anticoagulation/antiplatelet therapy during TRUS biopsy.
Materials and Methods
A total of 91 and 98 patients were included in the anticoagulation/antiplatelet (group I) and control (group II) groups, respectively. Group I subgroups consisted of patients on monotherapy or dual therapy of aspirin, warfarin, clopidogrel, or low molecular weight heparin. The TRUS biopsy technique was standardized to 12 cores from the peripheral zones. Patients completed a questionnaire over the 7 days following TRUS biopsy. The questionnaire was designed to assess the presence of hematuria, rectal bleeding, and hematospermia. Development of rectal pain, fever, and emergency hospital admissions following TRUS biopsy were also recorded.
Results
The patients' mean age was 65 years (range, 52 to 74 years) and 63.5 years (range, 54 to 74 years) in groups I and II, respectively. The overall incidence of hematuria was 46% in group I compared with 63% in group II (p=0.018). The incidence of hematospermia was 6% and 10% in groups I and II, respectively. The incidence of rectal bleeding was similar in group I (40%) and group II (39%). Statistical analysis was conducted by using Fisher exact test.
Transrectal ultrasound-guided prostate biopsy (TRUS biopsy) is performed to obtain systematic biopsies for histological examination in patients with suspected prostate carcinoma. However, subjecting men to TRUS biopsy can cause significant morbidity. The procedure may be complicated by sepsis in 0.5% of patients and by hemorrhagic complications, which are much more common (hematuria, 39 to 44%; rectal bleeding, 17 to 27%; and hematospermia, 12 to 16%). These complications tend to be minor and self-limiting [1,2].
There have been historical concerns regarding performing TRUS biopsy for patients on anticoagulation or antiplatelet therapy owing to bleeding complications [3,4]. The current practice with regard to the discontinuation of anticoagulation or antiplatelet therapy prior to TRUS biopsy varies widely among clinicians, with 52% of radiologists and 27% of urologists terminating antiplatelet (aspirin) therapy before TRUS biopsy and 95% of radiologists and 84% of urologists stopping anticoagulation (warfarin) before TRUS biopsy [5]. However, the literature regarding bleeding complications following TRUS biopsy is limited.
The aim of this prospective study was to assess our experience regarding the continuation of anticoagulation/antiplatelet therapy during TRUS biopsy and to compare this prospectively with patients not on anticoagulation/antiplatelet therapy. We sought to assess the previous findings of the safety of aspirin and warfarin in patients undergoing TRUS biopsy and to document for the first time the effects of clopidogrel in these patients.
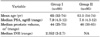
Data were collected on patients who were referred for TRUS biopsy on the basis of elevated prostate-specific antigen (PSA), an abnormal digital rectal examination, or clinical suspicion. Patients were divided into 2 groups, and a total of 88 patients on anticoagulation/antiplatelet therapy (group I) were included. The subgrouping of group I consisted of patients on monotherapy of aspirin, warfarin, clopidogrel, or low molecular weight heparin (LMWH) and patients on dual therapy of aspirin and warfarin or clopidogrel (Table 1). The dosage of aspirin and clopidogrel was 75 mg daily. The medical indications for patients on anticoagulation/antiplatelet therapy are listed in Table 1.
The control group (group II) of 95 patients who were not on anticoagulation or antiplatelet therapy was included for comparative analysis. The demographics of both groups, including PSA, prostate volumes, and international normalized ratio (INR), are listed in Table 2. A prospective comparative analysis was performed between the groups.
In group I, patients were advised not to discontinue their anticoagulation/antiplatelet therapy prior to TRUS biopsy. All participants received a detailed information leaflet explaining the procedure before undergoing the biopsy. The TRUS biopsy technique was standardized to 12 cores with an 18-gauge needle from the peripheral zones. A single dosage of 400 mg oral ofloxacin and 80 mg intravenous gentamicin was given before the procedure. The prostate was infiltrated with 10 ml of 1% lidocaine as a local anesthetic at the base of each lateral lobe with a 16-gauge spinal needle before TRUS biopsy as per the protocol [6]. A total of 200 mg of oral ofloxacin was also prophylactically prescribed to all patients for the evening of TRUS biopsy and the following morning.
All patients undergoing the TRUS biopsy completed a questionnaire over the 7 days following the biopsy (Fig. 1). This questionnaire examined the presence of hematuria, rectal bleeding, and hematospermia. Associated symptoms such as rectal pain and fever were also included. Patients were also asked to comment on whether they needed analgesia or general practitioner or hospital visits. Also included was information regarding the type of anticoagulants or antiplatelets used, known bleeding disorder, INR levels, and prostate volumes. A space for additional comments by the patient was provided, and relevant comments were taken into consideration. Upon return of the questionnaire, all information was entered into an electronic database and subsequently analyzed.
Responses from group I (88 patients) and group II (95 patients) were analyzed. The mean patient age was 65 years (range, 52 to 74 years) and 63.5 years (range, 54 to 74 years) in groups I and II, respectively. The overall incidence of hematuria was 40/88 patients (46%) in group I compared with 60/95 patients (63%) in group II (p=0.018). Additionally, the incidence of hematospermia was 5/88 patients (6%) and 9/95 patients (10%) in groups I and II, respectively (Table 3).
In contrast, the incidence of rectal bleeding was similar in group I (35/88 patients, or 40%) and group II (37/95 patients, or 39%) (Table 3).
The occurrence of rectal pain and the development of fever after TRUS biopsy were also examined in this study. In group I, 5/88 patients (6%) developed rectal pain following the procedure compared with 8/95 patients (8%) in group II. Similar findings were observed in relation to the development of fever after TRUS biopsy (5/88, or 6%, and 8/95, or 8%, in groups I and II, respectively) (Table 3).
Only 3 of 5 patients in group I who developed fever after TRUS biopsy visited their general practitioner and were subsequently prescribed antibiotics as appropriate in comparison with 4 of 8 patients in group II. The symptoms of rectal pain and fever in the remaining patients were self-limiting and did not require hospitalization. No patients in either group developed overwhelming urosepsis.
In group I, 2 of 88 patients (2.3%) required acute hospital admission with clot retention secondary to frank hematuria following TRUS biopsy. In group II, 1 of 95 patients (1%) sought medical attention with clot retention secondary to frank hematuria after TRUS biopsy.
In group I, one patient was on dual therapy of aspirin and clopidogrel for drug-eluting coronary stents, whereas the second patient was on warfarin alone (INR, 2.5) for atrial fibrillation. These patients were assessed, catheterized, and admitted to the hospital. The hemoglobin level of these patients was 9.4 g/dl (dropped from 11 g/dl at baseline) and 10 g/dl (dropped from 12 g/dl at baseline) in the first and second patients, respectively. Computerized tomography with intravenous contrast showed normal findings of the upper urinary tracts in both patients. Both patients were discharged well. One patient in group II, however, presented with clot retention following TRUS biopsy with hemoglobin of 10.2 g/dl and was managed in a similar fashion at both the emergency and ward levels. In both patients, the hematuria resolved after catheterization and no additional treatment or blood transfusion was required. This patient was also given prophylactic antibiotics (oral dosage of 400 mg twice daily of ciprofloxacin).
TRUS biopsy is the procedure of choice for diagnosing prostate cancer and is performed as an outpatient procedure. In some centers, it is common to discontinue antiplatelet and anticoagulant medications. Patients may need to be started on bridging therapy such as intravenous heparin infusion before TRUS biopsy to minimize cardiovascular or cerebral thrombotic complications [7].
There is evidence in the literature that there is a risk of increased cardiovascular or cerebral events associated with stopping antiplatelet agents. Current guidelines recommend that all patients suffering from coronary artery disease should receive daily aspirin therapy to reduce the risk of thromboembolic events such as stroke, myocardial infarction, and death, which is reduced by approximately 25% in patients with underlying cardiovascular disease [8]. It is also estimated that the discontinuation of antiplatelet therapy may precede up to 10.2% of acute cardiovascular syndromes. The time interval between discontinuation and acute cerebral events was 14.3±11.3 days, 8.5±3.6 days for acute coronary syndromes, and 25.8±18.1 days for acute peripheral arterial syndromes [3].
Moreover, in patients undergoing coronary stent insertion, the addition of clopidogrel to daily aspirin therapy is advocated for at least 1 month in the case of bare metal stents, 3 to 6 months for drug-eluting stents, and ideally for up to 1 year [9]. This combination has been shown to significantly reduce the incidence of ischemic cardiovascular events in patients with coronary stents [10,11].
Although antiplatelet therapy is commonly used for the primary prevention of atherothrombotic disease, it increases the risk of major gastrointestinal and intracranial bleeding by approximately 1.7- to 2.1-fold [12]. However, the absolute increase in risk of major bleeding is small, requiring 769 patients to be treated for 1 year to induce one additional major bleeding event [12]. Conversely, adding clopidogrel on top of daily aspirin therapy further increases the risk of bleeding, although combined aspirin and clopidogrel therapy has not been associated with increased risk of fatal or intracranial hemorrhage [12]. In surgical settings, it is believed that excessive bleeding induced by antiplatelet agents may result in surgical morbidity or mortality. In recent studies, the bleeding and transfusion rate following coronary artery bypass grafting was increased by 50% when combined clopidogrel and aspirin therapy was continued [13,14]. The practice of withholding antiplatelet agents 7 to 10 days before surgery to prevent excessive bleeding is widespread [15,16]. It is also known that many urology patients will be on long-term, low-dose aspirin, which is perhaps self-prescribed or prescribed by their general practitioner, usually as a prophylactic treatment for cardiovascular disease.
In a prospective study by Cahill et al. [17], 51 healthy volunteers were randomly assigned into 3 groups, each receiving a daily dosage of aspirin 75 mg, aspirin 300 mg, or placebo for 14 days. The specific platelet function test (PFA-100) was used to monitor platelet function before and after therapy. This study demonstrated that the duration of increased bleeding tendency after discontinuation of aspirin persisted up to 5 days. The study concluded that aspirin therapy should be discontinued 5 days before elective surgery. This should allow clinicians and surgeons to minimize the risks of stopping aspirin without increasing the risk of excessive perioperative bleeding [17].
Go et al. [18] reported a 50% reduction in the risk of ischemic stroke and peripheral embolism in known paroxysmal atrial fibrillation when patients were receiving warfarin. The authors stated, "Anticoagulation was associated with nearly a doubling in the relative rate of intracranial haemorrhage, but the additional absolute risk of intracranial haemorrhage on anticoagulation was low." Go et al. [18] also observed no significant increase in the rate of non-intracranial major hemorrhage on warfarin [18].
A recent survey from the United Kingdom demonstrated a significant variation in practice with regards to pre- and postoperative management of clopidogrel in patients undergoing urological procedures. The majority of urologists stopped clopidogrel agents before TRUS biopsy (90.6%). Furthermore, 43% of urologists did not routinely prescribe bridging therapy after discontinuing clopidogrel, and 92.8% of urologists felt evidence-based guidelines on clopidogrel use during the perioperative period would be useful [19].
Additionally, there appears to be significant variation in practice among orthopedic departments in the United Kingdom, with only 43.6% having a policy of discontinuing clopidogrel in patients before surgery for femoral neck fractures. This compares with 37.3% of orthopedic departments having a policy of stopping aspirin and 97.3% stopping warfarin before neck or femur surgery. These studies highlight the need for evidence-based guidelines for the perioperative management of patients on aspirin, warfarin, and clopidogrel in surgical settings [19,20].
Connor and Wingate [5] surveyed 91 radiology departments and 138 urology departments who perform prostate biopsies in the United Kingdom and found a wide variation in practice. In that study, 52% of radiologists and 27% of urologists reported terminating aspirin 5 to 12 days before TRUS biopsy.
A prospective study to determine whether low-dose aspirin increases morbidity after 6-core TRUS biopsy was recently performed [21]. In this cohort study, 36 patients were taking aspirin before TRUS biopsy compared with 177 patients who were not taking aspirin before TRUS biopsy. This study demonstrated no statistically significant difference in the incidence of hematuria or overall bleeding after TRUS biopsy between the group on aspirin and the group not on aspirin. In our study, 12-core TRUS biopsy was performed on all patients as compared with 6-core TRUS biopsy in Maan's study [21]. In our study, the incidence of hematuria was less at 46% in group I compared with 63% in group II (p=0.018). The incidence of hematospermia was 6% and 10% in groups I and II, respectively.
More recently, strong evidence has appeared in the current literature to support continuation of anticoagulation/antiplatelet therapy without additional morbidity [5,21-24]. By contrast, Halliwell et al. [22] compared 387 patients on aspirin versus 731 patients not on antiplatelet or anticoagulation therapy (control). In Halliwell's study [22], the incidence of hematuria and rectal bleeding was higher in the aspirin users than in the control group (72% vs. 61%, p<0.01, and 21% vs. 13%, p<0.001, respectively), but there were no significant differences in hematospermia. In addition, severe bleeding was very uncommon in both groups and no patients required intervention for bleeding complications [22].
Another comparative study by Giannarini et al. [23] reported on patients receiving aspirin (n=67) while undergoing 10-core TRUS biopsy. The overall bleeding rate in the aspirin group was not significantly higher at 78.5% than the 81.5% in the control group (non-aspirin-users). Giannarini et al. [23] concluded that no significant bleeding difference existed for hematuria, rectal bleeding, or hematospermia.
Ihezue et al. [24] evaluated the morbidity of 49 patients on warfarin therapy undergoing TRUS biopsy (mean INR, 2.2). The incidence of hematuria was 36.7% and 60.2% in the warfarin and control groups, respectively. In addition, the incidence of hematospermia was 8.2% and 21% in the warfarin and control groups, respectively. The incidence of rectal bleeding was slightly higher in the warfarin group at 14.3% than the 13% in the control group.
In our study, there was no statistical difference in the occurrence of rectal bleeding in either group. In addition, neither group of patients experienced significant rectal bleeding complications. In addition, patients in group I experienced fewer hematuria episodes than did the control group. We are unable to explain this; however, it could also be argued that, because people receiving anticoagulants are accustomed to a tendency to bleed easily, they might view their post-biopsy bleeding with less concern than would those not receiving anticoagulant therapy. Hence, a greater percentage of the control group would report hematuria and hematospermia. This may not be the case, however, because all patients in both groups had a discussion with the doctor who performed the TRUS biopsy, who requested that they record any episodes of bleeding, however small.
In the urological setting, the discontinuation of clopidogrel before TRUS biopsy is widely practiced among urologists in the United Kingdom [19]. The clinical application of the dual therapy of aspirin and clopidogrel is ideally prescribed for patients undergoing coronary stenting for up to 1 year after implantation [9]. Although this combination has been shown to significantly reduce the incidence of ischemic cardiovascular events, adding clopidogrel on top of daily aspirin therapy further increases the risk of bleeding [12]. In our study, TRUS biopsy was performed on 13 patients (15%) receiving clopidogrel (3 receiving clopidogrel alone and 10 receiving clopidogrel and aspirin). Although four patients in group I were on dual therapy of aspirin and warfarin for atrial fibrillation, none of the patients developed a significant bleeding complication. One would expect an increased incidence of bleeding complications in these subgroups. One patient on dual therapy of clopidogrel and aspirin for drug-eluting coronary stents developed clot retention following TRUS biopsy and required hospitalization.
The results of this multigroup study suggest that it is safe to continue with anticoagulation/antiplatelet treatment before TRUS biopsy. In addition, the results highlight the urgent need for large randomized trials to systematically evaluate the safety of continuation of anticoagulation/antiplatelet therapy in patients undergoing TRUS biopsy, particularly in relation to clopidogrel. This is also the first discussion of the effects of clopidogrel in patients undergoing TRUS biopsy. Future research should focus on increasing the sample size to increase the statistical power of the study. Another research facet should be directed to evaluating the radiological aspects of the prostatic changes following TRUS biopsy in patients receiving anticoagulant/antiplatelet therapy.
Figures and Tables
References
1. Ghani KR, Dundas D, Patel U. Bleeding after transrectal ultrasonography-guided prostate biopsy: a study of 7-day morbidity after a six-, eight- and 12-core biopsy protocol. BJU Int. 2004. 94:1014–1020.
2. Raaijmakers R, Kirkels WJ, Roobol MJ, Wildhagen MF, Schrder FH. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology. 2002. 60:826–830.
3. Burger W, Chemnitius JM, Kneissl GD, Rücker G. Low-dose aspirin for secondary cardiovascular prevention - cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation - review and meta-analysis. J Intern Med. 2005. 257:399–414.
4. Travis S, Wray R, Harrison K. Perioperative anticoagulant control. Br J Surg. 1989. 76:1107–1108.
5. Connor SE, Wingate JP. Management of patients treated with aspirin or warfarin and evaluation of haemostasis prior to prostatic biopsy: a survey of current practice amongst radiologists and urologists. Clin Radiol. 1999. 54:598–603.
6. Nambirajan T, Woolsey S, Mahendra V, Walsh IK, Lynch TH, Keane PF. Efficacy and safety peri-prostatic local anaesthetic injection in trans-rectal biopsy of the prostrate: a prospective randomised study. Surgeon. 2004. 2:221–224.
7. Douketis JD, Berger PB, Dunn AS, Jaffer AK, Spyropoulos AC, Becker RC, et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 299S–339S.
8. Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). J Am Coll Cardiol. 2003. 41:159–168.
9. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, Jacobs AK, Kern MJ, King SB 3rd, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention). Circulation. 2006. 113:e166–e286.
10. Mehta SR, Yusuf S, Peters RJ, Bertrand ME, Lewis BS, Natarajan MK, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001. 358:527–533.
11. Steinhubl SR, Berger PB, Mann JT 3rd, Fry ET, DeLago A, Wilmer C, et al. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002. 288:2411–2420.
12. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006. 119:624–638.
13. Chassot PG, Delabays A, Spahn DR. Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth. 2007. 99:316–328.
14. Pickard AS, Becker RC, Schumock GT, Frye CB. Clopidogrel-associated bleeding and related complications in patients undergoing coronary artery bypass grafting. Pharmacotherapy. 2008. 28:376–392.
15. Pass SE, Simpson RW. Discontinuation and reinstitution of medications during the perioperative period. Am J Health Syst Pharm. 2004. 61:899–912.
16. Dunning J, Versteegh M, Fabbri A, Pavie A, Kolh P, Lockowandt U, et al. Guideline on antiplatelet and anticoagulation management in cardiac surgery. Eur J Cardiothorac Surg. 2008. 34:73–92.
17. Cahill RA, McGreal GT, Crowe BH, Ryan DA, Manning BJ, Cahill MR, et al. Duration of increased bleeding tendency after cessation of aspirin therapy. J Am Coll Surg. 2005. 200:564–573.
18. Go AS, Hylek EM, Chang Y, Phillips KA, Henault LE, Capra AM, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA. 2003. 290:2685–2692.
19. Mukerji G, Munasinghe I, Raza A. A survey of the peri-operative management of urological patients on clopidogrel. Ann R Coll Surg Engl. 2009. 91:313–320.
20. Palan J, Odutola A, White SP. Is clopidogrel stopped prior to hip fracture surgery--A survey of current practice in the United Kingdom. Injury. 2007. 38:1279–1285.
21. Maan Z, Cutting CW, Patel U, Kerry S, Pietrzak P, Perry MJ, et al. Morbidity of transrectal ultrasonography-guided prostate biopsies in patients after the continued use of low-dose aspirin. BJU Int. 2003. 91:798–800.
22. Halliwell OT, Yadegafar G, Lane C, Dewbury KC. Transrectal ultrasound-guided biopsy of the prostate: aspirin increases the incidence of minor bleeding complications. Clin Radiol. 2008. 63:557–561.
23. Giannarini G, Mogorovich A, Valent F, Morelli G, De Maria M, Manassero F, et al. Continuing or discontinuing low-dose aspirin before transrectal prostate biopsy: results of a prospective randomized trial. Urology. 2007. 70:501–505.
24. Ihezue CU, Smart J, Dewbury KC, Mehta R, Burgess L. Biopsy of the prostate guided by transrectal ultrasound: relation between warfarin use and incidence of bleeding complications. Clin Radiol. 2005. 60:459–463.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download