Abstract
Purpose
In the endoscopic treatment of vesicoureteral reflux, the relatively high rate of success, the simplicity of the procedure, high patient compliance, and a lack of complications has led to the increased development of injection materials and techniques. We report a method of identifying and maintaining a clear visual field during ureteral and bladder submucosal wall injection of a dextranomer/hyaluronic acid copolymer (Deflux, Oceana, Therapeutics Inc.) by use of the hydrodistention implantation technique (HIT) with the aid of temporary ureteral catheter insertion.
Materials and Methods
We prospectively reviewed patients with grade IV or V reflux who received an endoscopic injection of Deflux. Reflux grade was evaluated before and after treatment (3 months) by use of voiding cystourethrograms. Conventional sub-trigonal injection (STING) was performed with injection of Deflux underneath the bladder mucosa at the 6 o'clock position. HIT was performed either with hydrodistention or with guidewire insertion. These techniques increase visualization of the intramural portion of the distal ureteral wall. Patients with treatment failures were offered reinjection up to three times.
Results
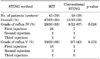
Sixty-three patients completed endoscopic injection and follow-up of 3 months. The overall resolution rate for conventional STING was 58%, i.e., 67% for grade IV and 43% for grade V. The overall resolution rate for HIT was 80%, i.e., 93% for grade IV and 66% for grade V. The modified methods showed higher resolution rates for overall cure owing to the success in patients with grade IV reflux (p=0.026). Although the success of grade V treatment was higher with the modified method, the success rate was not statistically significant (p=0.27).
Vesico-ureteral reflux (VUR) is an abnormal movement of urine from the bladder into the ureters or kidneys. VUR affects approximately 1 to 3% of all children [1,2], making it the most common pediatric anomaly of the urinary tract [3]. Although long-term prophylaxis is generally recommended as the first choice of therapy for low-grade VUR, high-grade VUR has a much lower expectancy of spontaneous resolution, with only 52% of cases reported as solved at 10 years of follow-up [4,5]. For high-grade VUR, ureteroneocystostomy has been the gold standard of therapy, with a success rate of over 95%. However, surgery is not free of complications, with obstructions occurring in 0.3% to 9.1% of cases, and grade V VUR has been reported to be resistant to treatment in 20% of cases after reimplantation [6].
Since its introduction in the 1980s, endoscopic treatment has become a valid alternative either to antibiotic prophylaxis (in low-grade reflux) or to open surgery (in high-grade reflux). Across several studies, the method showed a resolution rate of 70 to 90% [7-9]. Although not as effective as open ureteral reimplantation, endoscopic correction of VUR offers a minimally invasive, outpatient procedure with a low risk of complications. Although seemingly simple, the resolution rate of the procedure has been increased with several changes in both materials and techniques [10,11].
The general method does not deviate greatly from the initial sub-trigonal injection (STING) method of Puri [12], which was originally designed for injecting polytetrafluoroethylene. The success rate of the conventional STING method is 88%, 75%, and 52% for grade II, III, and IV VUR, respectively [9]. Several attempts have been made to improve the resolution rate of high-grade VUR. The modified STING procedure, later known as the hydrodistention implantation technique (HIT), was introduced in 2004 [13]. The conventional STING procedure is performed under the bladder mucosa, 2 to 3 mm below the affected ureteric orifice, at the 6 o'clock position; in contrast, the modified technique is performed under the assistance of hydrodistention of the orifice, which increases visualization of the injection site and allows needle insertion approximately 4 mm in the submucosa of the mid to distal ureteral tunnel, at the same 6 o'clock position [13].
Since 2004, our center has introduced Deflux injections for children with high-grade VUR. After originally practicing the conventional STING method, we adopted the HIT method. In this study, we present a prospective comparison of the treatment efficacy between the HIT method and conventional STING in children with high-grade VUR.
We prospectively reviewed all cases of endoscopic injection of Deflux by either the STING or HIT method for patients diagnosed with grade IV or V VUR who underwent treatment at the Korea University Hospital from February 2004, when our first experience with the use of this treatment occurred, to March 2010. All enrolled patients had VUR as determined by voiding cystourethrogram (VCUG) and further classification according to the International Reflux Study in Children.
We used the standard criteria for intervention, as follows: breakthrough urinary tract infection during antibiotic prophylaxis, progressive renal scarring, noncompliance with medical therapy, nonresolution of VUR, and parental preference. We excluded from the study patients with more complicated urinary anomalies, such as ectopic ureter, ureterocele, and neurogenic bladder, as determined by history or failed surgical reimplantation. All patients' guardians were given treatment options based on the AUA Pediatric Vesicoureteral Clinical Guidelines, according to the patients' age, severity of reflux, and presence of scarring. During the study period, all procedures were performed by a single surgeon, with the patient under general anesthesia, with the use of injection of a dextranomer/hyaluronic acid copolymer (Deflux, Oceana Therapeutics Inc., Edison, NJ, USA). A Wolf 9.5 Fr pediatric cystoscope with an offset lens was used in all cases.
The technique of endoscopic treatment used in this study was similar to that originally described by O'Donnell and Puri for polytetrafluoroethylene injection [12]. The 3.7 Fr needle was placed under the bladder mucosa 2 to 3 mm below the affected ureteral orifice, at the 6 o'clock position, and Deflux was injected inside the lumen until adequate mound morphology was attained.
The modified technique is based on that described by Kirsch et al. [13] The bladder is filled to half to three-quarters volume to permit visualization of the ureter and to avoid distortion and tension within the submucosal layer of the ureter secondary to overdistention. We directed a pressured stream of irrigation fluid into the ureter (hydrodistention) or inserted a guidewire to define the site of injection within the ureteral submucosa.
After confirmation of the shape and form distorted by hydrodistention, a flexible guidewire was additionally placed in the ureteral tunnel in case of the need to further enhance visualization of the ureter injection site. The guidewire was removed when the needle was placed at the injection site, so we were able to observe whether the morphology of the ureteral orifice was turning into a mound shape and whether an adequate degree of ureteral coaptation occurred. The injection site was approximately 4 mm in the submucosa of the mid to distal ureteral tunnel, at the 6 o'clock position (Fig. 1). The Deflux was injected into the submucosal intraureteral space, tracking along the entire length of the detrusor tunnel.
Follow-up VCUGs were performed between 3 months and 1 year after the operation. Antibiotic prophylaxis was continued until resolution of reflux was demonstrated on follow-up imaging. Successful surgical treatment was defined as complete disappearance of VUR. Patients who failed were offered reinjection up to three times.
Results are presented as mean values±SDs or as n values (range). According to the STING method, patients were divided into two groups and variables were analyzed with the Student's t-test, chi-square test, linear-by-linear association test, and simple correlation analysis by use of SPSS ver. 13 (SPSS Inc., Chicago, IL, USA). Differences were considered statistically significant at p<0.05.
A total of 78 ureters in 36 boys and 27 girls were treated, including 15 bilateral cases. A total of 63 patients were followed up for at least 3 months. The HIT procedure was performed in 45 patients, including 14 bilateral cases (59 ureters; grade IV VUR in 30 and grade V in 29), whereas the conventional procedure was performed in 18 patients, including 1 bilateral case (19 ureters; grade IV in 12 and grade V in 7). The general characteristics of the patients (age, gender, and follow-up period) and the vesico-ureteral reflux grades are listed and statistically analyzed in Table 1.
As mentioned above, we offered reinjection up to three times in situations in which the first treatment failed. Complete resolution occurred in 58% (11/19 ureters) of patients who received conventional STING, including 67% (8/12) of grade IV patients and 43% (3/7) of grade V patients. In contrast, the overall cure rate for patients who underwent HIT was 80% (47/59 ureters), including 93% (28/30) of grade IV patients and 66% (19/29) of grade V patients. Thus, HIT showed a significantly higher success rate than did the conventional method in patients with grade IV VUR (p=0.026). In patients with grade V VUR, although the cure rate (66%) was higher in group 2 than in group 1 (43%), the difference was not statistically significant (p=0.270) (Table 2).
In patients with grade IV VUR, the first injection was successful in 86.7% and 51.7% cases for the modified and conventional methods, respectively (p=0.028), whereas in patients with grade V VUR, the two methods solved VUR at the first attempt in 51.7% and 28.6% cases, respectively. The success rates decreased for the second and third injections. The number of patients requiring repeated injections was too small for any significant statistical analysis to identify common traits. Although all six patients who required repeated injections were bilateral cases, we found no significant difference in male-to-female ratio (4:2) or age.
There were no significant complications related to either of the two methods (i.e., conventional or modified). One child in the HIT group complained of moderate flank pain with persistent hydronephrosis several hours after the procedure. However, the symptoms resolved within a few hours. The hydronephrosis also disappeared at follow-up in 1 month.
Since its introduction, endoscopic surgery for VUR has gained great popularity owing to its low invasiveness and high efficacy. In many centers, single or repeated injections for VUR have replaced ureteral reimplantation [14]. Several obvious benefits are driving this trend, including a short operative time, greater patient satisfaction, lower morbidity, and reduced cost [15]. Although the medical cost may vary, the physical and mental burden is significantly decreased [16].
However, no reported study has approached the cure rate of ureteral reimplantation. Older studies from more than 10 years ago usually cite a resolution rate of 60 to 75%, depending on the material used [7,17]. The success rates have improved through the development of new techniques and refinement of materials. Recent reports on Deflux injection have consistently shown success rates above 90% with either single or repeated injections [8,18,19]. Our study showed an overall success rate of 80% for the modified method, reaching 93% for grade IV VUR.
Several significant factors should be considered in these optimistic evaluations. One of the limitations of this treatment is that despite the apparently simple procedure, the high resolution rates in all the cited studies sometimes required multiple, repeated injections; modification and refinement of the technique; and an obvious learning curve [8,10,18,20]. Our study also showed a significant improvement of the resolution rate with a modification of the method, from 58% with conventional STING to 80% with the HIT method, further applied by insertion of a ureteral catheter. Considering that this improvement was brought about without a change of materials, we believe that further applications may allow for even more improvement. The one caveat is that we did not suggest the excellence of using a guidewire during the procedure. As an application of the technique previously described by Kirsh, we ultimately used the guidewire as intraluminal hydrodistention when we needed to enhance visualization. Whereas submucosal injections have been applied previously in other methods, the intraluminal portion was the site of injection in this method, owing to the effect of hydrodistention.
Similar to other studies, we found cases resistant to treatment. In our study, 20% of patients did not improve when treated with the modified technique. Other studies also found that approximately 10% of patients are resistant to treatment [18,19]. Unfortunately, these patients have not been clearly characterized.
In line with previous results, we found a significant decrease in the success rate of surgical treatment in children suffering from grade V VUR, compared with grade IV, even with the modified injection method. In a study of 52 patients (80 ureters), Lavelle et al. [20] reported a success rate of 82% to 73% for grade I to IV and suggested ureteral orifice morphology as the primary predictive factor for treatment success. Another study by Dave et al. [10] suggested that the minimum injection volume of 0.8 ml per ureter was a determinant for treatment success, along with the surgeon's experience and low reflux grade. The study presented various success rates, ranging from 100% for grade I to 46.6% for grade V. Higham-Kessler et al. [21] also categorized mound morphology and suggested that the shifted mound shape was associated with recurrence and need for reinjection. These results suggested that orifice morphology was associated with either primary treatment failure or recurrence. Similarly, previous injections with smaller particles, such as polytetrafluoroethylene, were primarily criticized for the inability of the material to maintain mound morphology because of migration [22-24]. Although mound morphology may be critical for maintaining treatment effects, the treatment failure groups were heterogeneous in these studies. In our group of patients treated with the HIT method, the difference in the success rate of 93% and 66% for grade IV and V VUR was too large to consider the a common denominator for failure across all VUR grades.
In our experience, one of the main difficulties with recreating a proper volcanic-shaped mound by injection in a grade V VUR ureter is caused by the decreased thickness of the injection site. Other studies have also found a significant decrease in the wall thickness of the ureteral wall outside the bladder, which is our primary point of injection [25]. Studies of refluxing distal ureters have noted a decrease in smooth muscle cells, which are replaced with less elastic collagen type III fibers in these patients [25,26]. The lack of elasticity in the distal ureter, as well as the bladder mucosa covering the ureteral orifice, seems to resist reshaping by injectable materials. Optimal mound morphology is achieved with difficulty, often requiring multiple injection sites and more injection material.
Other urodynamic factors may also cause treatment failures. In other words, we need to consider the bladder not only anatomically, but also etiologically. For example, some children have difficulty relaxing the sphincter during urination and void against the sphincter, straining the bladder muscle extensively in the process, thus resulting in inefficient voiding. These abnormal voiding patterns are referred to as the dysfunctional elimination syndrome (DES). The high pressure generated by muscles straining against themselves may break down the one-way mechanism of urine flow that normally prevents urine from going back up into the kidneys from the bladder. It may also impede the flow of urine from the kidneys into the bladder. Thus, Koff et al reported that 66 of 143 (43%) cases with primary VUR were accompanied by DES. Moreover, 54 patients (82%) presented with urinary tract infection, and spontaneous resolution was delayed in DES patients. Unfortunately, we could not investigate these etiologies, because we did not perform videourodynamic study.
For the sake of homogeneity of the treatment population, our study focused on high-grade VUR and therefore could not identify other uncontrolled factors to suggest a definite comparison between the conventional and modified methods. One such factor is surgeon experience. As suggested by Dave et al. [10] surgeon experience is a significant factor in controlling the outcome of treatment. Our study was not performed in a parallel manner between the two methods, because the modified treatment was used more recently than the conventional method. However, our overall success rates are in line with previous results comparing the treatment success rates between the conventional and HIT methods [14,27]. Expanding the current patient pool and comparing data with previous results could be useful for identifying the role of surgeon's experience in the treatment outcomes.
We consider that the success of the procedure depends on coapting the ureteral tunnel, similar to the nonrefluxing ureter or the one corrected surgically. To establish this goal, the needle is placed in the ureteral tunnel and Deflux is injected in the submucosal intraureteral space, tracking along the entire length of the detrusor tunnel. It is technically easier to perform in ureters with higher grade VUR, because the needle may be more feasibly placed in an advantageous position in the ureteral submucosal space.
The majority of children with VUR undergoing HIT with Deflux were cured after 1 treatment. This was our preferred method of implant injection for the correction of high-grade VUR and produced an overall resolution rate of 80% (47/59 ureters), reaching 93% (28/30) in patients with grade IV VUR. The technique optimizes the ureteral coaptation and is easy to perform and is not associated with any significant short-term complications. Thus, we consider that the HIT procedure by hydrodistention or ureteral catheter-aided visualization is an effective treatment for high-grade VUR.
Figures and Tables
FIG. 1
(A) HIT method modified with guidewire-assisted identification of the injection site. (B) Post-injection mound morphology at the ureteral orifice.

References
1. Hodson EM, Wheeler D, Vimalchandra D, Smith G, Craig JC. Interventions for primary vesicoureteric reflux. Cochrane Database Syst Rev. 2007. (3):CD001532.
2. Cooper CS. Diagnosis and management of vesicoureteral reflux in children. Nat Rev Urol. 2009. 6:481–489.
3. Jacobson SH, Hansson S, Jakobsson B. Vesico-ureteric reflux: occurrence and long-term risks. Acta Paediatr Suppl. 1999. 88:22–30.
4. Smellie JM, Jodal U, Lax H, Möbius TT, Hirche H, Olbing H, et al. Outcome at 10 years of severe vesicoureteric reflux managed medically: report of the International Reflux Study in Children. J Pediatr. 2001. 139:656–663.
5. Jodal U, Smellie JM, Lax H, Hoyer PF. Ten-year results of randomized treatment of children with severe vesicoureteral reflux. Final report of the International Reflux Study in Children. Pediatr Nephrol. 2006. 21:785–792.
6. Elder JS, Peters CA, Arant BS Jr, Ewalt DH, Hawtrey CE, Hurwitz RS, et al. Pediatric vesicoureteral reflux guidelines panel summary report on the management of primary vesicoureteral reflux in children. J Urol. 1997. 157:1846–1851.
7. Puri P, Granata C. Multicenter survey of endoscopic treatment of vesicoureteral reflux using polytetrafluoroethylene. J Urol. 1998. 160(3 Pt 2):1007–1011.
8. Puri P, Chertin B, Velayudham M, Dass L, Colhoun E. Treatment of vesicoureteral reflux by endoscopic injection of dextranomer/hyaluronic acid copolymer: preliminary results. J Urol. 2003. 170(4 Pt 2):1541–1544.
9. Capozza N, Lais A, Nappo S, Caione P. The role of endoscopic treatment of vesicoureteral reflux: a 17-year experience. J Urol. 2004. 172(4 Pt 2):1626–1628.
10. Dave S, Lorenzo AJ, Khoury AE, Braga LH, Skeldon SJ, Suoub M, et al. Learning from the learning curve: factors associated with successful endoscopic correction of vesicoureteral reflux using dextranomer/hyaluronic acid copolymer. J Urol. 2008. 180:4 Suppl. 1594–1599.
11. Kirsch AJ, Perez-Brayfield MR, Scherz HC. Minimally invasive treatment of vesicoureteral reflux with endoscopic injection of dextranomer/hyaluronic acid copolymer: the Children's Hospitals of Atlanta experience. J Urol. 2003. 170:211–215.
12. O'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed). 1984. 289:7–9.
13. Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol. 2004. 171(6 Pt 1):2413–2416.
14. Cerwinka WH, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux associated with paraureteral diverticula in children. J Urol. 2007. 178(4 Pt 1):1469–1473.
15. Kobelt G, Canning DA, Hensle TW, Läckgren G. The cost-effectiveness of endoscopic injection of dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. J Urol. 2003. 169:1480–1485.
16. Stenberg A, Lackgren G. Treatment of vesicoureteral reflux in children using stabilized non-animal hyaluronic acid/dextranomer gel (NASHA/DX): a long-term observational study. J Pediatr Urol. 2007. 3:80–85.
17. Stenberg A, Läckgren G. A new bioimplant for the endoscopic treatment of vesicoureteral reflux: experimental and short-term clinical results. J Urol. 1995. 154(2 Pt 2):800–803.
18. Yu RN, Roth DR. Treatment of vesicoureteral reflux using endoscopic injection of nonanimal stabilized hyaluronic acid/dextranomer gel: initial experience in pediatric patients by a single surgeon. Pediatrics. 2006. 118:698–703.
19. Kirsch A, Hensle T, Scherz H, Koyle M. Injection therapy: advancing the treatment of vesicoureteral reflux. J Pediatr Urol. 2006. 2:539–544.
20. Lavelle MT, Conlin MJ, Skoog SJ. Subureteral injection of Deflux for correction of reflux: analysis of factors predicting success. Urology. 2005. 65:564–567.
21. Higham-Kessler J, Reinert SE, Snodgrass WT, Hensle TW, Koyle MA, Hurwitz RS, et al. A review of failures of endoscopic treatment of vesicoureteral reflux with dextranomer microspheres. J Urol. 2007. 177:710–714.
22. Henly DR, Barrett DM, Weiland TL, O'Connor MK, Malizia AA, Wein AJ. Particulate silicone for use in periurethral injections: local tissue effects and search for migration. J Urol. 1995. 153:2039–2043.
23. Bhatti HA, Khattak H, Boston VE. Efficacy and causes of failure of endoscopic subureteric injection of Teflon in the treatment of primary vesicoureteric reflux. Br J Urol. 1993. 71:221–225.
24. Malizia AA Jr, Reiman HM, Myers RP, Sande JR, Barham SS, Benson RC Jr, et al. Migration and granulomatous reaction after periurethral injection of polytef (Teflon). JAMA. 1984. 251:3277–3281.
25. Yurtçu M, Gürbüzer N, Findik S, Avunduk MC, Günel E. Investigation of histopathologic changes in the ureter walls in vesicoureteral reflux. J Pediatr Surg. 2009. 44:802–805.
26. Lee BR, Silver RI, Partin AW, Epstein JI, Gearhart JP. A quantitative histologic analysis of collagen subtypes: the primary obstructed and refluxing megaureter of childhood. Urology. 1998. 51:820–823.
27. Kirsch A, Elmore J, Molitierno J, Scherz H, editors. The double HIT methodology for the endoscopic correction of vesicoureteral reflux. Proceedings of the Annual Meeting of the American Urological Association. 2006 May 20-25; Atlanta, USA. Linthicum: American Urological Association.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download