Abstract
Purpose
The aim of this study was to assess the long-term clinical outcomes of the tension-free vaginal tape (TVT) procedure for stress urinary incontinence (SUI) in elderly women and to identify the factors influencing failure in these cases.
Materials and Methods
Women with SUI who underwent a TVT procedure were studied. "Cure" was defined as no urine leakage at all in any circumstances and "improvement" was defined as some urine leakage but a score of over 4 points out of 5 in a satisfaction inquiry. Patients were divided into two groups (middle-aged, <65 years and elderly, ≥65 years) for comparison of clinical outcomes. In the elderly group, patients were subdivided into two groups (cure and no cure groups) and were compared to identify the factors influencing failure.
Results
A total of 136 women (middle-aged group, 106; elderly group, 30) were enrolled in the study. The mean ages of the patients in the 2 groups were 53.5±5.9 and 72.0±5.0 years and the mean follow-up times were 50.5±9.4 and 48.8±9.1 months, respectively. The cure and improvement rates in the middle-aged and elderly groups were 80.2% vs. 66.7% and 4.7% vs. 3.3%, respectively (p>0.05). The satisfaction scores in the middle-aged and elderly groups were 3.8±1.1 vs. 3.3±1.5 points (p>0.05). In the elderly group, the body mass index of the cure and no cure groups were 24.6±3.3 kg/m2 and 26.6±1.0 kg/m2, and body mass index was the only factor that differed significantly between the two subgroups (p=0.028).
Urinary incontinence is not a life-threatening disorder; however, it can significantly affect a woman's health. Today, elderly women are a rapidly growing segment of the population in the industrialized world, and the prevalence of urinary incontinence increases as patients age. Aging women today are healthier than the previous generation owing to an improved general health care system, and they also seek surgical treatment for incontinence.
In the most recent publication, Lee et al. [1] reported a 6-year follow-up cure rate after the tension-free vaginal tape (TVT) procedure of 83.0% with a satisfaction rate of 80.1%. However, the effect of age on the outcomes of the TVT procedure is relatively undefined. Various studies have reported cure rates between 67% and 85.3% with 24 months of follow-up [2-4].
The aim of this study was to examine whether the TVT procedure is a successful and safe procedure for the long-term treatment of stress urinary incontinence (SUI) in elderly women aged 65 years or over and to identify the factors influencing failure in these cases.
The study sample included 241 consecutive women who underwent a TVT procedure performed by a single urologist surgeon between August 2005 and July 2008. At the time of follow-up, 136 patients had been contacted through routine postoperative visits or by telephone for an extensive interview.
Patients were divided into two groups: the middle-aged group (<65 years) and the elderly group (65 years old or older). Demographics, urodynamic study, and surgical variables were reviewed in a retrospective manner and were compared between the two groups.
Patients were asked about SUI symptoms by use of Sandvik's incontinence severity index [5] and their satisfaction with the TVT procedure by a single urology investigator at the final contacts. Women responded with a satisfaction score based on a 5-point Likert-type scale as 1 (completely dissatisfied), 2 (mostly dissatisfied), 3 (neutral), 4 (mostly satisfied), or 5 (completely satisfied). Cure rate, improvement rate, failure rate, satisfaction score, and incontinence severity after TVT failure on the basis of the questionnaires were compared between the middle-aged and the elderly group. "Cure" was defined as patients answering as having no urine leakage at all in any circumstances, and "improvement" was defined as patients answering as having some urine leakage but over 4 points out of 5 in the satisfaction inquiry. "Failure" was defined as patients answering as having some urine leakage and at most 3 points out of 5 in the satisfaction inquiry.
Elderly patients were also subdivided into the cure group and the no cure group. Demographics, urodynamic studies, and surgical variables were compared between the two subgroups to identify the factors influencing TVT procedure failure.
Student's t-tests and chi-square tests were applied. Reported p-values were two-sided and a p-value of 0.05 was considered statistically significant for all comparisons. Statistical analysis was performed with SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
The patients were divided into two groups according to age: the middle-aged group (n=106) and the elderly group (n=30). All TVT procedures were performed as previously described by Ulmsten et al. [6], except that surgeries were carried out with the patient under general or spinal anesthesia.
The patients' mean age was 53.5±5.9 years (range, 35 to 64 years) for the middle-aged group and 72.0±5.0 years (range, 65 to 82 years) for the elderly group. The mean follow-up time was 50.5±9.4 months (range, 36 to 70 months) and 48.8±9.1 months (range, 36 to 69 months), respectively. Twenty-nine women (27.4%) in the middle-aged group and 18 women (60%) in the elderly group had concomitant medical diseases, such as diabetes, hypertension, and cerebrovascular disease; this was significantly different between the two groups (p=0.002). Five women (4.72%) in the middle-aged group and seven (23.3%) in the elderly group underwent concomitant cystocele repair; this was also significantly different between the two groups (p=0.001). Parity, body mass index (BMI), and previous operation history showed no statistically significant differences between the two groups (p>0.05).
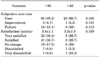
Concerning urodynamic parameters, the maximum urethral closure pressure (MUCP) in the middle-aged group was 78.1±44.7; that in the elderly group was 50.7±26.3 cmH2O (p=0.002). Other parameters, such as detrusor overactivity, maximum flow rate, post-voided residual urine (PVR), Valsalva leak point pressure (VLPP), and the urethral hypermobility rate, were not significantly different between the two groups (Table 1).
Concerning long-term clinical outcomes based on the patients' subjective symptoms, the cure rate, improvement rate, and failure rate were 80.2% vs. 66.7%, 4.7% vs. 3.3%, and 15.1% vs. 30%, respectively. Satisfaction scores in the middle-aged and elderly groups were 3.8±1.1 and 3.3±1.5 points, respectively. These parameters showed no statistically significant differences (p>0.05) (Table 2). In the middle-aged group, de novo urgency was 31.3%, and 60.3% of the patients were cured of their overactive bladder symptoms after the TVT procedure. In the elderly group, de novo urgency was 28.5%, and 42.9% of the patients were cured of their overactive bladder symptoms after the TVT procedure.
For surgical outcomes, in the elderly group, one patient had vaginal erosion, one had urinary tract infection, and one had urinary retention. In the middle-aged group, there were no postoperative complications during the follow-up.
In the elderly group, according to the multivariate analysis, age, concomitant medical disease, concomitant overactive bladder symptoms, MUCP, VLPP, and urethral hypermobility were not significantly different between the cure and no cure subgroups (p>0.05). The only significant parameter was BMI. The BMI of the cure and no cure subgroups was 24.6±3.3 kg/m2 and 26.6±1.0 kg/m2, which was significantly different (p=0.028) (Table 3).
Urinary incontinence is not a life-threatening disorder; however, it can significantly affect a woman's psychological, emotional, sexual, and social functioning. The prevalence of urinary incontinence has been reported to be between 10% and 40% in women older than 70 years and it increases as women age [7]. The increased prevalence of incontinence in late life reflects the compounding effects of functional deterioration and coincidental disability.
From a urological point of view, intrinsic sphincter deficiency increases in prevalence with advancing age as the result of a combination of factors, such as decreased estrogenization, age-related atrophy of the urethral tissue, and increased likelihood of a previous incontinence procedure. Furthermore, older women may have had a lesser degree of urethral mobility or greater degrees of urethral rigidity, thus reducing tape effectiveness as well as detrusor instability and symptoms of urgency [8].
As patients age, morbidity and mortality from surgery increase. Regarding the surgical risks, some studies have suggested that preexisting comorbidities, and not age, are the predominant determinants of perioperative morbidity and mortality following urogynecologic surgeries [9,10]. By contrast, some other studies have shown that elderly women over the age of 60 years have an increased risk of mortality and morbidity compared with women younger than 60 following urogynecologic procedures regardless of comorbidities [11]. Furthermore, as patients age, new illnesses and new pharmacological treatments can negatively influence the outcome of the TVT operation. A possible negative impact of later pelvic surgery would also be considered as a negative factor [12].
Regarding these possibilities, the literature indicates that elderly women are excluded from most clinical trials for incontinence surgeries [13]. This might be because of the perception that such interventions are less effective and have more complications in the elderly population, and in the end, surgical procedures in elderly groups are performed less frequently.
Today, elderly women are healthier than ever before and recent literature suggests that currently performed procedures for SUI in elderly women are relatively safe and effective, although the exact surgical results and complications vary in different study populations. Sevestre et al. [3] reported that in the elderly group who were aged over 70 years old, the cure rate was 67% after 24 months of follow-up. Allahdin et al. [4] reported that in the elderly group who were aged over 70 years, the subjective cure rate was 85.3% and there were no significant differences in efficacy outcomes between the elderly and younger patients after 1 year of follow-up. In our study, we evaluated the clinical outcomes following the TVT procedure in patients 65 years old or older with a mean follow-up duration of 48 months. The success rates for TVT in the elderly and middle-aged groups in our study showed results similar to those of recent studies [14-16].The success rate of the elderly group was slightly lower than that of the middle-aged group in our study, and the complication rates were slightly higher in the elderly groups than in the middle-aged group without statistical significance. Significant comorbidities and concomitant surgeries occurred more often in the elderly group and may have been a cause of these results.
Various studies have reported that the factors predicting failure of the TVT procedure in the elderly are high BMI, low VLPP, rigid urethra, and a high grade of incontinence [17,18]. We evaluated the outcome of the TVT procedure and examined the factors influencing the outcome in elderly patients. In the multivariate analysis, our results showed that BMI was the only significant factor associated with the failure of the TVT procedure in elderly patients. Obese women have chronically increased stress of the pelvic floor, which is generally regarded as being causally related to the increased prevalence of urinary incontinence [19]. In addition, obesity is related to detrusor instability and many medical and neurogenic diseases [20]. This might be the major cause of failure of the TVT procedure in elderly women.
The limitations of our study include not having geriatric-specific measures of functional status such as activities of daily living in order to characterize the potential change in functional status with surgery. Other major limitations of the study include the relatively small number of elderly patients and the lack of objective outcome measures. A small cohort number can bias the study results, and a larger cohort number is needed to clarify our results. Our outcomes based on subjective symptoms from questionnaires at the interview used less stringent criteria when compared with other studies that used pad tests and filling cystometry. In addition, the prevalence of overactive bladder symptoms and symptom severity may increase as patients age. This can influence the outcomes of TVT surgery. However, in this study, we did not use any specific questionnaire to distinguish the severity of overactive bladder in our study groups.
Despite these limitations, we performed no patient selection and no special modifications of the surgical technique. Furthermore, our results encouraged us to perform the TVT procedure even in elderly women. As the number of older women seeking care for this debilitating condition continues to increase, we will continue to adequately counsel them with respect to the risks and benefits of surgery.
Figures and Tables
ACKNOWLEDGEMENTS
This work was supported by the Konkuk University Medical Center Research Grant 2010.
References
1. Lee JH, Cho MC, Oh SJ, Kim SW, Paick JS. Long-term outcome of the tension-free vaginal tape procedure in female urinary incontinence: a 6-year follow-up. Korean J Urol. 2010. 51:409–415.
2. Walsh K, Generao SE, White MJ, Katz D, Stone AR. The influence of age on quality of life outcome in women following a tension-free vaginal tape procedure. J Urol. 2004. 171:1185–1188.
3. Sevestre S, Ciofu C, Deval B, Traxer O, Amarenco G, Haab F. Results of the tension-free vaginal tape technique in the elderly. Eur Urol. 2003. 44:128–131.
4. Allahdin S, McKinley CA, Mahmood TA. Tension free vaginal tape: a procedure for all ages. Acta Obstet Gynecol Scand. 2004. 83:937–940.
5. Sandvik H, Espuna M, Hunskaar S. Validity of the incontinence severity index: comparison with pad-weighing tests. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:520–524.
6. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:81–85.
7. McGrother C, Resnick M, Yalla SV, Kirschner-Hermanns R, Broseta E, Müller C, et al. Epidemiology and etiology of urinary incontinence in the elderly. World J Urol. 1998. 16:Suppl 1. S3–S9.
8. Lo TS, Huang HJ, Chang CL, Wong SY, Horng SG, Liang CC. Use of intravenous anesthesia for tension-free vaginal tape therapy in elderly women with genuine stress incontinence. Urology. 2002. 59:349–353.
9. Toglia MR, Nolan TE. Morbidity and mortality rates of elective gynecologic surgery in the elderly woman. Am J Obstet Gynecol. 2003. 189:1584–1587.
10. Stepp KJ, Barber MD, Yoo EH, Whiteside JL, Paraiso MF, Walters MD. Incidence of perioperative complications of urogynecologic surgery in elderly women. Am J Obstet Gynecol. 2005. 192:1630–1636.
11. Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL. Effect of patient age on increasing morbidity and mortality following urogynecologic surgery. Am J Obstet Gynecol. 2006. 194:1411–1417.
12. Allahdin S, Harrild K, Warraich QA, Bain C. Comparison of the long-term effects of simple total abdominal hysterectomy with transcervical endometrial resection on urinary incontinence. BJOG. 2008. 115:199–204.
13. Morse AN, Labin LC, Young SB, Aronson MP, Gurwitz JH. Exclusion of elderly women from published randomized trials of stress incontinence surgery. Obstet Gynecol. 2004. 104:498–503.
14. Olsson I, Abrahamsson AK, Kroon UB. Long-term efficacy of the tension-free vaginal tape procedure for the treatment of urinary incontinence: a retrospective follow-up 11.5 years post-operatively. Int Urogynecol J. 2010. 21:679–683.
15. Liapis A, Bakas P, Creatsas G. Long-term efficacy of tension-free vaginal tape in the management of stress urinary incontinence in women: efficacy at 5- and 7-year follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:1509–1512.
16. Nilsson CG, Falconer C, Rezapour M. Seven-year follow-up of tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004. 104:1259–1262.
17. Lee KS, Choo MS, Doo CK, Han DH, Lee YS, Kim JY, et al. The long term (5-years) objective TVT success rate does not depend on predictive factors at multivariate analysis: a multicentre retrospective study. Eur Urol. 2008. 53:176–182.
18. Liapis A, Bakas P, Christopoulos P, Giner M, Creatsas G. Tension-free vaginal tape for elderly women with stress urinary incontinence. Int J Gynaecol Obstet. 2006. 92:48–51.
19. Subak LL, Johnson C, Whitcomb E, Boban D, Saxton J, Brown JS. Does weight loss improve incontinence in moderately obese women? Int Urogynecol J Pelvic Floor Dysfunct. 2002. 13:40–43.
20. Cummings JM, Rodning CB. Urinary stress incontinence among obese women: review of pathophysiology therapy. Int Urogynecol J Pelvic Floor Dysfunct. 2000. 11:41–44.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download