Abstract
Purpose
To identify the predictors of death from other causes in patients with localized renal cell carcinoma (RCC).
Materials and Methods
We identified 1,101 patients with pathologically confirmed T1 or T2 RCC with a follow-up duration of over 6 months. Survival according to the cause of death was evaluated by using the Kaplan-Meier analysis with log-rank test. Prognostic factors for death from other causes were assessed by multivariate analysis using the Cox proportional hazard regression model. Once the prognostic factors were identified, a risk-group variable was created by counting the number of unfavorable features present for each patient.
Results
The median follow-up was 62 months, and RCC-related death occurred in 50 patients (4.5%), whereas death from other causes occurred in 47 (4.3%). Patients who died from other causes had a higher American Society of Anesthesiologist (ASA) score (26.1% vs. 10.2%; p=0.044), older age (63.4 years vs. 55.0 years; p<0.001), smaller mass size (5.1 cm vs. 7.9 cm; p<0.001), and lower nuclear grade (p=0.003). In the multivariate Cox regression analysis, older age, higher ASA score, and lower body mass index were independent factors predicting death from other causes in patients with localized RCC. On the basis of the number of risk factors for death from other causes, the 5-year other-cause-specific survival was 98.3% (0 risk factors), 84.7% (1 risk factor), and 67.6% (2 or 3 risk factors), respectively (p<0.001).
Over the past three decades, there has been a gradual increase in the incidence of renal cell carcinoma (RCC), coinciding with the widespread use of routine abdominal imaging [1]. However, despite an increase in early detection, overall death rates have not decreased, which suggests that treatment of these incidental renal masses may be of little or no benefit to some patients. Thus, the standard of care for localized RCC now includes active surveillance in selected patients with comorbidities or limited life expectancy. Several studies converging to support active surveillance have shown growth rates of approximately 0.28 cm per year [2], with only 1% progression to metastatic disease for patients undergoing active surveillance [3]. Given the natural history of localized RCC, the long-term benefit of aggressive treatment might depend in large part on competing risks of death. Thus, further analysis of mortality and cause of death is important to identify the risk factors for death following curative surgery for localized RCC. To address these unresolved issues, we evaluated the relationship between RCC and the risk of death and predictors of death from other causes in patients with localized RCC.
From 1989 to 2009, 1,101 consecutive patients with pathologically confirmed T1 or T2 RCC with a duration of follow-up of over 6 months were included in this study. Patients with lymph node or distant metastasis, multifocal tumors, or Von Hippel-Lindau disease were excluded. After approval by the Institutional Review Board at Seoul National University Hospital, clinical and pathological data from eligible patients were retrieved from the medical records and reviewed retrospectively.
Patient demographics including age, gender, body mass index (BMI), American Society of Anesthesiologist (ASA) score, symptoms at initial presentation, and type of surgery (radical nephrectomy or nephron-sparing surgery) were evaluated. Patients were categorized according to BMI based on the Asia-Pacific criteria for obesity as underweight (<18.5 kg/m2), normal weight (18.5 to 22.9 kg/m2), overweight (23 to 24.9 kg/m2), and obese (≥25 kg/m2) [4]. Histologic subtype was determined according to the Union for International Cancer Control/American Joint Committee on Cancer and Heidelberg recommendations [5], and tumor nuclear grade was determined according to the Fuhrman system [6]. The database of the Korea National Statistical Office was used to determine patient survival and cause of death if the patient was lost to follow-up.
Differences in demographics and clinical and pathological factors were examined by using the Student's t-test and chi-square test for continuous and categorical variables, respectively. Survival according to the cause of death was evaluated by Kaplan-Meier analysis with log-rank test, and prognostic factors for death from other causes were assessed by multivariate analysis with the Cox proportional hazard regression model in a forward stepwise regression. Once the prognostic factors were identified, a risk-group variable was created by counting the number of unfavorable features presented for each patient. Survival curves for each of these groups were estimated, and the groups were compared by using the log-rank test. All statistical analyses were performed with the use of the statistical software SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), and p<0.05 (two sided) was considered statistically significant.
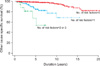
The median follow-up for 1,101 patients was 62 months (range, 7 to 243 months). At last contact, of the 1,101 patients, 1,004 (91.2%) were alive, 50 (4.5%) had died from RCC, and 47 (4.3%) had died from other causes. Other causes of death included cardiovascular disease, cerebrovascular disease, pulmonary disease, and other malignancies. The cumulative incidence of cancer-specific mortality was 0.4% at 1 year, 2.4% at 3 years, 4.4% at 5 years, and 8.9% at 10 years (Fig. 1). Most of the death from RCC occurred in the first 10 years following curative surgery, whereas the cumulative incidence of death from other causes increased steadily over time.
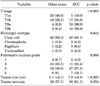
Table 1 lists the characteristics of the patients who died from RCC or other causes. The two groups differed with respect to age at operation, ASA score, and laterality. Patients who died from other causes were older (63.4 years vs. 55.0 years; p<0.001) and had a higher ASA score (26.1% vs. 10.2%; p=0.044) than did those who died from RCC. Table 2 shows the pathologic outcomes according to the cause of death. Pathologic T stage was significantly higher in patients who died from RCC: 56.0% of the patients who died from RCC had a score of pT2a or higher, compared with 14.9% of those who died from other causes (p<0.001). Likewise, a lower nuclear grade, smaller tumor size, and presence of tumor necrosis all favored death from other causes.
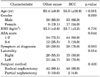
Kaplan-Meier curves demonstrated that other-cause-specific survival differed according to the age at diagnosis, BMI, and ASA score (Fig. 2). The unadjusted Kaplan-Meier estimates of other-cause-specific survival at 5 years was 99.3% for patients aged younger than 50 years, 97.1% for those between 50 and 60 years, 93.2% for those between 60 and 70 years, and 82.8% for those older than 70 years (p<0.001). With regard to BMI, 5 year other-cause-specific survival was 77.6% for patients who were underweight, 96.4% for those with a normal BMI, 99.3% for those who were overweight, and 96.5% for those who were obese (p<0.001). Also, 5 year other-cause-specific survival was 97.8% for patients with an ASA score of l or 2 and 80.1% for those with an ASA score of 3 or higher (p<0.001). Competing risks regression showed that age at diagnosis, BMI, and ASA score were all significantly associated with other-cause-specific death in both univariate and multivariate models (Table 3). Based on the number of risk factors for death from other causes, 5 year other-cause-specific survival was 98.3% (0 risk factors), 84.7% (1 risk factor), and 67.6% (2 or 3 risk factors), respectively (p<0.001) (Fig. 3).
Current options for the management of localized RCC include surgical excision, thermal ablation, and active surveillance. A recent meta-analysis failed to demonstrate a significant difference in metastasis-free survival between treatment options over a mean follow-up of 47.1 months [7]. Not only predicting the behavior of localized RCC but also understanding the individual's competing risks of death is especially important in elderly patients with comorbidities in whom surgery poses significant risks. Thus, we examined the patterns of death among patients with localized RCC. In this study population, 4.5% of the patients died from RCC and 4.3% died from other causes during the follow-up period. Cancer-specific death tended to occur in the first 10 years after curative surgery. Conversely, other causes of death that could be attributed to age or comorbid conditions steadily increased with time. Our data support that when deciding on the treatment plans for localized RCC, patients with old age and comorbidities and their clinicians must weigh the risk of treating localized RCC, which may not affect life expectancy, with the possibility of treating an aggressive RCC early.
Several studies have attempted to quantitate the competing risk of death for patients with RCC. Santos et al. [8] performed a competing risk analysis in 192 patients with clear cell RCC. After a median follow-up of less than 4 years, there were significant differences in overall survival depending on stage and the Charlson comorbidity index. Those authors concluded that patients with localized RCC and a Charlson comorbidity index greater than 2 did not gain a survival benefit from curative surgery. Kutikov et al. [9] reported that 5 year probabilities of kidney cancer death, other cancer death, and non-cancer death were 4%, 7%, and 11% in 30,801 patients with localized, surgically treated RCC from the Surveillance, Epidemiology, and End Results (SEER) database. They identified that age was most predictive of non-kidney cancer deaths, and increasing tumor size was inversely related to non-kidney cancer deaths. They estimated the risk of overall survival or non-kidney cancer death from various parameters including race, gender, tumor size, and age; however, an important limitation of their study was a short follow-up duration and a lack of data on the patients' comorbidities [8,9], which may be one of the important parameters affecting life expectancy [10,11]. We believe that our study has an advantage over previous studies owing to the thorough analysis of the clinical and pathological variables that could help in the choice of a proper treatment method and give more information about prognosis.
Consistent with our study, several studies demonstrated that overweight or obese patients with RCC have a more favorable prognosis than do patients with a low BMI [12-14]. However, the increased risk of death from other causes associated with a low BMI remains to be fully explained. The increased leptin and insulin-like growth factor-1 in obese patients might be associated with increased survival [15]. Also, a low BMI might be an indicator of certain other chronic medical conditions or a low standard of living, which could contribute to conditions such as undernutrition and may increase the risk of premature death [16,17].
This study had some important limitations. The retrospective nature of this study might have biased the subsequent analysis. However, for ethical reasons, it does not seem reasonable to perform a clinical trial of this issue by randomly allocating the patients to active surveillance or surgical treatment. Also, longer follow-up data from this study population would be beneficial. Finally, individuals who did not undergo surgical management were excluded. Although the exact number and indications for surveillance were not available, it is assumed that these patients were poor surgical candidates. Despite the limitations of this study, the usefulness of reviewing the cause of death of this relatively large series of patients with localized RCC is to build a foundation in the literature to support active surveillance for patients with old age or significant comorbidities.
The findings of our study suggest that old age, high ASA score, and low BMI are independent factors predicting death from other causes in patients with localized RCC. Other-cause-specific survival significantly differed on the basis of the number of risk factors for death from other causes. We conclude that the management of localized RCC should be individually based on predicted life expectancy considering these risk factors. Further studies will be required to evaluate the advisability of active surveillance in this patient population.
Figures and Tables
References
1. Chow WH, Devesa SS, Warren JL, Fraumeni JF Jr. Rising incidence of renal cell cancer in the United States. JAMA. 1999. 281:1628–1631.
2. Mues AC, Landman J. Small renal masses: current concepts regarding the natural history and reflections on the American Urological Association guidelines. Curr Opin Urol. 2010. 20:105–110.
3. Chawla SN, Crispen PL, Hanlon AL, Greenberg RE, Chen DY, Uzzo RG. The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J Urol. 2006. 175:425–431.
4. Anuurad E, Shiwaku K, Nogi A, Kitajima K, Enkhmaa B, Shimono K, et al. The new BMI criteria for asians by the regional office for the western pacific region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health. 2003. 45:335–343.
5. Kovacs G, Akhtar M, Beckwith BJ, Bugert P, Cooper CS, Delahunt B, et al. The Heidelberg classification of renal cell tumours. J Pathol. 1997. 183:131–133.
6. Fuhrman SA, Lasky LC, Limas C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol. 1982. 6:655–663.
7. Kunkle DA, Egleston BL, Uzzo RG. Excise, ablate or observe: The small renal mass dilemma- a and review. J Urol. 2008. 179:1227–1233.
8. Santos Arrontes D, Fernández Aceñero MJ, García González JI, Martín Muñoz M, Paniagua Andrés P. Survival analysis of clear cell renal carcinoma according to the Charlson comorbidity index. J Urol. 2008. 179:857–861.
9. Kutikov A, Egleston BL, Wong YN, Uzzo RG. Evaluating overall survival and competing risks of death in patients with localized renal cell carcinoma using a comprehensive nomogram. J Clin Oncol. 2010. 28:311–317.
10. Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK. Five-year survival after surgical treatment for kidney cancer: a population-based competing risk analysis. Cancer. 2007. 109:1763–1768.
11. Gettman MT, Boelter CW, Cheville JC, Zincke H, Bryant SC, Blute ML. Charlson co-morbidity index as a predictor of outcome after surgery for renal cell carcinoma with renal vein, vena cava or right atrium extension. J Urol. 2003. 169:1282–1286.
12. Schrader AJ, Rustemeier J, Rustemeier JC, Timmesfeld N, Varga Z, Hegele A, et al. Overweight is associated with improved cancer-specific survival in patients with organ-confined renal cell carcinoma. J Cancer Res Clin Oncol. 2009. 135:1693–1699.
13. Naya Y, Zenbutsu S, Araki K, Nakamura K, Kobayashi M, Kamijima S, et al. Influence of visceral obesity on oncologic outcome in patients with renal cell carcinoma. Urol Int. 2010. 85:30–36.
14. Jeon HG, Jeong IG, Lee JH, Lee CJ, Kwak C, Kim HH, et al. Prognostic value of body mass index in Korean patients with renal cell carcinoma. J Urol. 2010. 183:448–454.
15. Rasmuson T, Grankvist K, Jacobsen J, Olsson T, Ljungberg B. Serum insulin-like growth factor-1 is an independent predictor of prognosis in patients with renal cell carcinoma. Acta Oncol. 2004. 43:744–748.
16. Lopez-Jimenez F. Speakable and unspeakable facts about BMI and mortality. Lancet. 2009. 373:1055–1056.
17. Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011. 364:719–729.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download