Abstract
Purpose
A single surgeon skilled in conventional laparoscopic surgery used laparoendoscopic single-site surgery (LESS) to treat benign urological diseases. This study reports our surgical results and introduces a simple technique with tips based on our experience.
Materials and Methods
LESS surgery was performed on 116 patients by use of a homemade single-port device composed of an Alexis wound retractor and a powder-free surgical glove. Cases were 44 varicocelectomies (including 8 bilateral cases), 38 renal cyst marsupializations (including 3 bilateral cases), 26 ureterolithotomies (with 1 concomitant ureterolithotomy and contralateral renal cyst marsupialization), 4 prostatic enucleations, and 4 bladder rupture repairs. The mean patient age was 44.43±16.46 years (range, 11 to 76 years), and the male-to-female ratio was 87:29.
Results
In one ureterolithotomy case, LESS was converted to conventional laparoscopic surgery. The mean operative time was 87.03±45.03 minutes, the estimated blood loss was 61.90 ml (range, 0 to 2,000 ml), and the mean hospital stay was 3.03±2.12 days. Two patients underwent single-port transvesical enucleation of the prostate (STEP) requiring patient-controlled anesthesia. No patients developed major complications, and all patients were satisfied, with 75.86% expressing a high degree of satisfaction.
In 2007, Rane et al. and Raman et al. independently reported the first laparoendoscopic single-site surgery (LESS) for transumbilical nephrectomy [1]. Since then, many surgeons have used this technique to treat urological diseases, leading to a number of reports on its usefulness and safety [2]. Most reports of LESS show feasibility, effectiveness, and patient satisfaction for both benign and malignant adrenal, ureter, bladder, prostate, and testis conditions [3]. LESS is suitable for clinical implementation in appropriately selected patients, including normal-weight patients with limited prior abdominal surgery and favorable disease processes [4]. For oncologic surgery, LESS may be recommended only for highly selective conditions when the tumor anatomy is favorable [5]. LESS in pediatric cases and for benign disease has been reported and might be important for cosmetic outcomes [6]. However, commercial port devices have not been available in developing and undeveloped countries. In these countries, the simple technique and tips suggested in our study may be useful. In addition, this might be a chance for beginners to learn the LESS procedure on the model of our experience. The aim of this study was to report our results for LESS in 116 cases of benign urological disease with the introduction of a simple technique for making a homemade single port and several surgical tips for performing LESS.
Between January 2009 and May 2011, a surgeon skilled in conventional laparoscopic surgery used LESS to treat 116 cases of benign urologic disease. The inclusion and exclusion criteria that are used for conventional laparoscopic surgery were applied, resulting in 44 cases of varicocelectomy (8 bilateral), 38 cases of renal cyst marsupialization (3 bilateral), 26 cases of ureterolithotomy (1 with concomitant ureterolithotomy and contralateral renal cyst marsupialization), 4 cases of prostatic enucleation, and 4 cases of bladder rupture repair. In cases of ureterolithotomy, patients who were suspected of having an impacted upper ureter stone or whose prior shock wave lithotrips or ureteroscopy procedure failed to remove their stone were selected. Single-port transvesical enucleation of the prostate (STEP) was conducted on patients who had grade III intravesical prostatic protrusion with a prostatic volume of 80 ml or more via transrectal ultrasound. The mean patient age was 44.43±16.46 years (range, 11 to 76 years), the male-to-female ratio was 87:29, and the mean body mass index was 23.58±2.66 kg/m2.
For all operations, the patient was placed under general anesthesia and a 2 to 4 cm circular incision was made in the lateral side of the umbilicus. A 1-cm extended fascial incision was made and the peritoneum was resected by use of an open technique. The transperitoneal approach was used for surgery. In cases of STEP, a midline incision was made of approximately 3 cm at three finger widths above the symphysis pubis, and an extraperitoneal approach was used. A homemade single-port device was constructed by using an Alexis wound retractor (Applied Medical Resources Co., Rancho, Santa Margarita, CA, USA) and a powder-free surgical glove (Triplex P-free Glove, KM Healthcare, Guri, Korea) (Fig. 1). The wound retractor was inserted into the umbilicus incision site and the upper part of the wound retractor ring was covered with a size 6 or 6½ surgical glove. The surgical glove was folded and inserted to minimize the gap between the abdominal wall and the glove. Three fingers of the glove were cut off and three trocars were inserted and immobilized with 1-0 silk. The three trocars were either one 5-mm and two 12-mm trocars or one 12-mm and two 5-mm trocars. Intraperitoneal CO2 pressure was maintained at 15 mmHg. A 10-mm rigid laparoscope (Stryker, Kalamazoo, MI, USA; Linvatec, Largo, FL, USA) was inserted into the peritoneum through the 12-mm trocar along with the homemade single-port device, and the whole peritoneum, including the area destined for surgery, was examined. Flexible laparoscopic instruments (LaparoAngle, CambridgeEndo, Framingham, MA, USA; Roticulator, Autosuture, Norwalk, CT, USA), were inserted through the remaining trocars and passed into the peritoneal cavity through the single incision port. Surgery was performed by bending the tip of the articular laparoscopic equipment into a shape similar to the basic fifth movement of ballet (Fig. 2A) [7]. In cases in which more instruments were required during surgery, an additional finger of the glove was cut, a trocar was installed as described above, and the required instrument was inserted. In ureterolithotomy, the vertically resected ureter was subjected to continuous suture with 4-0 or 5-0 polyglactin. After completion of the surgery, the skin of the single incision site was sutured with Dermabond (Ethicon Inc., Somerville, NJ, USA).
Both ends of the wound retractor were securely tightened (Fig. 1) and the upper ring was folded three times. A size 6 and 1/2 surgical glove was placed in the upper ring and folded 6 to 7 times to form the shape of the homemade single-port device. The green lower ring was folded. A wound retractor was placed in the transumbilical incision, which was opened by using a Hasson technique.
Interference from the head of the disposable laparoscopic trocar caused problems comparable to the tangling of instruments during LESS (Fig. 2B). To secure sufficient space and to minimize the interference of the trocar head, a gas valve was placed either superiorly or inferiorly.
Articulating or rigid instruments placed in the homemade single-port device could encounter the abdominal wall in the superior region of the lowered wound retractor (Fig. 2C). By placing a telescope in the homemade single-port device, accurate insertion of the instruments was possible. However, this could contaminate the telescope lens. Therefore, we propose confirming the insertion of instruments through the transparent part of the wound retractor by pulling on the homemade single-port device. In particular, this was effective for inserting articulating instruments.
In laparoscopic surgery, the extraction of small samples such as lymph nodes or fat occurs through a trocar. However, in some cases, specimens are easily trapped in the trocar or escape to the peritoneal space. Therefore, we proposed a method for extracting specimens by using another finger of the glove (Fig. 2D). Gas leakage was prevented by clamping with a hemostat after specimen removal.
From January 2009 to May 2011, 116 cases of LESS were performed for benign urological disease. Of these cases using a homemade single-port device, conversion to conventional laparoscopic surgery occurred in only one (0.86%), a ureterolithotomy case (Table 1). The mean operation room times were 52.86±11.73 minutes for varicocelectomy, 92.11±25.31 minutes for renal cyst marsupialization, 118.46±49.04 minutes for ureterolithotomy, 207.50±49.04 minutes for STEP, and 90.00±10.80 minutes for repair of bladder rupture. The mean estimated blood loss for all patients during surgery was 61.90 ml (range, 0 to 2,000 ml). Postoperative surgical complications occurred in 12 cases (10.34%), including Clavien-Dindo grade 1 (10 cases, 8.62%) and 2 (2 cases, 1.72%). Only two patients received transfusions for a decrease in serum hemoglobin levels. Minor postsurgical complications occurred in 10 cases, as specific fever (6 cases, 5.17%) or mild ileus (4 cases, 3.45%). For all 116 patients, the average hospital stay was 3.03±2.12 days. Average hospital stays were 2.23±1.21 days for varicocelectomy, 2.50±0.61 days for renal cyst marsupialization, 3.23±1.80 days for ureterolithotomy, 3.50±0.71 days for STEP, and 7.75±1.71 days for repair of bladder rupture. Two patients underwent STEP with patient-controlled anesthesia after surgery (1.72%). Of the 115 patients in whom LESS surgery was successfully performed, all began oral intake immediately after surgery with a return to routine life in an average of 3.54±1.84 days after surgery. A survey on the level of satisfaction felt by the patients revealed that 88 (75.86%) felt very satisfied and 28 (24.14%) felt somewhat satisfied; thus, all LESS-treated patients expressed satisfaction. The average wound size of the patients 1 month after surgery was 3.06±0.26 cm.
We performed LESS by use of a homemade single-port device in patients with benign urological disease. Conversion to conventional laparoscopic surgery occurred in one ureterolithotomy case. Also, in one case of STEP, bleeding of about 2,000 ml occurred, but we did not convert to conventional laparoscopic surgery because the enucleation was almost finished and the amount of bleeding tends to be exaggerated owing to the inclusion of urine. Surgical outcomes in our study were similar to those in previous reports (Table 1). In particular, Choi et al. [8] reported 100 cases of excellent surgical outcomes of LESS and hybrid LESS in patients with benign urological disease. According to those authors, because of limits from issues such as the specimen extraction method and keeping oncologic principles, the primary treatment of urological cancers such as renal cell carcinoma, upper tract urothelial cell carcinoma, and prostate cancer would be questionable indications. Another study by Choi et al. [6] reported excellent surgical outcomes for 171 cases of LESS in patients with various urologic diseases. They also previously reported initial surgical outcomes of 50 cases of conventional LESS and robotic LESS [9]. Although they performed LESS on more than half of patients with malignant disease, they noted that the ideal indications are pediatric urologic diseases and benign diseases. Currently, when performing oncologic procedures, LESS is recommended only in highly selective situations when the tumor anatomy is favorable [5]. However, feasibility and excellent treatment outcomes with LESS have been reported in patients with malignant disease [10-13]. Further studies are warranted on the indications for LESS.
Initially, the procedures that used LESS were designed to improve the cosmetic outcome of surgery and were aimed to lessen postoperative discomfort [14]. These goals have now been realized. Kaouk et al. [15] reported the surgical outcomes of 1,076 cases of LESS in a worldwide, multi-institutional setting and found surgical outcomes such as skin incision length at closure of 3.5±1.5 cm, mean hospital stay of 3.6±2.7 days, and a visual analogue pain score at discharge of 1.5±1.4. In addition, they reported treating 46% of 1,076 cases by use of LESS with a homemade single-port device. Currently available platforms for single-port surgery include the TriPort (Olympus Co., Tokyo, Japan), SILS Port (Covidien, Norwalk, CT, USA), SSL Access System (Ethicon Inc.), OCTO Port (dalimSurgNET, Seoul, Korea), AirSeal (SurgiQuest Inc., Milford, CT, USA), GelPOINT (Applied Medical Resources Co.), and SPIDER (TransEnterix Inc., Durham, NC, USA) [16]. In countries such as Taiwan and China, however, where LESS is beginning to be performed for patients with urologic disease, no commercial single-port device is available. LESS is therefore performed by use of a homemade single-port device in these countries [10,17,18]. In these cases, as described in this study, a simple technique and tips are useful. In particular, this might be an opportunity for beginners to learn the LESS procedure through the management of cases of benign disease.
Here we described LESS, our technique, and tips for treating patients with benign urological disease. Compared with previous commercial single-port devices, homemade single-port devices composed of a wound retractor and a surgical glove may have some advantages. First, they allow the laparoscope and instruments to be moved relatively freely in a limited operative space. Second, additional surgical instruments can be inserted by cutting off extra fingers from the glove. Third, the elasticity of the surgical glove minimizes the interference of the instruments with the telescope. Fourth, the cost is low compared with that of commercial single-port devices (R-port vs. homemade single-port device; approximately 450 USD vs. 300 USD in Korea) [19]. In our early cases, it took some time to construct the homemade single-port device during surgery. As we have gained experienced with surgical cases, however, we learned tips and techniques that can save time when constructing a single-port device. In beginners performing LESS by use of a homemade single-port device, a surgical glove can be torn by a laparoscopic instrument or a needle, unlike a commercial device [20]. Another disadvantage is that the length to the target organ might be shortened. Particularly in pelvic surgery, the distance from the trocar to the prostate is long [21]. In some cases, the instruments might not reach. Despite these disadvantages, when a commercial device is lacking, attempting LESS by use of a homemade single-port device is worthwhile.
Figures and Tables
FIG. 1
(A) to (E) Homemade single-port device. (A) Both ends of the wound retractor were securely tightened. (B) The white upper ring was folded three times. (C) and (D) One size 6 and 1/2 surgical glove was placed in the upper ring and folded 6 to 7 times. (E) A wound retractor was placed in the transumbilical incision, which was opened by using a Hasson technique.
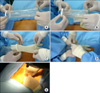
FIG. 2
(A) Surgery was performed by bending the tip of the articular laparoscopic equipment to a shape similar to the basic fifth movement of ballet. (B) To secure the space, a gas valve was placed either superiorly or inferiorly. This minimized interference from the trocar head. (C) Methods for confirming the insertion of instruments through the transparent part of the wound retractor by pulling on a homemade single-port device. (D) Methods of specimen extraction following the cutting of another finger of the glove.

References
1. Autorino R, Cadeddu JA, Desai MM, Gettman M, Gill IS, Kavoussi LR, et al. Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol. 2011. 59:26–45.
2. Autorino R, Stein RJ, Lima E, Damiano R, Khanna R, Haber GP, et al. Current status and future perspectives in laparoendoscopic single-site and natural orifice transluminal endoscopic urological surgery. Int J Urol. 2010. 17:410–431.
3. Symes A, Rane A. Urological applications of single-site laparoscopic surgery. J Minim Access Surg. 2011. 7:90–95.
4. Gettman MT, White WM, Aron M, Autorino R, Averch T, Box G, et al. Where do we really stand with LESS and NOTES? Eur Urol. 2011. 59:231–234.
5. Eisenberg MS, Cadeddu JA, Desai MM. Laparoendoscopic single-site surgery in urology. Curr Opin Urol. 2010. 20:141–147.
6. Choi KH, Ham WS, Rha KH, Lee JW, Jeon HG, Arkoncel FR, et al. Laparoendoscopic single-site surgeries: a single-center experience of 171 consecutive cases. Korean J Urol. 2011. 52:31–38.
7. Lee SW, Lee JY. Laparoendoscopic single-site urological surgery using a homemade single port device: the first 70 cases performed at a single center by one surgeon. J Endourol. 2011. 25:257–264.
8. Choi JD, Kim HS, Ju SH, Lee SY, Han DH, Jeong BC. Initial experience with LESS and hybrid LESS in patients with benign urologic disease. Minim Invasive Ther Allied Technol. 2012. 21:63–70.
9. Jeon HG, Jeong W, Oh CK, Lorenzo EI, Ham WS, Rha KH, et al. Initial experience with 50 laparoendoscopic single site surgeries using a homemade, single port device at a single center. J Urol. 2010. 183:1866–1871.
10. Lin T, Huang J, Han J, Xu K, Huang H, Jiang C, et al. Hybrid laparoscopic endoscopic single-site surgery for radical cystoprostatectomy and orthotopic ileal neobladder: an initial experience of 12 cases. J Endourol. 2011. 25:57–63.
11. White MA, Haber GP, Autorino R, Khanna R, Forest S, Yang B, et al. Robotic laparoendoscopic single-site radical prostatectomy: technique and early outcomes. Eur Urol. 2010. 58:544–550.
12. Lee JY, Kim SJ, Moon HS, Kim YT, Lee TY, Park SY. Initial experience of laparoendoscopic single-site nephroureterectomy with bladder cuff excision for upper urinary tract urothelial carcinoma performed by a single surgeon. J Endourol. 2011. 25:1763–1768.
13. Kaouk JH, Goel RK, Haber GP, Crouzet S, Desai MM, Gill IS. Single-port laparoscopic radical prostatectomy. Urology. 2008. 72:1190–1193.
14. Raybourn JH 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010. 75:100–103.
15. Kaouk JH, Autorino R, Kim FJ, Han DH, Lee SW, Yinghao S, et al. Laparoendoscopic single-site surgery in urology: Worldwide multi-institutional analysis of 1076 cases. Eur Urol. 2011. 60:998–1005.
16. Autorino R, Kim FJ, Rane A, De Sio M, Stein RJ, Damiano R, et al. Low-cost reusable instrumentation for laparoendoscopic single-site nephrectomy: assessment in a porcine model. J Endourol. 2011. 25:419–424.
17. Tai HC, Lin CD, Wu CC, Tsai YC, Yang SS. Homemade transumbilical port: an alternative access for laparoendoscopic single-site surgery (LESS). Surg Endosc. 2010. 24:705–708.
18. Lee JY, Lee SW. Laparoendoscopic single-site renal cyst marsupialization using a homemade single-port device has a role as a feasible treatment option. Urol Int. 2011. 87:309–313.
19. Lee SY, Kim YT, Park HY, Lee TY, Park SY. Initial experience with laparoendoscopic single-site surgery by use of a homemade transumbilical port in urology. Korean J Urol. 2010. 51:613–618.
20. Lee JY, Han JH, Kim TH, Yoo TK, Park SY, Lee SW. Laparoendoscopic single-site ureterolithotomy for upper ureteral stone disease: the first 30 cases in a multicenter study. J Endourol. 2011. 25:1293–1298.
21. Lee JY, Ha US, Lee SW. Initial experience of laparoendoscopic single-site radical prostatectomy requiring well-equipped appliances and a skilled technique. Case Rep Oncol. 2010. 3:445–450.
22. Park SW, Kim TN, Lee W, Park HJ, Lee SD, Park NC. Umbilical laparoendoscopic single site surgery versus inguinal varicocelectomy for bilateral varicocele: a comparative study. Int J Urol. 2011. 18:250–254.
23. Kaouk JH, Palmer JS. Single-port laparoscopic surgery: initial experience in children for varicocelectomy. BJU Int. 2008. 102:97–99.
24. Micali S, Isgrò G, Stefani SD, Pini G, Sighinolfi M, Bianchi G. Retroperitoneal laparoendoscopic single-site surgery: Preliminary experience in kidney and ureteral indications. Eur Urol. 2011. 59:164–167.
25. Ryu DS, Park WJ, Oh TH. Retroperitoneal laparoendoscopic single-site surgery in urology: initial experience. J Endourol. 2009. 23:1857–1862.
26. Rané A, Rao P. Single-port-access nephrectomy and other laparoscopic urologic procedures using a novel laparoscopic port (R-port). Urology. 2008. 72:260–263.
27. White WM, Haber GP, Goel RK, Crouzet S, Stein RJ, Kaouk JH. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009. 74:801–804.
28. Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, et al. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009. 74:805–812.
29. Desai MM, Fareed K, Berger AK, Astigueta JC, Irwin BH, Aron M, et al. Single-port transvesical enucleation of the prostate: a clinical report of 34 cases. BJU Int. 2010. 105:1296–1300.
30. Oh JJ, Park DS. Novel surgical technique for obstructive benign prostatic hyperplasia: finger-assisted, single-port transvesical enucleation of the prostate. J Endourol. 2011. 25:459–464.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download