Abstract
Xanthogranulomatous cystitis is a rare, benign chronic inflammatory disease of unknown etiology. Herein we report a case of a 41-year-old man who presented with painless hematuria and a bladder mass on imaging studies.
Xanthogranulomatous cystitis (XC) is a rare, benign chronic inflammatory disease of unclear etiology that was first described in 1932 [1]. Xanthogranulomatous changes have been reported to occur in many sites, including the colon, ovary, pancreas, salivary gland, appendix, gall bladder, endometrium, brain, and kidney [2]. To the best of our knowledge, about 30 cases have been reported in the literature and only 5 cases have been reported in the Korean literature [3-5]. Herein we describe the 6th case of XC to be reported in Korea.
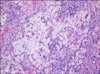
A 41 year-old male presented with a 3 month history of painless hematuria. He had no significant past medical history. The results of a physical examination were normal. Laboratory studies revealed a normal hematological and biochemical profile. Urinalysis showed many red blood cells and plenty of white blood cells per high power field. Urine culture grew Escherichia coli and urine cytology revealed no malignant cells. Ultrasonography showed a protruding mass lesion (1.5 cm) in the left posterobasal area of the bladder (Fig. 1). Contrast-enhanced computed tomography demonstrated no invasion of the bladder muscle or surrounding organ. Excretory urography showed a normal upper urinary tract. Cystoscopy revealed a sessile protruded mass with petechia (Fig. 2). Complete endoscopic resection was done. Biopsy of the sessile mass revealed histological findings suggestive of XC characterized by foamy histiocytes and lymphocytes (Fig. 3). The postoperative course was uneventful. The patient remains asymptomatic with no recurrence of symptoms 3 months after surgery.
XC is an extremely rare, affirmative chronic inflammatory disorder throughout the world, and approximately 30 cases have been reported since the first report in 1932 by Wassiljew [1]. Most of these cases were associated with a urachal remnant or urachal adenoma [6], whereas the remaining cases either had association with or did not have any association with anaerobic bacterial infection [7], malignant bladder tumor [8], and suture materials [3].
However, nothing about the disease has been clearly and definitively defined to date. Regarding its origin, various theories have been presented, including immune abnormality, abnormal lipid metabolism, and reduction of chemotaxis activity and chronic urothelial dysplasia due to chronic infection [9]. In addition, although race and epidemiological association or lifestyle are suspected to be related on the basis of the finding that most of the cases were reported in Japan, China, and Korea, many more cases and more research on this aspect are necessary to confirm this [4].
Most of the reported cases were localized mainly at the dome of the bladder or near the dome [2]. However, in the present case, the mass was on the posterobasal wall of the bladder, which indicated an absence of relation with the urachus. Although the details of the etiology of the present case are unclear, it appears that XC may be associated with some chronic infection without a urachal remnant or urachal adenoma.
The symptoms of XC are nonspecific and difficult to distinguish from other disorders of the bladder. Therefore, diagnosis is very difficult without tissue biopsy or without examining the tissues obtained from surgery [9]. Even in the cases that we have examined, we suspected bladder tumor before the surgery but were able to diagnose the mass as XC when we discovered xanthoma cells with foamy cytoplasm with numerous infiltrations of inflammatory cells and an abundance of lipids in the tissue biopsy following the surgery.
Figures and Tables
References
1. Wassilijew AI. Uber Erkrankungen des urachus. Z Urol Chir. 1932. 35:199–212.
2. Hayashi N, Wada T, Kiyota H, Ueda M, Oishi Y. Xanthogranulomatous cystitis. Int J Urol. 2003. 10:498–500.
3. Chung MK, Seol MY, Cho WY, Seo HK, Kim JS. Xanthograulomatous cystitis associated with suture material. J Urol. 1998. 159:981–982.
4. Jeong WI, Lee KG, Han KH, Lee SC, Kim YT, Kim WJ. Xanthogranulomatous cystitis. Korean J Urol. 2002. 43:180–182.
5. Han DH, Choi HJ, Kim JH, Shin JS, Chung KJ, Choi HY, et al. Xanthogranulomatous cystitis. Korean J Urol. 2004. 45:958–961.
6. Walther M, Glenn JF, Vellios F. Xanthogranulomatous cystitis. J Urol. 1985. 134:745–746.
7. Tai HL, Chen CC, Yeh KT. Xanthogranulomatous cystitis associated with anaerobic bacterial infection. J Urol. 1999. 162:795–796.
8. Bates AW, Fegan AW, Baithun SI. Xanthogranulomatous cystitis associated with malignant neoplasms of the bladder. Histopathology. 1998. 33:212–215.
9. Tan LB, Chiang CP, Huang CH, Chian CH. Xanthogranulomatous cystitis: A case report and review of the literature. Int Urol Nephrol. 1994. 26:413–417.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download