Abstract
Purpose
To investigate the impact of menopause on the quality of life (QoL) of middle-aged and older women, including their general well-being, voiding-related symptoms, and sexual distress.
Materials and Methods
To assess QoL, we administered a questionnaire that included questions about voiding-related symptoms and female sexual distress and part of the Women's Health Questionnaire. The self-administered questionnaires were completed by 1,679 women in the Korea. Data for 1,262 women were available for analysis, including premenopausal (n=307), perimenopausal (n=240), and postmenopausal (n=715) groups.
Results
Voiding-related discomfort increased significantly in perimenopausal and postmenopausal women compared with premenopausal women (p<0.001). General well-being worsened as menopause progressed (p<0.001). Menopausal women who were older (p=0.014), had a hysterectomy (p=0.005), or had urinary incontinence (p=0.001) had more voiding-related symptoms. Hypertension (p=0.026), cardiac disease (p=0.013), and arthritis (p=0.001) resulted in significantly decreased general well-being. Women with a hysterectomy (p=0.017) and those with arthritis (p=0.004) had high sexual distress. In the menopausal group, employed women had better general well-being than did unemployed women.
Conclusions
Menopause negatively affected the QoL of middle-aged and older women because of decreased general well-being and increased voiding-related symptoms. General health, even in menopausal women, was important to maintain a better QoL. To preserve the QoL of women undergoing menopause, control of menopause and underlying disease should be considered.
As people are living longer with advances in science, medicine, and economic status, interest has transitioned from simply increasing longevity to improving the quality of life (QoL). Middle-aged and older women undergoing menopause experience lifestyle changes. A postmenopausal woman with an erratic decline in ovarian steroid hormones, especially estrogen and progesterone, experiences symptoms such as an irregular menstrual cycle, hot flashes, sleep disturbance, mood swings, voiding-related symptoms, and changes in sexual function. In the past, when life expectancy was less than 60 years, life after menopause was considered a blessing and postmenopausal symptoms were not considered seriously.
Gracia et al reported that numerous factors play roles in the sexual dysfunction encountered after menopause, including the absence of a partner, high anxiety, children living at home, and pain [1]. A low dehydroepiandrosterone sulfate (DHEAS) level was reported to correlate well with sexual dysfunction. Declining estrogen levels also contribute to changes in the lower urinary tract. For example, the urinary bladder and urethra may produce symptoms related to stress incontinence, urinary urgency, and frequency. Deterioration in the vaginal and periurethral tissue is called vaginal atrophy and decreased estrogen is the primary cause. From a psychiatric perspective, affected women are susceptible to decreased libido, depression, low back pain, and memory loss compared with their healthy counterparts, and they subsequently experience deteriorating health and a poor QoL.
Although many studies have examined the decline in physical and mental functions among postmenopausal women, few studies have reported on their overall QoL, including lower urinary tract symptoms and sexual distress, as menopause progresses. Few studies have reported objective data for the effects of menopause on changes in urinary habits, sexual stress, and general well-being, which led us to accumulate these important data on patient care in Korea.
This study investigated the effects of menopause on QoL, including general well-being, voiding-related symptoms, and sexual distress, and the correlations among these factors.
The study subjects were 1,679 women aged 40 to 65 years in the general population. To avoid selecting patients with specific symptoms, we recruited lay people, including 816 in Busan and Gyeongsangnam-do, 561 in Seoul and Gyeonggi-do, and 302 in Daegu and Gyeongsangnam-do.
After giving informed consent, the subjects completed a questionnaire. After excluding subjects who did not fall into the target age range (40 to 65 years old) or did not answer every question, 1,262 subjects remained for analysis.
The subjects were categorized into premenopausal, perimenopausal, and postmenopausal groups. Perimenopause was defined as the state in which a woman had irregular periods or no periods in the past year. Postmenopause was defined as post-oophorectomy or the absence of menstruation for more than 1 year.
The questionnaire comprised 30 subsets, including personal information, voiding-related symptoms, general well-being, and sexual distress. The personal information included questions on age, occupation, history of hysterectomy, menstrual status, and medical conditions, including diabetes mellitus (DM), hypertension (HTN), obesity, dyslipidemia, cancer, urinary incontinence, and arthritis. The subset of questions on voiding-related symptoms used five of the nine questions from the Korean version of the benign prostatic hypertrophy QoL questionnaire, an instrument developed by the Korean Urology Association in 2001 to evaluate the QoL of patients with lower urinary tract symptoms [2]. Scores ranged from 1 to 6, with higher scores indicating worse voiding-related symptoms. To evaluate general well-being, we translated into Korean and validated 15 questions (scored 1-4) from the Woman's Health Questionnaire developed by Hunter et al to evaluate the physical and psychological symptoms of peri- or postmenopausal patients [3]. Lower summed scores indicated worse QoL. To obtain information about sexual function, we used the female sexual distress scale (FSDS) developed by Derogatis et al to assess the degree of stress associated with sexual life in the most recent 2 weeks [4]. For simplicity, we used five of the 12 questions after confirming their validity in Korean. Scores ranged from 1 to 5, with higher scores indicating greater stress.
SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Student's t-test and ANOVA were used to analyze the voiding-related symptoms, general well-being, and sexual distress according to menopausal status and the severity of the voiding-related symptoms, general well-being, and sexual distress according to the employment status of the postmenopausal women. The association of voiding-related symptoms, general well-being, and sexual distress with chronic disease in the postmenopausal women was assessed by using a linear regression model. We used the risk ratio with a 95% confidence interval (CI) to evaluate the association between chronic disease and voiding-related symptoms, general well-being, and sexual distress. Beta is reported with the accompanying 95% CI. Results were considered statistically significant when p<0.05.
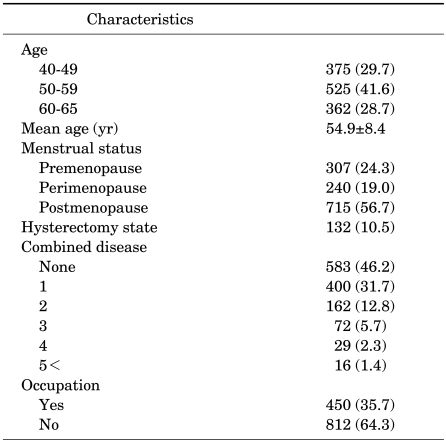
The subjects included 375 (29.7%), 525 (41.6%), and 362 (28.7%) women in their 40s, 50s, and 60s, respectively, with an average age of 54.9±8.4 years. According to menstrual status, the sample included 307 (24.3%), 240 (19%), and 715 (56.7%) pre-, peri-, and postmenopausal women with average ages of 46.9±5.0, 50.7±4.7, and 59.8±7.0 years, respectively. The sample included 583 (46.2%) subjects with no underlying medical condition, 400 (31.7%) subjects with one disease, 162 (12.8%) with two diseases, 72 (5.7%) with three diseases, 29 (2.3%) with four diseases, and 16 (1.4%) subjects with five or more diseases. In addition, 450 (35.7%) subjects were employed and 812 (64.3%) were not (Table 1).
A significant difference (ANOVA, p<0.001) was observed among the average scores for voiding-related symptoms in the pre- (8.1±4.2), peri- (10.1±3.9), and postmenopausal (11.7±5.0) groups (Table 2).
Total scores were 32.4±6.8, 39.1±5.4, and 37.1±6.5 in the pre-, peri-, and postmenopausal groups, respectively, confirming the decrease in general well-being as menopause progresses (ANOVA, p<0.001) (Table 2).
The average score for sexual distress tended to increase from 10.9±3.7 to 11.5±4.0 to 12.7±4.4 in the pre-, peri-, and postmenopausal groups, respectively (ANOVA, p=0.318) (Table 2), although the differences were not significant.
Among women aged 40 to 44, 45 to 49, and over 50 years in the premenopausal group, no statistical significance was demonstrated in voiding-related symptoms (p=0.614) or general well-being (p=0.555). Among women in the postmenopausal group aged under 50, 50 to 59, and over 60 years, statistical significance was demonstrated for voiding- related symptoms (p=0.009) and general well-being (p=0.015).
The number of premenopausal, perimenopausal, and postmenopausal women aged 50 to 55 years was 61,104, and 170, respectively. Among women in these groups, the statistical significances in the parameters of voiding-related symptoms and general well-being were p=0.000 and p=0.020, respectively.
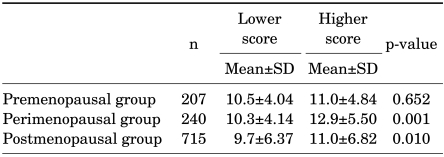
The menopausal groups were subdivided into two groups on the basis of the average scores for questions in the sexual domain (15-30 vs. 5-14). The higher subgroup had a significantly higher score in the urinary domain than did the lower subgroup (11.0±6.82 vs. 9.7±6.37, p=0.010). In the premenopausal group, no correlation was found between the subgroups with high and low scores (11.0±4.84 vs. 10.5±4.04, p=0.652). In contrast, a significant difference was observed between the high- and low-scoring perimenopausal subgroups (12.9±5.50 vs. 10.3±4.14, p=0.001) (Table 3).
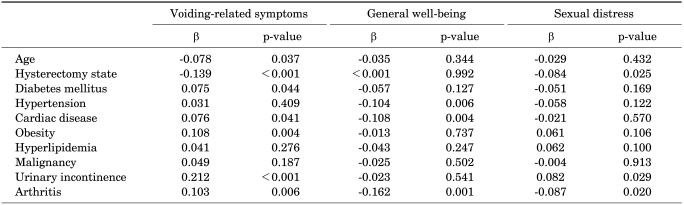
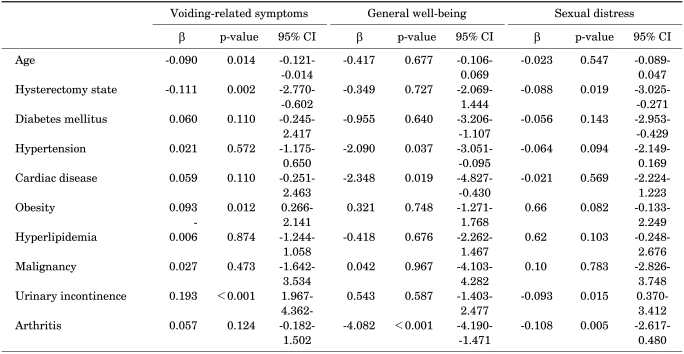
We found significant correlations between voiding-related symptoms and old age (p=0.037), a previous hysterectomy (p<0.001), cardiac disease (p=0.041), obesity (p=0.004), urinary incontinence (p<0.001), and arthritis (p=0.006). Multivariate analysis showed correlations with age (p=0.014, 95% CI: -0.121, -0.014), a previous hysterectomy (p=0.002, 95% CI: -2.770, -0.602), obesity (p=0.012, 95% CI: 0.266, 2.141), and urinary incontinence (p<0.001, 95% CI: 1.967, 4.362). General well-being was correlated with HTN (p=0.006), cardiac disease (p=0.004), and arthritis (p<0.001). In the multivariate analysis, HTN (p=0.037, 95% CI: -3.206, 1.107), cardiac disease (p=0.019, 95% CI: -4.827, -0.430), and arthritis (p<0.001, 95% CI: -4.190, -1.471) were all correlated. Sexual distress was related to a previous hysterectomy (p=0.025), urinary incontinence (p=0.029), and arthritis (p=0.020); the multivariate analysis showed correlations with previous hysterectomy (p=0.019, 95% CI: -3.025, -0.271), urinary incontinence (p=0.015, 95% CI: 0.370, 3.412), and arthritis (p=0.005, 95% CI: -2.617, -0.480) (Tables 4, 5).
Despite having gone through menopause, women who were employed had a higher QoL score than did those who were unemployed (36.1±6.46 vs. 37.6±6.52, p=0.001). Sexual distress (11.1±4.80 vs. 9.96±6.93, p=0.084) and voiding-related symptoms (11.5±5.0 vs. 12.17±5.35, p=0.162) (Fig. 1) were not correlated with employment status.
This study examined postmenopausal symptoms in middle-aged women in Korea to prepare for the aging of society by understanding the effects of menopause on QoL, especially in terms of voiding-related symptoms, sexual function, and general well-being. The subjects were divided into pre-, peri-, and postmenopausal groups and were administered a questionnaire to evaluate the impact of the progression of menopause. We restricted the study subjects to the age range of 40 to 65 years to minimize the influence of age. Obviously, the average age in the three groups differed (p<0.001), implying that the effect of menopause on the QoL of middle-aged women is closely related to the physical aging process.
Voiding difficulty worsened as the women went through menopause. Scores for three questions about lower urinary tract symptoms and the two about physical conditions increased with the progression through menopause. Physiologically, estrogen receptors are present in the proximal and distal urethra, vagina, and trigonal epithelium of the urinary bladder. The lack of estrogen after menopause can cause dysfunction of bladder contraction and urethral closure by affecting the circulation to the urethra, which decreases pressure and contributes to incontinence [5-7]. In addition, estrogen would relieve voiding-related symptoms, including urgency, frequency, and urge incontinence [8].
The questionnaire on general well-being included questions about depressive mood (3), vasomotor symptoms (3), attractiveness (1), somatic symptoms (4), memory and concentration (1), and sexual behavior (3). Responses to these questions showed that the QoL decreased as menopause progressed. This decline is thought to be secondary to the physical and psychological changes due to the reduction in hormones after menopause. As Freeman's study indicated, depressive symptoms worsen as women enter the perimenopausal period. Significant predictors of depressive symptoms include a history of depression, severe premenstrual syndrome, poor sleep, age, race, and employment status [9].
The original FSDS questionnaire comprised 20 questions, of which 16 dealt with single factors, such as dissatisfaction, anger, concern, and disappointment. Others measured different aspects, such as a bad sexual relationship and anxiety regarding sexual performance. We used one question each about sexual performance, stress, dissatisfaction, anger, and loss of sexual attraction, but did not include sexual performance, because it does not seem to be a good measure of whether sexual problems exist [5]. When we included all of these measures, sexual stress did not seem to be influenced by menopause. However, the questionnaire on general well-being suggested that physical sexual activity contributed to general well-being in the pre-, peri-, and postmenopausal groups (ANOVA, p<0.001).
Because these groups were composed of women of different ages, age could have affected the parameters as well as menopause. Therefore, we tried to verify the statistical significance of the parameters affected by menopause, not by age. We subanalyzed the statistical significance in voiding-related symptoms and general well-being in the premenopausal and postmenopausal groups according to age, which showed statistical significance except for sexual distress. We also analyzed the parameters among premenopausal, perimenopausal, and postmenopausal women aged 50 to 55 years. This analysis demonstrated statistical significance in the parameters of voiding-related symptoms and general well-being. These 3 subanalyses supported the finding that menopause rather than age significantly affected voiding-related symptoms and general well-being, although age was one of the factors to more adversely affect voiding-related symptoms in the older aged group.
We postulate that although physical discomfort may be worse, a decrease in sexual desire may contribute to reduced psychological stress. In addition, one should consider cultural factors when interpreting sexually related matters. In a study of women who had surgically induced menopause and lacked ovarian hormones, Graziottin et al found that 35% to 44% of the women had disordered sexual desire [10,11]. Up to 87% of elderly women have been reported to complain of sexual dissatisfaction [12]. In attempts to treat sexual desire disorder, testosterone and estrogen replacement are effective in the short term for disorders of desire, arousal, and orgasm; vaginal estrogen tablets to correct the physical component might be effective in treating symptoms due to vaginal atrophy, the pH of the vagina, and the vaginal maturation index [13,14].
Voiding-related symptoms were prominent in menopausal women who were older, had a previous hysterectomy, were obese, and had urinary incontinence. As mentioned, the physical aging process is associated with voiding-related symptoms, and the loss of bladder support secondary to a hysterectomy can contribute to such symptoms. A recent study found a correlation between DM and voiding-related symptoms, although the correlation was not significant, perhaps because the study did not examine the severity or duration of DM. The general-well being was worse in patients with HTN, cardiac disease, and arthritis; physical restrictions, rather than DM, obesity, or dyslipidemia, may contribute to the QoL [15]. Patients with a disorder of the genital tract, such as a hysterectomy or connective-tissue disorder, may have limited movement of the large joints during intercourse that restricts the positions they can assume and may have a negative body image, all of which might negatively affect their sexual life [16]. As with the results for voiding-related symptoms, DM was not correlated with sexual distress in this study.
In the menopausal group, employed women expressed greater satisfaction in the assessment of QoL, but sexual distress was not affected by employment. Our results differed from those of previous studies. In a Turkish study, employed women of all ages had low sexual dysfunction. Moreover, the Turkish subjects in the same age range as examined in our study showed a low prevalence of sexual dysfunction [17]. This discrepancy might be explained by a cultural difference in terms of whether women consider reduced sexual desire a problem. In the menopausal group, employment did not contribute to voiding-related symptoms. The EPIC study, which compared subjects with overactive bladders to those without symptoms, found a significant difference in the effect of employment [18]. In contrast, employment in Korean women had no effect on lower urinary tract symptoms, although patients with voiding-related problems may need these to be corrected because they could reduce performance and productivity at work.
Our subdivision of menopausal women into high- and low-scoring subgroups for voiding-related symptoms revealed that worse voiding-related symptoms were associated with greater sexual dysfunction. The dysfunction was related more to the combination of an overactive bladder with voiding-related symptoms, rather than an overactive bladder alone or an overactive bladder with urge incontinence alone. An improvement in voiding-related symptoms might correct the sexual dysfunction experienced by menopausal women.
There are several limitations to this study. First, we would have preferred to recruit subjects nationwide but were limited to recruiting subjects from a few metropolitan areas. Consequently, we cannot exclude the possibility that socioeconomic and educational backgrounds might have affected the results. In addition, the use of a questionnaire, rather than in-depth interviews, to collect data might have affected the validity of our study.
Menopause in Korean females has a negative impact on voiding-related symptoms and general well-being but not on sexual distress. Nevertheless, in the menopausal group, worsening voiding-related symptoms strongly affected sexual distress. Underlying medical conditions can decrease QoL. In general, employed subjects, even menopausal women, had better well-being. In conclusion, it might be necessary to control physical symptoms, treat underlying medical conditions, and encourage subjects to take an active attitude toward life to improve the QoL of middle-aged women.
References
1. Gracia CR, Freeman EW, Sammel MD, Lin H, Mogul M. Hormones and sexuality during transition to menopause. Obstet Gynecol. 2007; 109:831–840. PMID: 17400843.

2. Hong JE, Choi HY, Hong SJ, Chung MK, Ahn TY, Rim JS, et al. Construction of a short form BPH specific health related quality of life scale: reliablility and validity tests. Korean J Urol. 2001; 42:1270–1277.
3. Lee KY, Park TJ. The quality of life in the menopausal women. J Korean Acad Fam Med. 1999; 20:894–905.
4. Han C, Kim HC, Kang SH, Moon DG, Kim JJ, Choi JY. Validity and reliability of Korean version of the female sexual distress scale (FSDS). Korean J Androl. 2004; 22:68–74.
5. Blakeman PJ, Hilton P, Bulmer JN. Oestrogen and progesterone receptor expression in the female lower urinary tract, with reference to oestrogen status. BJU Int. 2000; 86:32–38. PMID: 10886079.

6. Shenfeld OZ, McCammon KA, Blackmore PF, Ratz PH. Rapid effects of estrogen and progesterone on tone and spontaneous rhythmic contractions of the rabbit bladder. Urol Res. 1999; 27:386–392. PMID: 10550529.

7. Rud T. The effects of estrogens and gestagens on the urethral pressure profile in urinary continent and stress incontinent women. Acta Obstet Gynecol Scand. 1980; 59:265–270. PMID: 7191614.

8. Sultana CJ, Walters MD. Estrogen and urinary incontinence in women. Maturitas. 1994; 20:129–138. PMID: 7715464.

9. Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry. 2004; 61:62–70. PMID: 14706945.
10. Graziottin A, Koochaki PE, Rodenberg CA, Dennerstein L. The prevalence of hypoactive sexual desire disorder in surgically menopausal women: An epidemiological study of women in four European countries. J Sex Med. 2009; 6:2143–2153. PMID: 19453880.

11. Shifren JL, Braunstein GD, Simon JA, Casson PR, Buster JE, Redmond GP, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000; 343:682–688. PMID: 10974131.

12. Azadzoi KM, Siroky MB. Neurologic factors in female sexual function and dysfunction. Korean J Urol. 2010; 51:443–449. PMID: 20664775.

13. Sherwin BB, Gelfand MM. The role of androgen in the maintenance of sexual functioning in oophorectomized women. Psychosom Med. 1987; 49:397–409. PMID: 3615768.

14. Kim M, Choi H. Changes in atrophic symptoms, the vaginal maturation index, and vaginal pH in postmenopausal women treated with vaginal estrogen tablets. J Korean Soc Menopause. 2010; 16:162–169.
15. Ho MH, Yip S, Bhatia NN. Lower urinary tract dysfunctions in women with diabetes mellitus. Curr Opin Obstet Gynecol. 2007; 19:469–473. PMID: 17885464.

16. Josefsson KA, Gard G. Women's experiences of sexual health when living with rheumatoid arthritis- an explorative qualitative study. BMC Musculoskelet Disord. 2010; 11:240. PMID: 20950461.

17. Cayan S, Akbay E, Bozlu M, Canpolat B, Acar D, Ulusoy E. The prevalence of female sexual dysfunction and potential risk factors that may impair sexual function in Turkish women. Urol Int. 2004; 72:52–57. PMID: 14730166.

18. Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008; 101:1388–1395. PMID: 18454794.

FIG. 1
Symptom severity of voiding-related symptoms, general well-being, and sexual distress according to the employment state in the group of postmenopausal women (ap<0.05). QoL: quality of life.
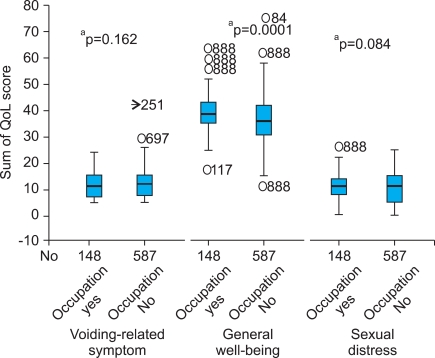
TABLE 2
ANOVA of voiding-related symptoms, general well-being, and sexual distress according to menstrual state
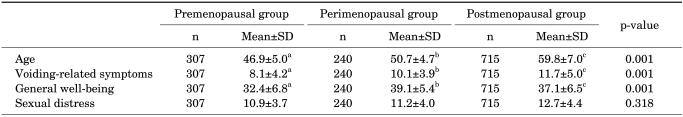
TABLE 3
Correlation between voiding-related symptoms and sexual distress according to menstrual state




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download