Abstract
Purpose
To report our initial clinical experience and perioperative outcomes of retroperitoneal laparoendoscopic single-site surgery (RLESS) for upper urinary tract surgery.
Materials and Methods
Between June 2009 and October 2010, we performed RLESS in 23 patients for various indications including radical nephrectomy (n=4), nephroureterectomy (n=2), simple nephrectomy (n=10), and renal cyst ablation (n=7). RLESS was performed with a homemade single-port device with a conventional rigid laparoscopic instrument and laparoscope. The parameters analyzed were age, body mass index, operative time, estimated blood loss, transfusion, time of oral intake, visual analogue pain scale score (VAPS), length of hospital stay, and complications.
Results
One case of simple nephrectomy was converted to open nephrectomy because of severe adhesion and inadequate surgical exposure. RLESS was completed in 23 patients. Mean operative time was 168.7±29.2, 227.5±50.0, 230.0±56.5, and 70.5±8.9 minutes for simple nephrectomy, radical nephrectomy, nephroureterectomy, and renal cyst ablation, respectively. Estimated blood loss was 113.0±149.8, 170.0±156.8, 400.0±141.4, and 22.8±16.0 ml. The time to oral intake after surgery was 1.4±0.5, 1.2±0.5, 1.5±0.7, and 1.1±0.3 days. The mean VAPS score was 1.1±0.2, 2.1±0.5, 2.0±0.5, and 1.0±0.0 of 10 (range, 0.8 to 2.6). The hospital stay was 4.6±1.5, 3.7±0.5, 6.0±1.4, and 3.2±1.7 days. No major perioperative complications were observed.
Transperitoneal and retroperitoneal laparoscopic urologic surgeries have proven to be safe and effective compared with open surgery, offering the benefits of decreased blood loss, less postoperative pain, shorter hospital stay, rapid convalescence, and improved cosmetic effect. Recently, laparoscopic surgery using new technology and surgical techniques has maximized the cosmetic effect by reducing the number of trocars, which has led to efforts to reduce the complications caused by trocars. Laparoendoscopic single- site surgery (LESS), a technique that developed as an extension of conventional laparoscopic surgery with the insertion of a single port, multiple ports, or a single multi-port platform through a single incision or location, is currently receiving the spotlight [1-3].
Since the first LESS nephrectomy reported in the urologic literature by Rané et al in 2007 [4], increasing experience and the proven safety and feasibility of LESS have allowed the expansion of indications to include complex reconstructive procedures such as pyeloplasty, partial nephrectomy, ureterolithotomy, radical prostatectomy, and radical cystectomy [1-3,5-9]. However, the majority of cases reported to date have been transperitoneal procedures for the various urologic diseases [10].
The retroperitoneal approach has some advantages compared with the transperitoneal approach, which allows more direct access to the kidney and renal hilum and has the merits of rare retraction of internal organs and less risk of peritoneal contamination by spillage of urinary contents such as urine, tumor, or abscess [11].
Two institutions reported the first retroperitoneal LESS surgery in urology in 2009 [12,13]. Since then, a limited number of authors have reported retroperitoneal LESS because of the long learning curve and technical difficulties [14 - 17].
The aim of this study was to evaluate the technical feasibility and safety of retroperitoneal laparoendoscopic single- site surgery (RLESS) and the clinical effects of 23 cases of RLESS in our hospital.
Between June 2009 and October 2010, we performed RLESS in 23 patients for various indications including simple nephrectomy (n=10), radical nephrectomy (n=4), nephroureterectomy (n=2), and renal cyst ablation (n=7). All surgeries were performed by one surgeon. The patient was placed in the full flank position, and an approximately 3 to 4 cm transverse single incision was made beneath the tip of the 12th rib. The retroperitoneal space was developed with blunt finger dissection, and a balloon dilator was placed into the retroperitoneal space and inflated with 800 ml of air. An Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) was inserted into the retroperitoneal space through a single incision. A homemade single-port device consisted of an Alexis wound retractor and a surgical glove. The ends of three fingers of a no.7 surgical glove were cut, one 5 mm trocar and two 11 mm trocars were fixed with silk tie in the finger joint of the surgical glove, and the wrist of the glove was put in the outer ring of the wound retractor (Fig. 1). After insertion of the homemade single-port device and retroperitoneal insufflation with CO2 to 12 mmHg, conventional laparoscopic instruments and a 30 degree, 10 mm rigid laparoscope were inserted. The RLESS procedures were performed according to techniques used in conventional retroperitoneal laparoscopy by the types of surgery.
Small specimens were retrieved through the 10 mm port without port removal. Large benign specimens were removed after the specimen in the entrapment bag was fragmented by use of scissors without extension of the incision at the end of procedure. For radical nephrectomy, the specimens were extracted via extension of the original incision or via an additional Gibson incision according to oncological principles. For nephroureterectomy, a modified Gibson incision was made to pull out the dissected kidney and ureter and then a distal ureterectomy with bladder cuff excision was performed through the modified Gibson incision to remove the specimen en bloc.
To analyze the patient group, we examined age, disease, body mass index (BMI), the operative time, estimated blood loss, transfusion, the time to oral intake after surgery, pain intensity, length of hospital stay, and complications. The pain intensity was measured by using a self-report pain intensity scale (Visual Analogue Pain Scale, VAPS) for three days after surgery. Patients were followed up postoperatively for evidence of adverse events.
A total of 23 of 24 cases were completed without insertion of the subsidiary port or open conversion. One case of simple nephrectomy was converted to open surgery because of severe adhesion and inadequate surgical exposure.
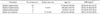
The average age of the patients who underwent RLESS was 56.8±14.4 years (range, 23 to 82 years), and the mean BMI was 23.3±2.7 kg/m2 (range, 16.1 to 27.2 kg/m2) (Table 1). The mean operative time of RLESS simple nephrectomy, radical nephrectomy, nephroureterectomy, and renal cyst ablation was 168.7±29.2, 227.5±50.0, 230.0±56.5, and 70.5±8.9 minutes, respectively. The estimated blood loss during the operation was 113.0±149.8, 170.0±156.8, 400.0±141.4, and 22.8±16.0 ml. The time of oral intake after surgery was 1.4±0.5, 1.2±0.5, 1.5±0.7, and 1.1±0.3 days. The mean VAPS score was 1.1±0.2, 2.1±0.5, 2.0±0.5, and 1.0±0.0 out of 10 (range, 0.8 to 2.6), and the mean hospital stay was 4.6±1.5, 3.7±0.5, 6.0±1.4, and 3.2±1.7 days. Almost all patients were satisfied with the relatively small scar. No major perioperative complications were observed. There was one case of surgical site infection, and three cases received a postoperative blood transfusion. No positive surgical margins were observed in patients who underwent RLESS radical nephrectomy and nephroureterectomy (Table 2).
Since the introduction of laparoscopic surgery in the urologic area, the clinical outcomes of laparoscopic surgery have shown decreased postoperative morbidity, shorter hospitalization and convalescence times, and improved cosmesis compared with open surgery. All urologic intra- abdominal and pelvic procedures are feasible and safe by the laparoscopic approach. However, complications related to port placement have been recognized in laparoscopic surgery [18,19].
Ongoing attempts to reduce surgical morbidity and improve the cosmesis of laparoscopic surgery have stimulated the minimization of the size and number of ports, and as one of the evolving techniques, LESS was recently introduced to aim at performing laparoscopic surgery by consolidating all ports within a single-site incision [1-3]. Since the first LESS nephrectomy for a small nonfunctioning kidney was reported by Rane et al in 2007 [4], various clinical procedures in urology have been successfully completed by using LESS techniques and have evolved rapidly with improving techniques and technology [1-10].
Both transperitoneal and retroperitoneal approaches are available for LESS. However, despite the several advantages of the retroperitoneal approach, RLESS has been less commonly reported because it is more difficult to check anatomical landmarks with RLESS and there is more clashing of laparoscopic instruments due to the relatively small working space compared with the transperitoneal approach [11]. Recently, a large multi-institutional, worldwide series of LESS in urology was reported, in which a total of 1,076 cases of LESS done at 18 institutions were included. The most common procedures were extirpative or ablative operations in the upper urinary tract. Clinical outcomes of LESS were comparable to those of conventional transperitoneal laparoscopic surgery. In that study, 92% of the LESS procedures were performed via the transperitoneal route [10].
After RLESS was first reported independently in 2009 by two groups, White et al and Ryu et al, several researchers have presented their experiences with RLESS [12,13]. White et al performed 8 RLESS procedures, including 5 cases of cryoablation, 1 case of partial nephrectomy, 1 case of cyst decortications, and 1 case of metastectomy [12]. The clinical results showed that RLESS was feasible and offered comparable surgical outcomes and superior cosmesis and pain control compared with conventional retroperitoneoscopy. Ryu et al described single-port laparoscopic urological surgery via the retroperitoneal approach using an Alexis wound retractor with flexible laparoscopic instrumentation [13]. In that study, 14 patients underwent RLESS for renal cyst decortications, adrenalectomy, nephroureterectomy, nephrectomy, and ureterolithotomy. All cases were completed without conversion to conventional laparoscopic or open surgery. There were no major intraoperative complications, but wound dehiscence and bleeding were noted in two patients. Micali et al presented 11 RLESS procedures for renoureteral surgeries such as ureterolithotomy, renal cyst ablation, and renal biopsy [14]. They used a multichannel port with standard and bent instruments and a flexible laparoscope. A total of 10 of 11 procedures were completed without conversion. A single case of ureterolithotomy was converted to open surgery. RLESS was concluded to be a safe and feasible procedure for renal biopsy and renal cyst ablation with a shorter convalescence time, less postoperative pain, and better cosmetic outcomes, but LESS ureterolithotomy was more challenging for the lack of triangulation. Bent laparoscopic instruments were not suitable for the retroperitoneal space.
Chung et al successfully completed seven RLESS adrenalectomies using a homemade single-port and conventional laparoscopic instrumentation without laparoscopic conversion or complications [15]. They reported that RLESS adrenalectomy was a safe and feasible procedure for functional adrenal tumors using conventional laparoscopic instruments.
In our study, 23 of 24 cases of RLESS for upper urinary tract surgery were completed without insertion of the additional port or open conversion. We preferred the retroperitoneal approach to the transperitoneal approach because we have been familiar with conventional retroperitoneal laparoscopic surgery since the first experience of retroperitoneal laparoscopic nephrectomy in 1997. Although RLESS does not make a scarless wound compared with transperitoneal LESS and objective assessment concerning cosmetic satisfaction is difficult, most of the patients were satisfied with the small scar. The operative outcomes of our RLESS renal cyst ablation and simple nephrectomy series were comparable to those of previously reported RLESS studies [13,14,17]. Our initial results showed that, in our experience, RLESS is a technically feasible and safe procedure for upper urinary tract surgery.
The multi-channel port, which allows many instruments to be inserted in the single incision, is necessary for operating RLESS. We used a homemade single-port device that consisted of an Alexis wound retractor and a surgical glove instead of a commercially available port (Fig. 1). It takes 10 to 15 minutes to make the homemade single-port device and there is a possible risk of tearing of the glove or wound retractor, resulting in gas leaking or a loss of insufflation pressure. However, the number and size of the instruments for surgery is freely adjustable and provides a wide range of motion. The glove expanding with insufflation provides additional gap among the instruments, and it enables the instrument to have free movement in a single port. The surgical glove could accommodate the usual insufflation pressure with 12 mm Hg of CO2.
Instrument triangulation is essential for proper dissection along anatomical tissue planes. However, parallel insertion of conventional rigid laparoscopic instruments is difficult to provide sufficient triangulation for the performance of procedures. Therefore, most laparoscopic surgeons use flexible laparoscopic instruments for extirpative or reconstructive urologic surgery to minimize clashing of the instruments during the operation [10]. However, we used conventional rigid laparoscopic instruments despite clashing of the instruments because flexible instruments are difficult to use, are bulky, and do not have sufficient strength to provide robust retraction and dissection in our early experiences. For radical nephrectomy, RLESS was completed by using conventional rigid laparoscopic instruments, although it took a somewhat long time for dissection of the upper pole.
Extraction of the specimen can be considered to be one of the important steps in RLESS. Small specimens can be retrieved without port removal owing to the high elasticity of the homemade single-port device. Large benign specimens placed in an entrapment bag are removed after the specimen is fragmented by use of scissors without extension of the incision at the end of the procedure, because expansion of the incision or making an additional incision reduces the merit of the single-port surgery in terms of the number and size of incisions. For radical nephrectomy, the specimens are extracted via additional Gibson incision or extension of the incision according to oncological principles. For nephroureterectomy, the distal ureterectomy with bladder cuff excision is performed through a modified Gibson incision and then the specimen is removed en bloc. We may consider whether organ-ablative or non-radical surgeries are suitable for RLESS.
RLESS is technically difficult compared with the conventional retroperitoneal laparoscopic surgery and is still in its relative infancy. According to recent clinical studies, the clinical outcomes of RLESS are comparable to those of the conventional retroperitoneal laparoscopic surgery. Shi et al reported outcomes of LESS retroperitoneoscopic adrenalectomy compared with those of conventional retroperitoneoscopic adrenalectomy [16]. There were no significant differences in terms of the estimated blood loss, hospital stay, or postoperative complications between the two groups, but the RLESS group had a longer median operative time, whereas the use of analgesics was significantly less. White et al described a comparative study between RLESS and conventional retroperitoneal laparoscopic cryoablation [12]. The mean operative time was significantly shorter in the conventional laparoscopic groups (120 vs. 174 minutes, p≤0.001). However, the mean VAPS score was 0.4 out of 10 for the RLESS cryoablation and 2.6 out of 10 for the conventional retroperitoneal laparoscopic cryoablation (p=0.023). Other perioperative parameters, including mean tumor size, mean EBL, and mean length of hospital stay were all comparable between the two techniques. Chueh et al performed eight RLESS nephrectomies that were completed successfully without complications [17]. No extra working port was required for any cases. The median operating time was 164 minutes and the median estimated blood loss was 50 ml. The median length of hospital stay was 2 days. The median visual analogue pain scale at discharge was 2 out of 10. These clinical results were comparable with those of their previous retroperitoneoscopic nephrectomy [20].
There are some limitations to this study. We did not attempt to evaluate the comparative outcomes between RLESS and conventional laparoscopy or transperitoneal LESS. In addition, scar satisfaction and quality of life were not evaluated with a validated questionnaire. It is necessary to expand the indication to complex reconstructive procedures such as pyeloplasty, partial nephrectomy, and ureterolithotomy. The power of our conclusions is weakened by the retrospective nature of the study.
The 23 procedures were successfully completed in our initial experience with RLESS for upper urinary tract surgery. The initial outcomes of our experience suggest that RLESS is a technically feasible and safe procedure for use in upper urinary tract surgery. However, RLESS in urology is currently in the initial step. Additional surgical experiences are essential to achieve proficiency, and further refinements in instrumentation and operative techniques will be required. Prospective comparative studies with conventional retroperitoneal laparoscopic surgery or transperitoneal LESS are needed to better establish the role of RLESS in urologic surgery.
References
1. Symes A, Rane A. Urological applications of single-site laparoscopic surgery. J Minim Access Surg. 2011. 7:90–95.
2. Irwin BH, Rao PP, Stein RJ, Desai MM. Laparoendoscopic single site surgery in urology. Urol Clin North Am. 2009. 36:223–235.
3. Autorino R, Stein RJ, Lima E, Damiano R, Khanna R, Haber GP, et al. Current status and future perspectives in laparoendoscopic single-site and natural orifice transluminal endoscopic urological surgery. Int J Urol. 2010. 17:410–431.
4. Rané A, Rao P, Rao P. Single-port-access nephrectomy and other laparoscopic urologic using a novel laparoscopic port (R-port). Urology. 2008. 72:260–263.
5. Choi KH, Ham WS, Rha KH, Lee JW, Jeon Hg, Arkoncel FR, et al. Laparoendoscopic single-site surgeries: A single-center experience of 171 consecutive cases. Korean J Urol. 2011. 52:31–38.
6. Lee JY, Lee SW. Concomitant laparoendoscopic single-site surgery for ureterolithotomy and contralateral renal cyst marsupialization. Korean J Urol. 2011. 52:64–67.
7. Lee SY, Kim YT, Park HY, Lee TY, Park SY. Initial experience with laparoendoscopic single-site surgery by use of a homemade transumbilical port in urology. Korean J Urol. 2010. 51:613–618.
8. Seo IY, Hong HM, Kang IS, Lee JW, Rim JS. Early experience of laparoendoscopic single-site nephroureterectomy for upper urinary tract tumors. Korean J Urol. 2010. 51:472–476.
9. Kim TH, Jeong BC, Seo SI, Jeon SS, Han DH. Transumbilical laparoendoscopic single-site ureterolithotomy for large impacted ureteral stones: initial experiences. Korean J Urol. 2010. 51:403–408.
10. Kaouk JH, Autorino R, Kim FJ, Han DH, Lee SW, Yinghao S, et al. Laparoendoscopic single-site surgery in urology: worldwide multi-institutional analysis of 1076 cases. Eur Urol. 2011. 60:998–1005.
11. Hemal AK. Laparoscopic retroperitoneal extirpative and reconstructive renal surgery. J Endourol. 2011. 25:209–216.
12. White WM, Goel RK, Kaouk JH. Single-port laparoscopic retroperitoneal surgery: initial operative experience and comparative outcomes. Urology. 2009. 73:1279–1282.
13. Ryu DS, Park WJ, Oh TH. Retroperitoneal laparoendoscopic single-site surgery in urology: initial experience. J Endourol. 2009. 23:1857–1862.
14. Micali S, Isgrò G, Stefani SD, Pini G, Sighinolfi MC, Bianchi G. Retroperitoneal laparoendoscopic single-site surgery: preliminary experience in kidney and ureteral indications. Eur Urol. 2011. 59:164–167.
15. Chung SD, Huang CY, Wang SM, Tai HC, Tsai YC, Chueh SC. Laparoendoscopic single-site (LESS) retroperitoneal adrenalectomy using a homemade single-access platform and standard laparoscopic instruments. Surg Endosc. 2011. 25:1251–1256.
16. Shi TP, Zhang X, Ma X, Li HZ, Zhu J, Wang BJ, et al. Laparoendoscopic single-site retroperitoneoscopic adrenalectomy: a matched-pair comparision with the gold standard. Surg Endosc. 2011. 25:2117–2124.
17. Chueh SC, Sankari BR, Chung SD, Jones JS. Feasibility and safety of retroperitoneoscopic laparoendoscopic single-site nephrectomy: technique and early outcomes. 2011. BJU Int;Epub ahead of print.
18. Marcovici I. Significant abdominal wall hematoma from an umbilical port insertion. JSLS. 2001. 5:293–295.
19. Lowry PS, Moon TD, D'Alessandro A, Nakada SY. Symptomatic port-site hernia associated with a non-bladed trocar after laparoscopic live-donor nephrectomy. J Endourol. 2003. 17:493–494.
20. Chueh SC, Chen J, Chen SC, Hsiao PJ, Chiu TY, Lai MK. Simple nephrectomy by retroperitoneoscope. J Formos Med Assoc. 1996. 95:487–489.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download