Abstract
Purpose
Most men with benign prostatic hyperplasia (BPH) have bothersome lower urinary tract symptoms (LUTS). This study aimed to investigate the safety and efficacy of high-performance system (HPS) laser photoselective vaporization of the prostate (PVP) for the treatment of BPH in men with detrusor underactivity (DU).
Materials and Methods
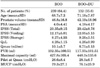
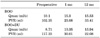
From March 2009, 371 patients with BPH were divided into 2 groups according to the findings of preoperative urodynamic study: 239 (64.4%) patients with bladder outlet obstruction (BOO) and 132 (35.6%) patients with bladder outlet obstruction with detrusor underactivity (BOO+DU). 120 W HPS laser PVP was performed to resolve the BOO. The perioperative data and postoperative results at 1 month and 12 months, including the International Prostate Symptom Score (IPSS), maximum urinary flow (Qmax), and postvoid residual urine (PVR) values, were evaluated.
Results
Compared with the preoperative parameters, significant improvements in IPSS, Qmax, and PVR were observed in each group at 1 and 12 months after the operation. In addition, IPSS, Qmax, and PVR were not significantly different between the BOO and BOO+DU groups at 1 and 12 months after the operation.
Bladder outlet obstruction (BOO) caused by benign prostatic hyperplasia (BPH) is the most common cause of male lower urinary tract symptoms (LUTS) [1,2]. Among patients with BPH, some require surgery owing to the failure of medical treatment or complications such as acute urinary retention, hematuria, and urinary stones. However, about 25% to 35% of patients report dissatisfaction with the results after transurethral resection of the prostate (TUR-P), despite the resolution of the BOO induced by BPH [3-5]. According to one study, there may be other causes of LUTS, such as a functional impairment of the bladder; moreover, men with BPH may have concomitant bladder dysfunction such as detrusor underactivity (DU) [6]. There have been some studies about the effect of surgery such as TUR-P in men with BPH and DU; however, it remains controversial whether elimination of BOO improves LUTS or not.
Urodynamic study is an optional diagnostic modality in patients with BPH. Therefore, it was done in selected patients whose LUTS was suspected to be induced by problems other than BPH. However, men with BPH may have other concomitant abnormalities that influence bladder function. Generally, most men with BPH are older adults; therefore, they also have comorbidities, like diabetes, that influence bladder function. Also, bladder function in older adults can be altered by aging itself. As a result, LUTS in these men can be induced by mixed etiologies rather than BPH alone. Therefore, if we get information about bladder function as well as the degree of BOO through preoperative urodynamic study, it would be a great help in selecting good candidates for surgery as well as in predicting postoperative outcomes.
Recently, there have been many reports about the effect of laser surgery for BPH. This procedure shows similar effects and patient satisfaction with conventional TUR-P and, in addition, may have several advantages compared with TUR-P. Retrograde ejaculation and urethral stricture are reported to be lower than with TUR-P. Particularly, the 120 W high-performance system (HPS) laser has been regarded as an effective and safe procedure among the various types of laser surgery for BPH [7-10].
Therefore, we evaluated the short- and long-term outcomes according to the degree of detrusor contractility by preoperative urodynamic study in patients with BPH after 120 W HPS laser surgery.
The subjects were patients who were diagnosed as having BPH, who underwent 120 W Greenlight HPS laser photoselective vaporization of the prostate (PVP) from March 2009, and who were available for follow-up for up to 12 months after surgery. History taking, physical examination, prostate-specific antigen (PSA) measurement, transrectal ultrasonography, the International Prostate Symptom Score (IPSS) questionnaire, and urodynamic study were performed in all patients. Patients with a history of neurogenic bladder, prostate cancer, or urethral stricture were excluded.
Pressure-flow study (PFS) was performed on the patients, and the degree of BOO and the contractility of the detrusor muscle were assessed by use of the Schäfer nomogram. Patients maintained alpha-blocker medication during PFS and uroflowmetry. According to the results of the PFS, the patients were divided into two groups: the group with BOO only (BOO group) and the group with BOO with DU (BOO+DU group). We defined DU as patients whose contractility was lower than weak by the Schäfer nomogram.
Indications for operation were persistent symptoms even after the administration of alpha-blockers or the combination of alpha-blockers and 5 alpha reductase inhibitors for longer than 3 months and cases in which medications were avoided because of the side effects.
General or spinal anesthesia was used, and the surgery was performed by a single surgeon. A continuous irrigation system 22 Fr resectoscope with a 30 degree lens and a 75 degree laser fiber was used. All prostate tissue causing obstruction was removed until a fine surgical cavity was formed, as in TURP. An 18 Fr urethral catheter was placed after the operation and was removed the next day, taking into consideration the degree of hematuria.
Operation time, the energy used during the operation, the catheter indwelling period, and the hospitalization period were analyzed. The outcomes and effectiveness of surgery at 1 month and 12 months after surgery were compared with preoperative values by assessing the IPSS, maximal flow rate (Qmax), and postvoid residual urine volume (PVR).
Postoperative Qmax, PVR, and IPSS with quality of life (QoL) score were obtained at 1 and 12 months after surgery. Operation time, amount of applied energy, and duration of catheterization were assessed. SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Postoperative Qmax, PVR, IPSS, and QoL score were compared with preoperative values by using the t-test; p-values of less than 0.05 were defined as significant.
A total of 371 patients were selected. The mean age of the patients was 69.3±8.6 years.
The patient group with only BOO included 239 cases (64.4%), and the patient group with BOO+DU included 132 patients (35.6%). Patient distribution of DU was analyzed according to the Schäfer nomogram as weak+, weak-, and very weak. The number of patients in the weak+ group was 92, that in the weak- group was 32, and that in the very weak group was 8 (Fig. 1).
The patients' preoperative clinical characteristics, such as age, prostate volume, PSA level, and IPSS, were compared, and there were no significant differences between the two groups. In addition, there were no statistically significant differences in the Qmax or PVR between these two groups (Table 1). There were no significant differences in operation time, lasing time, total laser energy, or postoperative urinary catheter indwelling time between these two groups (Table 2).
One month after the operation, the total IPSS of the BOO group was significantly improved from 20.35±9.15 points to 9.92±7.16 points. The voiding symptom score was significantly improved from 12.17±5.01 points to 6.64±6.16 points, and the storage symptom score was improved from 8.27±4.55 points to 4.31±3.06 points at 1 month after the operation. All changes were significant (p<0.05).
The total IPSS of the BOO+DU group was significantly improved from 20.42±8.78 to 10.63±8.47, and the voiding symptom score was significantly improved from 12.05±5.15 to 7.22±5.60. The storage symptom score was significantly improved from 9.26±3.51 to 5.17±3.76 at 1 month after the operation (p<0.05).
One month after the operation, the QoL score in the BOO group was significantly improved from 4.28±1.15 to 2.00±1.13, and in the BOO+DU group, the QoL score was significantly improved from 4.26±0.99 to 2.77±1.41 (p<0.05).
In the BOO group, compared with preoperative data, the postoperative 1 month Qmax was improved from 10.1±5.7 ml/s to 15.3±9.05 ml/s and PVR was improved from 102.35±100.51 ml to 23.08±21.61 ml. In the BOO+DU group, postoperative 1 month Qmax was improved from 8.71±5.15ml/s to 13.35±7.80 ml/s, and PVR was improved from 117.33±101.51 ml to 30.01±40.34 ml. All changes were significant (p<0.05).
At 12 months after the operation, in the BOO group, total IPSS, voiding symptom score, storage symptom score, QoL score, Qmax, and PVR showed significant improvement compared with preoperative data (p<0.05). In the BOO+DU group at 12 months after the operation, total IPSS, voiding symptom score, storage symptom score, QoL score, Qmax, and PVR showed significant improvement compared with preoperative data (p<0.05).
There were no significant differences between the BOO and BOO+DU groups at the same time interval period after the operation (postoperative 1 and 12 months (Tables 3, 4).
There were no severe postoperative complications that required re-hospitalization or re-do operation for gross hematuria, retrograde ejaculation, urethral stricture, or urinary tract infection. Acute urinary retention was observed in a total of 27 patients (7%): 14 cases in the BOO group and 13 cases in the BOO+DU group. In all cases, only temporary urinary catheterization for 2 weeks was needed. After the catheter was removed, the patients were all able to void well. A total of 48 cases (13%) of mild dysuria were observed: 21 cases in the BOO group and 27 cases in the BOO+DU group. In all cases, the symptoms were managed by follow-up or conservative care such as temporary analgesic medications.
In the patients with BOO associated with impaired detrusor contractility, it is still controversial whether eliminating BOO improves LUTS. But, according to our results, patients with BOO and DU showed improvements in preoperative LUTS and were satisfied about their postoperative results after relief of BOO by the 120 W HPS laser.
BPH is the major cause of male LUTS, and the symptoms in many patients with BPH are related to BOO induced by enlargement of the prostate. However, BOO may not develop in all patients with BPH, and LUTS in some patients with BPH are associated with not only BOO but also bladder function. Some investigators reported that BOO is observed in about 50% to 70% of males with BPH; moreover, 37% to 47% of patients with BPH also have bladder dysfunction such as impaired detrusor contractility as well as BOO [6,11]. Several factors influence bladder function. Impaired detrusor contractility can be induced by BOO itself, because alteration of bladder function can appear as a secondary change following BOO. In addition, hormonal changes, aging, concomitant disease, and neurologic disorders can affect bladder function and lead to impairment of detrusor contractility [5]. Most patients with BPH are of old age, and aging is one of the factors that affect bladder function. Moreover, the incidence of a lower testosterone level and diseases such as diabetes or stroke increase in males with old age. These are among the factors that affect bladder function. As a result, LUTS in several patients with BPH may be related to both BOO and functional impairment of the bladder. Similar to previous reports, we also observed that 35.6% of BPH patients who needed surgical treatment showed BOO and DU in this study. Therefore, assessment of detrusor function as well as BOO in men with LUTS induced by BPH is important for selecting a treatment strategy and, in addition, may help to predict which patients need additional medications after relieving BOO [12].
There have been several studies about the usefulness of preoperative urodynamic study. Abrams et al reported that the success rate of the operation was approximately 72% when urologists select surgical candidates according to Qmax only [13]. However, the success rate of surgery rose to 88% when the candidates for surgery were selected by the results of urodynamic evaluation including PFS. This higher success rate after surgery suggested that it is possible to diagnose the patients who have true BOO. In such a manner, urodynamic study is a helpful method for evaluating patients with BOO. Thus, urodynamic study could be of great help in the selection of patients before surgery and in the prediction of postsurgical prognosis [12,14,15].
Because of deterioration of bladder emptying, DU leads to a decreased flow rate and higher PVR. Therefore, it was thought that men with BOO and DU would have greater PVR and a higher IPSS as well as lower flow rates compared with those without DU [16,17]. However, in this study, only a small difference was observed in Qmax and PVR between the BOO only and BOO+DU groups preoperatively, and the difference was not significant. We supposed that this result was related with voiding by abdominal straining in the patients in the BOO+DU group, because an elevation in abdominal pressure was noted in most of the patients in the BOO+DU group during PFS. In addition, the severity of DU might be mild compared with that in other previous studies.
The effect of surgery in BPH patients with BOO and DU is still controversial. DU is one of the important factors that influences the prognosis of BPH treatment and is found in approximately 20% to 25% of males with LUTS. Thomas et al reported in a study conducted on patients with DU that deterioration of detrusor muscle contractility is the major cause of persistent symptoms after surgery [14]. Thus, DU has been considered to be a risk factor that predicts poor prognosis even after surgery in patients with BPH [18,19]. There were reports that LUTS can be improved by eliminating BOO through transurethral surgery or photoselective vaporization of the prostate in patients with BPH without postoperative alterations of detrusor contractility [15,20]. In addition, Monoski et al reported that even in BPH patients with impaired detrusor contractility and a preoperative history of urinary retention, eliminating BOO by KTP laser improves both subjective and objective parameters [21]. Park et al reported that there were significant improvements in Qmax, voiding urine volume, PVR, IPSS, and QoL scores at 6 months after PVP treatment [22]. In our study, similarly, in the BOO with DU group, 1 month after 120 W HPS laser operation, IPSS scores, QoL, Qmax, and PVR were improved and the improvements were maintained for 12 months. During the follow-up period, in the BOO with DU group, cholinergic medication was able to be reduced to less than preoperative doses or stopped altogether after the operation in almost all patients. In this study, most of the men with BOO induced by BPH benefited from 120 W HPS laser with an improvement in both subjective and objective voiding parameters regardless of the presence of DU.
Additionally, further evaluation is necessary about the effect of concomitant DU on outcomes after BPH surgery because bladder function can deteriorate as patients grow older. As a result, more long-term follow-up is needed to evaluate the changes in LUTS in patients with BOO and DU.
Figures and Tables
 | FIG. 1Distribution of patients according to the Schäfer nomogram. The number of patients who showed weak (+) contractility was 92, the number who showed weak (-) contractility was 32, and the number who showed very weak contractility was 8. The patient group with detrusor underactivity included 132 patients. |
References
1. Chaikin DC, Blaivas JG. Voiding dysfunction: definitions. Curr Opin Urol. 2001. 11:395–398.
2. Grossfeld GD, Coakley FV. Benign prostatic hyperplasia: clinical overview and value of diagnostic imaging. Radiol Clin North Am. 2000. 38:31–47.
3. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989. 141:243–247.
4. Doll HA, Black NA, McPherson K, Flood AB, Williams GB, Smith JC. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992. 147:1566–1573.
5. Andersson KE. Storage and voiding symptoms: pathophysiologic aspects. Urology. 2003. 62:5 Suppl 2. 3–10.
6. Abrams P. Objective evaluation of bladder outlet obstruction. Br J Urol. 1995. 76:Suppl 1. 11–15.
7. Sohn JH, Choi YS, Kim SJ, Cho HJ, Hong SH, Lee JY, et al. Effectiveness and safety of photoselective vaporization of the prostate with the 120 W HPS greenlight laser in benign prostatic hyperplasia patients taking oral anticoagulants. Korean J Urol. 2011. 52:178–183.
8. Kang SH, Choi YS, Kim SJ, Cho HJ, Hong SH, Lee JY, et al. Long-term follow-up results of photoselective vaporization of the prostate with the 120 W greenlight HPS laser for treatment of benign prostatic hyperplasia. Korean J Urol. 2011. 52:260–264.
9. Bachmann A, Schürch L, Ruszat R, Wyler SF, Seifert HH, Müller A, et al. Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP): a prospective bi-centre study of perioperative morbidity and early functional outcome. Eur Urol. 2005. 48:965–971.
10. Ko DW, Jeong BC, Son H. Initial experiences with a new 120 W greenlight (TM) high-power system for photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia in Korea. Korean J Urol. 2009. 50:1089–1094.
11. Lee JG, Shim KS, Koh SK. Incidence of detrusor underactivity in men with prostatism older than 50 years. Korean J Urol. 1999. 40:347–352.
12. Jung YS, Hwang TK, Kim JC. The outcome and satisfaction of patients with lower urinary tract symptoms/benign prostatic hyperplasia following transurethral resection of the prostate according to urodynamic obstruction and the bladder function. Korean J Urol. 2007. 48:965–970.
13. Abrams PH, Farrar DJ, Turner-Warwick RT, Whiteside CG, Feneley RC. The results of prostatectomy: a symptomatic and urodynamic analysis of 152 patients. J Urol. 1979. 121:640–642.
14. Thomas AW, Cannon A, Bartlett E, Ellis-Jones J, Abrams P. The natural history of lower urinary tract dysfunction in men: the influence of detrusor underactivity on the outcome after transurethral resection of the prostate with a minimum 10-year urodynamic follow-up. BJU Int. 2004. 93:745–750.
15. Gotoh M, Yoshikawa Y, Kondo AS, Kondo A, Ono Y, Ohshima S. Prognostic value of pressure-flow study in surgical treatment of benign prostatic obstruction. World J Urol. 1999. 17:274–278.
16. Oelke M, Höfner K, Jonas U, de la Rosette JJ, Ubbink DT, Wijkstra H. Diagnostic accuracy of noninvasive tests to evaluate bladder outlet obstruction in men: detrusor wall thickness, uroflowmetry, postvoid residual urine, and prostate volume. Eur Urol. 2007. 52:827–834.
17. Kang MY, Ku JH, Oh SJ. Non-invasive parameters predicting bladder outlet obstruction in Korean men with lower urinary tract symptoms. J Korean Med Sci. 2010. 25:272–275.
18. Seki N, Takei M, Yamaguchi A, Naito S. Analysis of prognostic factors regarding the outcome after a transurethral resection for symptomatic benign prostatic enlargement. Neurourol Urodyn. 2006. 25:428–432.
19. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006. 50:969–979.
20. Masumori N, Furuya R, Tanaka Y, Furuya S, Ogura H, Tsukamoto T. The 12-year symptomatic outcome of transurethral resection of the prostate for patients with lower urinary tract symptoms suggestive of benign prostatic obstruction compared to the urodynamic findings before surgery. BJU Int. 2010. 105:1429–1433.
21. Monoski MA, Gonzalez RR, Sandhu JS, Reddy B, Te AE. Urodynamic predictors of outcomes with photoselective laser vaporization prostatectomy in patients with benign prostatic hyperplasia and preoperative retention. Urology. 2006. 68:312–317.
22. Park KS, Cho YS, Joo KJ. Potassium-titanyl-phosphate laser photoselective vaporization of the prostate in patients with benign prostatic hyperplasia with detrusor underactivity: influence on detrusor pressure. Korean J Urol. 2009. 50:1193–1197.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download