Abstract
Purpose
We aimed to determine whether prediagnostic lower urinary tract symptoms (LUTS) are associated with the aggressiveness of nonmetastatic prostate cancer (PCa) and compared the clinicopathologic features of PCa patients with and without preexisting LUTS.
Materials and Methods
We retrospectively reviewed the medical records of 295 prostate cancer patients who underwent a radical prostatectomy (RP) by a single surgeon from 2006 to 2010. A total of 205 patients were assigned to two groups according to whether they showed preoperative LUTS (International Prostate Symptom Score [IPSS]≥8). Clinical, operative, pathologic, and postoperative functional data were collected.
Results
The mean age at RP was 62.7 years in the no LUTS group (group A, n=108) and 64.7 in the LUTS group (group B, n=97). The baseline mean IPSS score was 6.1 in group A and 14.6 in group B (p=0.029). The incidence of pathologic T3a stage or above was significantly higher in group B than in group A (p=0.036). The mean postoperative follow-up period was 16.8 months (range, 4 to 38 months). The mean time to biochemical recurrence was 16.9 and 18.2 months in groups A and B, respectively (p=0.148). The median time to recovery of urinary incontinence was 3.6 and 3.3 months in groups A and B, respectively.
Generally, serum prostate-specific antigen (PSA) testing in clinical practice is used either in the screening of asymptomatic men or in the workup of men with lower urinary tract symptoms (LUTS). Although an elevated PSA level can be an important predictor of prostate cancer (PCa), it may also be indicative of benign prostatic hyperplasia. Several studies have reported a weak association between LUTS and the detection of PCa [1,2]. Men with LUTS are often concerned that their symptoms indicate PCa [3]. They believe the PSA evaluation to be more effective for the detection of PCa than do men who have not been tested [4]. PSA, Gleason score at biopsy, and clinical stage are currently the most reliable markers of aggressiveness or prognosis for PCa [3]. However, controversy exists regarding whether prediagnostic LUTS affects the aggressiveness of PCa [1,5]. Collin et al reported that associations of LUTS with PCa did not differ between localized or advanced PCa [1]. In our study, we aimed to determine whether prediagnostic LUTS are associated with the aggressiveness of nonmetastatic PCa and compared the clinicopathologic features of PCa patients with and without preexisting LUTS.
We retrospectively reviewed the medical records of 295 prostate cancer patients who underwent a radical prostatectomy (RP) by a single surgeon from 2006 to 2010. In our study, prostate cancer diagnosis took one of the following two main routes: asymptomatic diagnosis following a screening test or symptomatic diagnosis with LUTS. All patients attended the center's urology department at the initial visit for completion of an International Prostate Symptom Score (IPSS) questionnaire, digital rectal examination, PSA test, and transrectal ultrasound (TRUS) (12 cores). We defined the LUTS group as those with IPSS ≥8 and the no LUTS group as those with IPSS <8.
After excluding those patients with unclear medical records, a history of medication with an alpha blocker or 5 alpha reductase inhibitor, a history of prostate surgery, clinically insignificant PCa according to the Epstein criteria, or a history of prostatitis, 205 patients were assigned to two groups according to the presence or absence of preoperative LUTS: group A (no LUTS, IPSS<8) and group B (LUTS, IPSS≥8) [6]. Clinical, operative, pathologic, and postoperative functional data were collected. Biochemical recurrence was defined as three consecutive rises in the PSA level, each >3 months apart, with a final value greater than 1.0 ng/ml [7,8]. Postoperative continence was defined as being pad-free.
A kit from BK Medical (Herlev, Denmark), was used for TRUS, and an automatic gun was used for 12 prostatic biopsies (right 6 cores and left 6 cores). The 12 core biopsies were done in each patient by an urologist with 12 years of experience. The 12 core biopsy regimen was performed according to a previously established standard biopsy protocol [9]. The standard length of the biopsy cores was 15 mm and each core was embedded separately and submitted in multiple containers.
Pathological grading was done by the Gleason scoring system, and pathologic review was performed by a single experienced urologic pathologist (SWH). The prostatectomy specimens were fixed overnight (10% neutral buffered formaldehyde) and coated with India ink. Transverse whole-mount step-section specimens were obtained at 4 mm intervals on a plane. The presence and extent of cancer were outlined on the glass cover. The presence of tumor cells beyond the capsular margin was defined as extracapsular extension.
Statistical analyses were performed by using a Student's t-test to evaluate the demographic and clinical differences between the LUTS and no LUTS groups. A Pearson's chi-squared test was used to compare groups for categorical variables. The Kaplan-Meier method was used to compare the duration of continence recovery and the biochemical recurrence rate. The log rank test analyzed the difference between the two groups, and a p-value of <0.05 was considered significant. All data were analyzed by using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Statistical analysis was performed with the Graphpad Prism ver. 5.00 (Graphpad Instat, San Diego, CA, USA).
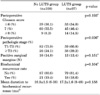
The mean age at RP was 62.7 years in the no LUTS group (group A, n=108) and 64.7 years in the LUTS group (group B, n=97). Other preoperative baseline parameters such as past history, body mass index, and clinical stage were not statistically different between the two groups. The baseline mean IPSS score was 6.1 in group A and 14.6 in group B (p=0.029), and the mean quality of life score was 2.6 in group A and 4.2 in group B (p=0.013). There was no significant difference in preoperative prostate-specific antigen levels (10.1 vs. 11.2 ng/ml in groups A and B, respectively) (Table 1). The prostate volume was large in the LUTS group (39.8 cc) compared with the no LUTS group (34.5 cc); however, there was no significant difference between the two groups.
The incidence of a pathologic stage of T3a or above was significantly higher in group B than in group A (p=0.036). After RP, the incidence of Gleason scores of 7 or more was 69 (64.8%) and 59 (60.9%) in groups A and B, respectively. The incidence of a positive surgical margin showed no significant difference between the two groups (Table 2). In the multivariate analysis, IPSS total scores and biopsy Gleason scores were predictable values for locally advanced PCa (Table 3).
The mean postoperative follow-up period was 16.8 months (range, 4 to 38 months) (Table 2). We used the Kaplan-Meier analysis to compare the biochemical recurrence rate between the two groups (Fig. 1). The mean time to biochemical recurrence was 16.9 and 18.2 months in groups A and B, respectively (p=0.148). The median time to recovery of urinary incontinence was 3.6 and 3.3 months in groups A and B, respectively. This result did not differ significantly between the two groups.
In the present study, more than half (52.7%) of the men with no baseline LUTS were diagnosed with PCa and underwent RP. In addition, we demonstrated that the group with no LUTS at baseline had a favorable pathologic stage (≤T2) of PCa after RP compared with the LUTS group, even though this result did not affect the biochemical recurrence rate. However, there was no evidence of a positive association with advanced PCa, which was partially contradictory to our results. Because most PCa develops in the peripheral zone of the prostate and needs to be advanced before provoking LUTS, a positive association with advanced cancer would be expected if such cancers truly caused LUTS. Our results indicate that the prospect of benefit outweighs the potential for harm and that screening for early PCa is worthwhile even though the value of population-based screening has to be demonstrated in well-conducted randomized trials.
There is a widespread misconception that the risk of PCa is increased with the severity of LUTS, but a lack of cancer symptoms does not mean that there is no cancer. Catalona et al found that the absence of prostatic disease symptoms is more predictive of cancer than their presence [10]. In addition, there are many reports that patients with baseline LUTS are not at higher risk for PCa than are asymptomatic men [1,8,11]. Especially, men with a PSA level of ≥3 ng/ml and LUTS were more likely to be diagnosed with benign disease than with PCa [1]. However, the present study included only patients treated with RP, and the data therefore give no information about patients referred to the department with or without symptoms who did not have a diagnosis of PCa or any nonsurgical treatment thereof. Our results warrant future study to determine the "pure" incidence of prostate cancer in the screened population of Korea.
In the present study, there were no significant differences in postoperative Gleason scores, biochemical recurrence, or positive surgical margins, regardless of the presence or absence of baseline LUTS. This finding is important, because measurement of PSA when a patient has LUTS is controversial. Regardless of the PCa detection rate according to baseline LUTS, our results suggest that there might be more aggressive pathologic features in the no LUTS group if the subjects had not participated in PCa screening. Some authors insist that PSA testing in men with LUTS should be standard procedure, whereas others believe it is the equivalent of screening and therefore inappropriate [12,13]. The incidence of PCa has rapidly increased over the past 10 years in East Asia, including Korea [14,15]. In South Korea, PSA screening is not yet recommended in the national early detection strategy for cancer, even though a growing proportion of patients undergoing RP are asymptomatic and are diagnosed as a result of unsystematic PSA screening. In a 2004 telephone survey of over 700 Korean men older than 50 years in a small city, approximately 15% had been screened for PCa during the previous 2 years (unpublished data), a much lower rate than the 75% reported for men in the United States [16]. In view of the growing proportion of asymptomatic PCa, we suggest that PSA screening is needed not only in men with LUTS that could be caused by PCa, but also in men who are asymptomatic at baseline [17,18].
There are several limitations to our study. First, the short duration with a relatively small number of patients requires further investigation for a longer period of time with a larger number of patients. In fact, we could not explain the exact background by which the correlation between low IPSS and low T stage was made. We think this will be an important point to clarify in future studies. Also, we were unable to include advanced or metastatic PCa cases because only RP patients were included in our study. Therefore, this study cannot assess the relationship between LUTS and more advanced or metastatic PCa.
Figures and Tables
FIG. 1
Kaplan-Meier analysis of time to biochemical recurrence (A) and recovery of continence (B) for patients with and without baseline lower urinary tract symptoms. BCR: biochemical recurrence, IPSS: international prostate symptom score.

References
1. Collin SM, Metcalfe C, Donovan J, Lane JA, Davis M, Neal D, et al. Associations of lower urinary tract symptoms with prostate-specific antigen levels, and screen-detected localized and advanced prostate cancer: a case-control study nested within the UK population-based ProtecT (Prostate testing for cancer and Treatment) study. BJU Int. 2008. 102:1400–1406.
2. Porter CR, Kim J. Low AUA symptom score independently predicts positive prostate needle biopsy: results from a racially diverse series of 411 patients. Urology. 2004. 63:90–94.
3. Brown CT, O'Flynn E, Van Der Meulen J, Newman S, Mundy AR, Emberton M. The fear of prostate cancer in men with lower urinary tract symptoms: should symptomatic men be screened? BJU Int. 2003. 91:30–32.
4. Steginga SK, Occhipinti S, McCaffrey J, Dunn J. Men's attitudes toward prostate cancer and seeking prostate-specific antigen testing. J Cancer Educ. 2001. 16:42–45.
5. Tubaro A, De Nunzio C, Mariani S, Trucchi A, Miano R, Vicentini C, et al. Reduction of prostate specific antigen after tamsulosin treatment in patients with elevated prostate specific antigen and lower urinary tract symptoms associated with low incidence of prostate cancer at biopsy. Urology. 2010. 76:436–441.
6. Bastian PJ, Mangold LA, Epstein JI, Partin AW. Characteristics of insignificant clinical T1c prostate tumors. A contemporary analysis. Cancer. 2004. 101:2001–2005.
7. Consensus statement: guidelines for PSA following radiation therapy. American Society for Therapeutic Radiology and Oncology Consensus Panel. Int J Radiat Oncol Biol Phys. 1997. 37:1035–1041.
8. Cookson MS, Aus G, Burnett AL, Camby Hagino ED, D'Amico AV, Dmochowski RR, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol. 2007. 177:540–545.
9. Gore JL, Shariat SF, Miles BJ, Kadmon D, Jiang N, Wheeler TM, et al. Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J Urol. 2001. 165:1554–1559.
10. Catalona WJ, Richie JP, Ahmann FR, Hudson MA, Scardino PT, Flanigan RC, et al. Comparison of digital rectal examination and serum prostate specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 men. J Urol. 1994. 151:1283–1290.
11. Matsubara A, Yasumoto H, Teishima J, Seki M, Mita K, Hasegawa Y, et al. Lower urinary tract symptoms and risk of prostate cancer in Japanese men. Int J Urol. 2006. 13:1098–1102.
12. Farmer A. 10-minute consultation: Prostatic symptoms. BMJ. 2001. 322:1468.
13. Jenkins L, Rose P, Wilson T. Prostatic symptoms. Isn't use of prostate specific antigen tests just screening by the back door. BMJ. 2001. 323:750–751.
14. Sim HG, Cheng CW. Changing demography of prostate cancer in Asia. Eur J Cancer. 2005. 41:834–845.
15. Park SK, Sakoda LC, Kang D, Chokkalingam AP, Lee E, Shin HR, et al. Rising prostate cancer rates in South Korea. Prostate. 2006. 66:1285–1291.
16. Sirovich BE, Schwartz LM, Woloshin S. Screening men for prostate and colorectal cancer in the United States: does practice reflect the evidence? JAMA. 2003. 289:1414–1420.
17. Borre M. Screening by lower urinary tract symptoms vs asymptomatic prostate-specific antigen levels leading to radical prostatectomy in Danish men: tumour characteristics and treatment outcome. BJU Int. 2009. 104:205–208.
18. Kim JM, Song PH, Kim HT, Moon KH. Effect of obesity on prostate specific antigen, prostate volume, and international prostate symptom score in patients with benign prostatic hyperplasia. Korean J Urol. 2011. 52:401–405.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download