Abstract
Purpose
To assess the ability of preoperative variables to predict extracapsular extension (ECE) and positive surgical margin (PSM) in radical prostatectomy patients with prostate-specific antigen (PSA) levels of less than 10 ng/ml.
Materials and Methods
From January 2008 to December 2009, 121 patients with prostate cancer with PSA levels lower than 10 ng/ml who underwent radical prostatectomy were enrolled in the study. The differences in clinical factors (age, PSA, PSA density [PSAD], digital rectal examination [DRE] positivity, positive magnetic resonance imaging [MRI], Gleason sum, positive core number, and positive biopsy core percentage) with ECE and the presence of positive margins were determined and their independent predictive significances were analyzed.
Results
The ECE-positive patients had higher PSA, PSAD, and MRI-positive percentages, and PSM patients had higher PSA, PSAD, MRI-positive percentages, Gleason sum, and positive biopsy core percentages for prostate cancer. In the multivariate analysis, PSAD and MRI positivity were the best independent predictors for ECE, and PSA and PSAD were the best independent predictors of PSM. By receiver operating characteristic curve analysis, PSAD had better discriminative area under the curve value than did PSA for ECE (0.765 vs 0.661) and PSM (0.780 vs 0.624). The best predictive PSAD value was 0.29 ng/ml/cc for ECE and 0.27 ng/ml/cc for PSM.
Prostate cancer is best cured by radical prostatectomy when the disease is organ-confined and the pathologic stage after surgery is known to be related with cancer control. Predicting the pathological stage of a prostate cancer is important for deciding on a treatment strategy, but current clinical methods, including imaging or examination tools, are still of limited value for given patients, especially those with intermediate risk [1,2].
Prostate-specific antigen (PSA) has been used as a criterion for consideration for prostate biopsy, and 30% to 35% of men with PSA less than 10 ng/ml will be found to have prostate cancer [3]. Usually, 80% of men with PSA less than 4.0 ng/ml have pathologically proven organ-confined disease, and 66% of men with PSA levels between 4.0 and 10.0 ng/ml have organ-confined disease [4]. In other words, 20% to 34% of prostate cancer patients have extraprostatic disease regardless of low to intermediate PSA levels (less than 10 ng/ml). Shinohara et al reported the ability of the serum PSA level to predict the pathologic stage [5]. On the other hand, Partin et al failed to utilize serum PSA to determine the pathologic stage of clinically localized prostate cancer. They could not find a correlation between serum PSA and pathologic stage [6].
Because of variable PSA production by individual prostate cancer cells and wide variation in the contribution of benign prostatic hyperplasia to serum PSA levels, risk analysis based on only the PSA level seems incomplete if the PSA level is low to intermediate.
Extracapsular extension (ECE) and positive surgical margin (PSM) are important findings because of their implications for tumor biology, disease recurrence, and cancer survival [7,8]. In this study, we tried to determine the correlation between preoperative predictive factors such as digital rectal examination (DRE) findings, magnetic resonance imaging (MRI) findings, PSA with prostate-specific antigen density (PSAD), and biopsy characteristics and ECE and PSM as pathological outcomes in 121 radical prostatectomy patients with PSA less than 10 ng/ml.
From January 2008 to December 2009, we evaluated 121 prostate cancer patients with PSA lower than 10 ng/ml who underwent radical prostatectomy performed by the standard transperitoneal approach with the interfacial technique as previously reported [9]. Patients who had undergone previous surgery for benign prostatic hypertrophy or who had received hormonal or radiation therapy previous to robot-assisted laparoscopic radical prostatectomy (RALP) were excluded. These 121 men underwent transrectal prostate biopsies owing to elevated PSA levels of ≥4 ng/ml or abnormal DRE findings or abnormal hypoechoic lesions on transrectal ultrasonography (TRUS). For PSA testing, patients' serum was obtained before prostatic manipulations. Prostate volume was defined by measuring the height (H), width (W), and length (L) of the prostate from two selected orthogonal views and calculating the volume (V) as that of the corresponding ellipsoid formula: V=0.52xWxHxL [10]. PSAD was obtained by dividing serum PSA levels by the individual prostate volumes measured by TRUS. All patients underwent a DRE and endorectal MRI to determine preoperative prostate status. Tumors that MRI showed to be attached to the prostate capsule or tumors with a localized bulge were classified as suspected extracapsular extension. Systematic biopsies were obtained for 6 to 13 cores from separate regions, with at least 3 cores from each of both lobes. The total core number and positive core number of biopsies per patient were verified. Biopsy specimens were taken from different areas of the prostate assigned to proper Gleason scores. Pathological staging of the radical prostatectomy specimen was performed and organ-confined cancer was designated as long as the capsule was not penetrated. Histopathologic data of radical prostatectomy specimens including capsule penetration and surgical margin were recorded. ECE was defined as a tumor extending outside of the prostate into the periprostatic soft tissues; accordingly, tumor invasion of the prostatic capsule without penetration was not ECE.
Once the patients were identified, we performed univariate analysis to determine the differences by pathologic outcome (ECE positivity and PSM) in age, PSA, PSAD, DRE positivity, and MRI positivity. Biopsy characteristics (Gleason sum, number of positive cores, and positive biopsy core percentage for prostate cancer) were also compared. Next, the significant predictors were entered into a logistic regression test to determine their independent predictive significance. All statistical analysis was performed by using the Mann Whitney U-test, Pearson's chi-square test for univariate analysis, and logistic regression for multivariate analysis. Receiver operating characteristic (ROC) curves were used to compare the diagnostic power and determine the cutoff value associated with ECE and PSM positivity. SPSS version 12.0 (SPSS Inc., Chicago, IL, USA) was used and a p-value below 0.05 was considered statistically significant.
Table 1 lists the patients' characteristics. The patients' mean age was 62.6 years (range, 46 to 75 years). The mean pre-biopsy PSA level was 6.65 mg/l, mean prostate volume was 27.89 g, and mean PSAD was 0.31 (range, 0.07 to 1.10). Twenty-six patients had palpable tumors and 18 patients had ECE on MRI. The median number of total cores was 8.7. The percentage of positive cores was derived from the number of positive biopsy cores divided by the total number of biopsy cores per patient multiplied by 100. The median positive core number and the percentage of positive cores were 2.48 (range, 1 to 6) and 26.03% (range, 7.69% to 62.50%), respectively.
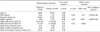
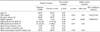
Table 2 shows the association of clinical and biopsy features with ECE in radical prostatectomy patients. By univariate analysis, ECE-positive patients had higher PSA (7.37 vs. 6.32 ng/ml), PSAD (0.43 vs. 0.26 ng/ml/cc) level, and MRI positivity (39.28% vs. 7.53%). In the multivariate analysis, PSAD and MRI positivity were the best independent predictors of ECE. In the ROC curve analysis of PSA and PSAD, PSAD showed better discriminative AUC value (0.765) than did PSA (0.661) for ECE (Fig. 1A). In Table 3, the analysis of associated factors for PSM showed that PSM patients had higher PSA (7.42 vs. 6.28 ng/ml), PSAD (0.44 vs. 0.25 ng/ml/cc) level, and MRI positivity for ECE (26.01% vs. 12.24%). As for biopsy characteristics, Gleason sum (6.97 vs. 6.25) and percentage of biopsy cores positive for prostate cancer (29.92% vs. 24.14%) were higher in PSM patients. In the multivariate analysis, however, only PSA and PSAD were independent predictors of PSM statistically. The ROC curve showed diagnostic value of PSA and PSAD for PSM, and PSAD had better discriminative AUC value (0.780) than did PSA (0.624) (Fig. 1B). The best predictive PSAD value for ECE was 0.29 ng/ml/cc (sensitivity 0.72, specificity 0.68) and 0.27 ng/ml/cc (sensitivity 0.82, specificity 0.67) for PSM.
Pathological stage is usually predicted preoperatively to evaluate the possibility of cure by a particular therapy. Reliable assessment of organ-confined prostatic cancer would be the best available method for complete removal without increasing the incidence of avoidable PSMs. Several established reports have tried to show the probability of PSM or ECE positivity by use of preoperative variables, such as clinical stage, PSA, and biopsy features [7,10-12].
Despite preoperative staging with the use of these parameters, pathologic evaluation shows that a significant number of patients undergoing radical prostatectomy have extraprostatic disease and positive resection margins. Patients with organ-confined prostatic cancer have significantly greater 5 year disease-free survival than do those with disease that is not organ-confined, and several studies have shown that PSM is an independent adverse predictor of pathologic outcome and significantly correlates with the progression-free survival rate [11,13-15].
Former studies have shown that combining Gleason score, clinical stage, and PSA allows the estimation of organ-confined prostate cancer. However, for the intermediate-risk patient group, little additional information may be expected from those characteristics for predicting organ-confined disease [16,17]. In our study of 121 prostate cancer patients with a low to intermediate PSA level, biopsy Gleason score, DRE positivity, and mean number of positive cores showed no significant relationship. It is well known that biopsy features, such as tumor length, the proportion of cancer involvement, number of positive cores, and the proportion of positive cores are predictive parameters of ECE and cancer-related outcomes [18-20]. The histopathological features of prostate cancer grade and extent in needle biopsies have been used to predict cancer grade, tumor volume, and pathological stage in the prostate. The Gleason grade on needle biopsies has been demonstrated to be predictive of stage, and the number of positive cores in the biopsy was the most useful predictor of tumor size [21-23]. Equally, maximum tumor length was the best independent independent predictor of ECE and the number of positive biopsies was the most useful single parameter with a positive predictive value of 83% in 274 lobes and a negative predictive value of 55% [7,13].
Pretreatment PSA, highest biopsy Gleason sum, and percentage of positive biopsy cores for cancer were the three most significant independent predictors of pathologic stage after radical prostatectomy in a recent study [24]. But cancer volume in the prostatectomy specimens was weakly or not correlated with the number of positive biopsies, total length of cancer in biopsies, and the percent of Gleason grade 4/5 on biopsies. Therefore, with these critical parameters from the biopsy specimens, Noguchi et al were unable to estimate cancer volume in the radical prostatectomy specimen on an individual basis [25]. In our data, PSM patients had a higher percentage of positive biopsy cores with no statistical significance.
Generally, PSA is a strong predictor of tumor aggressiveness. Noldus and Stamey reported a strong correlation (r=0.70) between preoperative PSA and the pathologically measured cancer volume. This correlation was not shown when they investigated larger numbers of patients [26]. PSA alone cannot predict the cancer volume reliably. PSA elevation produced by benign prostatic hyperplasia and advancing age decreases the reliability of serum PSA as a predictive parameter for cancer volume [5,6]. In an attempt to improve the ability to predict organ-confined disease, Seaman et al tested the efficacy of PSAD. These investigators found greater accuracy predicting organ-confined disease with PSAD. Patients who have low PSAD values are ideal candidates for radical prostatectomy, and PSAD was a better predictor of final pathologic stage than Gleason score [27]. Taneja et al reported that the AUC for predicting the ECE of prostate tumors was 0.62 and 0.69 for complexed serum PSA and complexed PSAD, respectively [28]. These findings were supported by those of Naya et al who reported an AUC of 0.54 and 0.70 for complexed PSA and complexed PSAD, respectively [29]. Our study showed a better discriminative AUC value of PSAD for ECE (0.765) and for PSM (0.780) than previous reports. These results could be significant because of the narrow spectrum of enrolled patients with PSA less than 10 ng/ml. In general, PSAD is a better predictor of prostate cancer in men with PSA levels of 4-10 ng/ml, especially when ultrasound- determined measurements of prostate volume are available. This suggests that PSAD is a powerful parameter for estimating tumor volume in the gray zone of prostate cancer regardless of patient race or age. Our data showed more accuracy of PSAD in predicting stage, which could be related to the small volume of the Asian race; more international study will be needed [27]. As we know, this is the first study about the relationship between PSM and PSAD. Furthermore, like our result for ECE, Ishida et al reported that the pathological stage was found to be significantly correlated with the MRI findings but not the DRE findings [11].
Accurate cancer staging is critical for selecting the most appropriate treatment option in prostate cancer. Currently available predictive efforts for stage are complicated, so we tried to simplify the related factors. In our study, we were able to show a significant predictive power and cutoff value of PSAD in terms of ECE and PSM compared with PSA. This study had some limitations, including its retrospective manner and lack of data about actual pathologically measured cancer volume. Although no single parameter should be used in clinical practice to increase the ability to predict the presence of unfavorable pathologic outcomes, PSAD can be a useful and very effective predictor of ECE and PSM as a tool to reflect the tumor burden, and we can counsel patients with discretion regarding the likelihood of complete cancer control.
PSAD has relevance to ECE (plus MRI findings) and PSM (plus PSA). Although various clinical factors could significantly increase adequate cancer control, PSAD could be a useful and powerful predictor for ECE and PSM as a preoperative characteristic in radical prostatectomy patients with PSA less than 10 ng/ml. However, our study was conducted in two centers with 94 RALP cases and 27 RRP cases under three surgeons. Thus, larger and single-center studies will be needed.
Figures and Tables
FIG. 1
(A) Receiver operating characteristic (ROC) curves comparing prostate-specific (PSAD, dotted line) and PSA (line) for extracapsular extension. (B) ROC curves comparing PSAD (dotted line) and prostate-specific antigen (PSA, line) for positive surgical margin.

TABLE 2
Uni-variate and multi-variate analysis of clinical and biopsy features for predicting ECE of 121 radical prostatectomy patients
References
1. Hara I, Miyake H, Hara S, Yamanaka N, Ono Y, Eto H, et al. Value of the serum prostate-specific antigen-alpha 1-antichymotrypsin complex and its density as a predictor for the extent of prostate cancer. BJU Int. 2001. 88:53–57.
2. Smith JA Jr, Scardino PT, Resnick MI, Hernandez AD, Rose SC, Egger MJ. Transrectal ultrasound versus digital rectal examination for the staging of carcinoma of the prostate: results of a prospective, multi-institutional trial. J Urol. 1997. 157:902–906.
3. Zheng XY, Xie LP, Wang YY, Ding W, Yang K, Shen HF, et al. The use of prostate specific antigen (PSA) density in detecting prostate cancer in Chinese men with PSA levels of 4-10 ng/mL. J Cancer Res Clin Oncol. 2008. 134:1207–1210.
4. Rietbergen JB, Hoedemaeker RF, Kruger AE, Kirkel WJ, Schröder FH. The changing pattern of prostate cancer at the time of diagnosis: characteristics of screen detected prostate cancer in a population based screening study. J Urol. 1999. 161:1192–1198.
5. Shinohara K, Wolf JS Jr, Narayan P, Carroll PR. Comparison of prostate specific antigen with prostate specific antigen density for 3 clinical applications. J Urol. 1994. 152:120–123.
6. Partin AW, Carter HB, Chan DW, Epstein JI, Oesterling JE, Rock RC, et al. Prostate specific antigen in the staging of localized prostate cancer: influence of tumor differentiation, tumor volume and benign hyperplasia. J Urol. 1990. 143:747–752.
7. Graefen M, Haese A, Pichlmeier U, Hammerer PG, Noldus J, Butz K, et al. A validated strategy for side specific prediction of organ confined prostate cancer: a tool to select for nerve sparing radical prostatectomy. J Urol. 2001. 165:857–863.
8. Ohori M, Kattan MW, Koh H, Maru N, Slawin KM, Shariat S, et al. Predicting the presence and side of extracapsular extension: a nomogram for staging prostate cancer. J Urol. 2004. 171:1844–1849.
9. Choi H, Ko YH, Kang SG, Kang SH, Park HS, Cheon J, et al. Biopsy related prostate status does not affect on the clinicopathological outcome of robotic assisted laparoscopic radical prostatectomy. Cancer Res Treat. 2009. 41:205–210.
10. Gancarczyk KJ, Wu H, McLeod DG, Kane C, Kusuda L, Lance R, et al. Using the percentage of biopsy cores positive for cancer, pretreatment PSA, and highest biopsy Gleason sum to predict pathologic stage after radical prostatectomy: the Center for Prostate Disease Research nomograms. Urology. 2003. 61:589–595.
11. Ishida M, Nakashima J, Hashiguchi A, Mizuno R, Shinoda K, Kikuchi E, et al. Are predictive models for cancer volume clinically useful in localized prostate cancer. Int J Urol. 2009. 16:936–940.
12. Lee JT, Lee S, Yun CJ, Jeon BJ, Kim JM, Ha HK, et al. Prediction of perineural invasion and its prognostic value in patients with prostate cancer. Korean J Urol. 2010. 51:745–751.
13. Nakanishi H, Troncoso P, Babaian RJ. Prediction of extraprostatic extension in men with biopsy Gleason score of 8 or greater. J Urol. 2008. 180:2441–2445.
14. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Schnall M, Tomaszewski JE, et al. A multivariate analysis of clinical and pathological factors that predict for prostate specific antigen failure after radical prostatectomy for prostate cancer. J Urol. 1995. 154:131–138.
15. Mian BM, Troncoso P, Okihara K, Bhadkamkar V, Johnston D, Reyes AO, et al. Outcome of patients with Gleason score 8 or higher prostate cancer following radical prostatectomy alone. J Urol. 2002. 167:1675–1680.
16. Kattan MW, Stapleton AM, Wheeler TM, Scardino PT. Evaluation of a nomogram used to predict the pathologic stage of clinically localized prostate carcinoma. Cancer. 1997. 79:528–537.
17. Partin AW, Kattan MW, Subong EN, Walsh PC, Wojno KJ, Oesterling JE. Combination of prostate specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer. A multi-institutional update. JAMA. 1997. 277:1445–1451.
18. Graefen M, Haese A, Pichlmeier U, Hammerer PG, Noldus J, Butz K, et al. A validated strategy for side specific prediction of organ confined prostate cancer: a tool to select for nerve sparing radical prostatectomy. J Urol. 2001. 165:857–863.
19. Naya Y, Slaton JW, Troncoso P, Okihara K, Babaian RJ. Tumor length and location of cancer on biopsy predict for side specific extraprostatic cancer extension. J Urol. 2004. 171:1093–1097.
20. Tsuzuki T, Hernandez DJ, Aydin H, Trock B, Walsh PC, Epstein JI. Prediction of extraprostatic extension in the neurovascular bundle based on prostate needle biopsy pathology, serum prostate specific antigen and digital rectal examination. J Urol. 2005. 173:450–453.
21. Cookson MS, Fleshner NE, Soloway SM, Fair WR. Correlation between Gleason score of needle biopsy and radical prostatectomy specimen: accuracy and clinical implications. J Urol. 1997. 157:559–562.
22. Wang X, Brannigank RE, Rademaker AW, McVary KT, Oyasu R. One core positive prostate biopsy is a poor predictor of cancer volume in the radical prostatectomy specimen. J Urol. 1997. 158:1431–1435.
23. Cheng L, Slezak J, Bergstralh EJ, Myers RP, Zincke H, Bostwick DG. Preoperative prediction of surgical margin status in patients with prostate cancer treated by radical prostatectomy. J Clin Oncol. 2000. 18:2862–2868.
24. Gancarczyk KJ, Wu H, McLeod DG, Kane C, Kusuda L, Lance R, et al. Using the percentage of biopsy cores positive for cancer, pretreatment PSA, and highest biopsy Gleason sum to predict pathologic stage after radical prostatectomy: the Center for Prostate Disease Research nomograms. Urology. 2003. 61:589–595.
25. Noguchi M, Stamey TA, McNeal JE, Yemoto CM. Relationship between systematic biopsies and histological features of 222 radical prostatectomy specimens: lack of prediction of tumor significance for men with nonpalpable prostate cancer. J Urol. 2001. 166:104–109.
26. Noldus J, Stamey TA. Limitations of serum prostate specific antigen in predicting peripheral and transition zone cancer volumes as measured by correlation coefficients. J Urol. 1996. 155:232–237.
27. Seaman EK, Whang IS, Cooner W, Olsson CA, Benson MC. Predictive value of prostate-specific antigen density for the presence of micrometastatic carcinoma of the prostate. Urology. 1994. 43:645–648.
28. Taneja SS, Hsu EI, Cheli CD, Walden P, Bartsch G, Horninger W, et al. Complexed prostate-specific antigen as a staging tool: results based on a multicenter prospective evaluation of complexed prostate-specific antigen in cancer diagnosis. Urology. 2002. 60:4 Suppl 1. 10–17.
29. Naya Y, Fritsche HA, Cheli CD, Stamey TA, Bartsch G, Brawer MK, et al. Volume indexes of total, free, and complexed prostate- specific antigen enhance prediction of extraprostatic disease extension in men with nonpalpable prostate cancer. Urology. 2003. 62:1058–1062.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download