Abstract
We report a rare case of testicular metastasis from prostate cancer. A 68-year-old patient presented with a right testicular mass with discomfort. He had a history of robot-assisted laparoscopic radical prostatectomy and had received adjuvant radiation therapy and had been treated with androgen deprivation therapy continuously at another institution. We performed a right inguinal orchiectomy. The testicular mass was diagnosed as a metastasis from prostate carcinoma.
Secondary neoplasms of the testis have been reported with an incidence of 0.02% to 2.5% on autopsy [1]. Moreover, prostate cancer metastases to the testis are rare despite the proximity. Testicular metastases generally are painless and are detected incidentally in up to 4% cases after orchiectomy for treatment of advanced prostate cancer [2,3]. This case of testicular metastasis from prostate cancer has been reported rarely in Korea.
A 68-year-old man presented to our outpatient department with discomfort from a palpable mass in his right testis that had persisted for 1 month. The mass was insidious in onset and had increased gradually in size. He had undergone robot-assisted laparoscopic radical prostatectomy (RALP) at another institution in December 2009. The preoperative metastatic evaluation at that time, including a bone scan and computerized tomography (CT) of the abdomen and pelvis, was negative. The pathological report of the surgical specimen revealed cribriform, poorly differentiated ductal adenocarcinoma with a positive surgical margin. The adenocarcinoma had a Gleason score of 9 (4+5) and the pathologic stage was T3. After the RALP, the patient had received adjuvant radiation therapy for 1 month and had been continuously treated with androgen deprivation therapy. The serum prostate-specific antigen (PSA) level of the patient was stable, ranging from 0.04 to 0.07 ng/ml. However, the patient's PSA level had increased to 0.347 ng/ml over the past 3 months.
The scrotum was normal except for a mildly enlarged right testis. The right testicular mass was hard and non-tender. The spermatic cord was also nonspecific. The laboratory examinations showed a normal complete blood count and normal renal and liver functions. Tumor markers for testis tumor were as follows: lactate dehydrogenase 345 U/l, alpha-fetoprotein 2.6 ng/ml, and beta-human chorionic gonadotropin 0.0 mIU/ml. The result of a chest X-ray was normal. Ultrasonographic examination of the scrotum showed a right intratesticular solid mass and an ovoid hyperechoic and slightly heterogeneous mass sized 2.4×1.7×2.0 cm (Fig. 1). The right testis was enlarged to 4.0×2.4×3.0 cm in size. CT of the abdomen and pelvis showed no evidence of local recurrence after radical prostatectomy and no abnormal lymphadenopathy suspicious of primary testicular cancer metastasis.
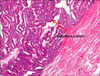
On May 12, 2011, the patient underwent right inguinal orchiectomy. The mass in the right testis measured 2.5×2.5×2.5 cm (Fig. 2). Histopathological examination revealed metastatic cribriform ductal adenocarcinoma of the testis from prostate cancer (Fig. 3). An immunohistochemical prostate acid phosphatase examination of the specimen was performed and revealed diffuse immunoreactions. This proved that there was metastasis from the prostate to the testis.
On May 26, 2011, the patient attended a follow-up examination. His serum PSA level was 0.03 ng/ml and a bone scan showed no metastatic involvement. We are going to continue the androgen deprivation therapy and regular follow-up of the serum PSA level.
Prostate cancer is the most rapidly increasing malignant neoplasm in Korean men. To our knowledge, the most common metastatic sites of prostate cancer are the pelvic lymph nodes, bone, lung, liver, bladder, and brain, but rarely the testis [1,4]. In testicular metastasis of prostate cancer, most patients are asymptomatic and the metastasis is only incidentally found during autopsy or following surgical castration by a bilateral orchiectomy for patients suffering from advanced prostate cancer. The first case of prostate carcinoma metastasizing to the testis was reported by Semans in 1938 [5]. In two autopsy reviews, Dutt et al reported that only 0.02% to -2.5% patients with prostate cancer has testicular metastases [1]. Pienkos and Jablokow examined 24,000 autopsies and reported a 0.06% incidence of testicular metastasis [6]. About 4% of patients with testicular metastases were incidentally diagnosed after a bilateral orchiectomy for surgical castration instead of medical androgen deprivation therapy [7]. In Korea, Kim et al recently presented a report on prostate cancer with solitary metastases to the bilateral testis [8]. Most authors believe that they most frequently originate from malignant lesions of the prostate gland or the lung. The tumor may spread from the prostatic urethra by retrograde venous extension, arterial embolism, or by direct invasion into the lymphatics and lumen of the vas deferens [9,10]. In our case, the route of angiolymphatic extension was suspected in the pathologic findings.
The prognostic significance of testicular metastasis from prostate cancer is still unknown because of the rare occurrence in the testis, especially in patients with a history of advanced prostate cancer. Therefore, it is difficult to assess the value of solitary testicular metastasis as a prognostic indicator. However, we cannot exclude that testicular metastasis is a sign of advanced prostate disease.
In this case, the patient had a palpable testicular mass and we suspected primary testicular cancer concomitant with prostate cancer. However, the mass turned out to be metastasis from the prostate cancer. Thus, if a patient with prostate cancer presents with a testicular mass, we should consider testicular metastasis from prostate cancer as well as primary testicular cancer. In this report, a significant decrease in the PSA level was observed after surgical resection of the testicular metastasis. We have to determine whether such a marked PSA drop has a positive clinical effect on outcome.
Figures and Tables
FIG. 1
Ultrasonography showing an ovoid, hyperechoic and heterogeneous 2.4×1.7×2.0 cm sized intratesticular mass in the right testis.

References
1. Dutt N, Bates AW, Baithun SI. Secondary neoplasms of the male genital tract with different patterns of involvement in adults and children. Histopathology. 2000. 37:323–331.
2. Tu SM, Reyes A, Maa A, Bhowmick D, Pisters LL, Pettaway CA, et al. Prostate carcinoma with testicular or penile metastases. Clinical, pathologic, and immunohistochemical features. Cancer. 2002. 94:2610–2617.
3. Baykal K, Yildirim S, Inal H, Kalci E, Albayrak S, Cingil H, et al. Metastasis of prostate adenocarcinoma to testis. Int J Urol. 1997. 4:104–105.
4. Patel SR, Richardson RL, Kvols L. Metastatic cancer to the testes: a report of 20 cases and review of the literature. J Urol. 1989. 142:1003–1005.
5. Semans JH. Carcinoma of the prostate with metastases to the testes. J Urol. 1938. 40:524.
6. Pienkos EJ, Jablokow VR. Secondary testicular tumors. Cancer. 1972. 30:481–485.
7. Johansson JE, Lannes P. Metastases to the spermatic cord, epididymis and testicles from carcinoma of the prostate--five cases. Scand J Urol Nephrol. 1983. 17:249–251.
8. Kim SO, Choi YD, Jung SI, Oh KJ, Im CM, Kang TW, et al. Prostate cancer with solitary metastases to the bilateral testis. Yonsei Med J. 2011. 52:362–364.
9. Price EB Jr, Mostofi FK. Secondary carcinoma of the testis. Cancer. 1957. 10:592–595.
10. Howard DE, Hicks WK, Scheldrup EW. Carcinoma of the prostate with simultaneous bilateral testicular metastases; case report with special study of routes of metastases. J Urol. 1957. 78:58–64.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download