Abstract
Purpose
The aim of this study was to evaluate whether long-term, postoperative ureteral stenting is necessary after ureteroscopic removal of stones (URS) during an uncomplicated surgical procedure.
Materials and Methods
We prospectively examined 54 patients who underwent URS for lower ureteral stones from February 2010 to October 2010. Inclusion criteria were a stone less than 10 mm in diameter, absence of ureteral stricture, and absence of ureteral injury during surgery. We randomly placed 5 Fr. open-tip ureteral catheters in 26 patients and removed the Foley catheter at postoperative day 1. The remaining 28 patients received double-J stents that were removed at postoperative day 14 by cystoscopy
under local anesthesia. All patients provided visual analogue scale (VAS) pain scores at postoperative days 1, 7, and 14 and completed the storage categories of the International Prostate Symptom Score (IPSS) at postoperative day 7.
Results
The VAS scores were not significantly different on postoperative day 1 but were significantly smaller in the 1-day ureteral catheter group at postoperative days 7 and 14 (p<0.01). All of the storage categories of the IPSS were significantly lower in the 1-day ureteral stent group (p<0.01). The ratio of patients who needed intravenous analgesics because of severe postoperative flank pain was not significantly different between the two groups (p=0.81). No patients experienced severe flank pain after postoperative
day 2, and no patients in either group had any other complications.
Go to : 
The double-J stent was first described by Finney et al in 1978 [1,2]. Since then, ureteral stents have been conventionally placed to reduce the occurrence of colicky pain due to ureteral stricture and the ureteral edema that can occur following ureteroscopic removal of stones (URS) [3, 4]. There are also reports that the placement of an indwelling ureteral stent following URS prevents or reduces the occurrence of ureteral stricture [5]. However, indwelling stents can cause symptoms such as hematuria, dysuria, flank pain, and frequency. In addition, other problems could require a ureteral stent to be removed by use of a cystoscope. With the recent development of a smaller caliber ureteroscope, the occurrence of iatrogenic ureteral injury has decreased and the frequency of ureteral orifice dilation has been reduced. Accordingly, there are also reports of procedures in which ureteral stents are not conventionally placed. In cases with a lack of complications (such as ureteral injury or ureteral orifice stricture), ureteral stones can be safely removed without postoperatively leaving a ureteral stent indwelling following URS. In addition, it has also been reported that postoperative symptoms associated with ureteral stents could be shortened [6]. Djaladat et al equally divided 109 patients who underwent URS into two groups: patients who received a 5 Fr. polyurethane ureteral catheter left indwelling for 24 hours (n=54) and a noncatheterized group (n=55) [7]. They reported that flank pain and renal colic on the first postoperative day were significantly higher in the noncatheterized group. This flank pain and renal colic resulted from early ureteral edema; having a ureteral catheter for the first 24 hours seemed to eliminate the possibility of early ureteral edema, secondary hydronephrosis, and pain. Hosking et al reported that mild flank pain could occur in 57% of patients unless a ureteral stent was left indwelling following URS [6]. Because the pain usually disappears within 48 hours postoperatively, however, the pain might occur temporarily because of ureteral edema. To date, no Korean studies have reported on short-term, indwelling ureteral catheter use following URS for lower ureteral stones.
We conducted this prospective study to assess the efficacy and safety of a 1-day indwelling period of an openended ureteral catheter following URS for lower ureteral stones compared with the long-term indwelling of a conventional type of ureteral catheter.
Go to : 
The present study was conducted in patients who underwent URS for ureteral stones during the period between February and October of 2010 at two hospitals in Korea. Inclusion criteria were 1) lower ureteral stones and 2) at least one stone smaller than 10 mm in diameter. Exclusion criteria included 1) patients who were indicated for shock wave lithotripsy for the presence of renal stones on the ipsilateral side, 2) patients who underwent a ureteral opening dilation for the presence of ureteral opening stricture, and 3) patients who suffered ureteral mucosal injury during the surgery. The locations and sizes of the ureteral stones were assessed by preoperative computerized tomography.
The current prospective study was conducted in 54 patients. Of these patients, 26 were randomly selected by using a random function of Open Office Calc (Open Office. org® version 3.2.0, Oracle Corp., Redwood Shores, CA, USA), and these patients received a 5 Fr. open-ended ureteral catheter that was placed for 1 day following surgery. Then, the catheter was exposed ex vivo and fixed by using a rubber band along with a urethral Foley catheter. The catheter was sealed with a surgical glove and then drained (group 1). In the remaining 28 patients, a 5 Fr. double-J stent was placed for 2 weeks postoperatively (group 2). The length of the double-J stent varied depending on the height of the patient, and it ranged between 22 and 26 cm.
All patients underwent surgery under spinal epidural anesthesia. Surgery was done by using an 8.5-Fr. rigid ureteroscope (Karl Storz®, Tuttlingen, Germany). Ureteral stones were fragmented by using a Holmium:YAG laser with an energy of 3 J (0.6 Hz, 5 W). The excretion of the fragmented ureteral stones was monitored by using a stone basket. In patients who had an indwelling, 5-Fr. openended ureteral catheter, this catheter was removed along with the urethral Foley catheter on postoperative day 1. Patients who had an indwelling, double-J stent also received local anesthesia using 1% lidocaine gel for the urethra during postoperative week 2, and the double-J stent was removed by using a cystoscope.
The operation time of URS was defined as the length of time that elapsed from the time the ureteroscope entered the urethral opening until all the endoscopes were removed. To compare the subjective degree of pain, all patients were asked to complete a visual analogue scale (VAS) pain score on postoperative day 1 and at weeks 1 and 2. In addition, patients who had an indwelling double-J stent were asked to complete a VAS immediately after the removal of the cystoscopic stent. To monitor changes in irritative bladder symptoms due to the use of a double-J stent, all patients completed a questionnaire about storage symptoms on the International Prostate Symptom Score (IPSS) at postoperative week 1. To compare the degree of satisfaction with postoperative outcomes, participants were asked the following question: "Are you willing to undergo the same surgery if you experience ureteral stones again?" on postoperative week 2. Patients responded with either "Yes" or "No."
To quantitatively assess the patients' pain, the severity of pain was graded on an 11-point scale by using the VAS (where 0 points=no pain and 10 points=the most severe pain). Postoperative complications, such as fever and hematuria, were evaluated during the hospitalization period and at postoperative weeks 1 and 2 in an outpatient setting. To unify the type and amount of analgesics administered for patients who complained of flank pain, patients were first given an intravenous injection of tramadol 50 mg. Thereafter, if the pain was persistent, patients received an intravenous injection of pethidine 25 mg. All patients were examined for residual stones by plain X-ray at postoperative day 1 and via intravenous pyelography at 4 weeks postoperatively to identify any occurrence of ureteral stricture. The patients were also asked to visit the outpatient clinic at postope
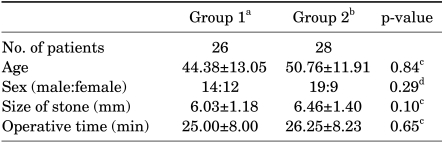
A comparative analysis was performed to evaluate the age, gender, ureteral stone size, and operative time between the two groups by using Student's t-tests and Pearson chisquare tests. We also comparatively analyzed our results to evaluate the severity of pain at postoperative day 1 and weeks 1 and 2, and the scores for each category regarding storage symptoms of the IPSS and total scores at postoperative week 1.
We used Fisher's exact tests and Pearson chi-square tests to compare the number of patients who needed intravenous analgesics due to severe postoperative pain and also to examine the responses to our questionnaire: "Are you willing to undergo the same surgery if you experience ureteral stones again?"
Go to : 
Age, gender, ureteral stone size, and operative time were not significantly different between the two groups (Table 1).
On postoperative day 1, the mean VAS scores for flank pain in group 1 and group 2 were 2.53±1.94 and 3.14±1.84, respectively, which were not significantly different (p=0.55). At postoperative week 1, however, the mean VAS scores for flank pain were 0.19±0.49 in group 1 and 2.60±0.87 in group 2. These scores were significantly different between the groups (p<0.01). Additionally, the mean VAS scores for flank pain at postoperative week 2 were 0.07±0.27 for group 1 and 2.50±1.10 in group 2. This finding was also significantly different between the two groups (p<0.01) (Fig. 1). We calculated the mean VAS to assess the severity of pain during the removal of a cystoscopic ureteral catheter under local anesthesia in group 2, and its mean value was 4.96±1.29. This finding corresponded to a moderate severity of pain.
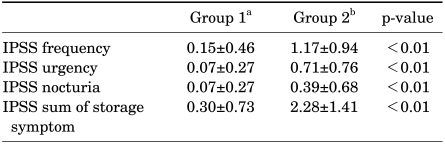
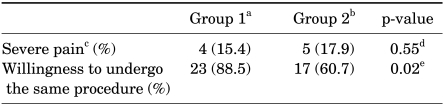
On postoperative week 1, the IPSS values for frequency, urgency, and nocturia were significantly different between group 1 and group 2 (p<0.01) (Table 2). In four group 1 patients, tramadol 50 mg was injected on postoperative day 1 because the patients reported severe pain. Three group 1 patients who experienced persistent pain received an injection of pethidine 25 mg. In group 2, five patients were given tramadol 50 mg injections for severe pain on postoperative day 1. Two additional group 2 patients who had persistent pain received pethidine 25 mg injections. No patients complained of pain with severity so great as to need analgesics after postoperative day 2. In addition, there were no complications such as postoperative fever or severe hematuria. Four patients in group 1 and five patients from group 2 (15.4% and 17.9%, respectively; p=0.81) received postoperative intravenous injections of analgesics (Table 3). No patients in either group had residual stones or ureteral stricture on intravenous pyelography at the 4-week follow-up visit. At postoperative month 3, no patients reported recurring flank pain, and no other complications were observed in either group.
At postoperative week 2, a total of 23 patients in group 1 and 17 patients in group 2 responded that they would undergo the procedure again if necessary. Accordingly, the possibility that surgery could be repeated again with the same methods was 88.5% and 60.7% in the two groups, respectively, with a relatively higher chance in group 1 (p=0.02) (Table 3).
Go to : 
Ureteral stenting is traditionally used to treat uretera l strictures and ureteral obstruction, and it is also frequently recommended to prevent the occurrence of flank pain and ureteral stricture following URS [4, 8, 9]. According to Stoller et al however, ureteral stent-related symptoms, such as flank pain, frequency, urgency, and dysuria, manifest in only 50% of patients who receive an indwelling ureteral stent [8]. In addition, Bregg and Riehle also reported that ureteral catheter-related complications, such as gross hematuria (42%), dysuria (26%), and flank pain (30%), appear before the shock wave lithotripsy in 50 patients with an indwelling ureteral catheter [10]. Pollard and Macfarlane found that ureteral stent-related symptoms appeared in 18 (90%) of 20 patients who had indwelling ureteral stents following URS [11]. Han etal also reported time-dependent changes in symptoms in patients who had received indwelling, double-J ureteral stents [12]. According to these authors, hematuria was the most common symptom (69.5%) of all symptoms evaluated at 1 week after placement of an indwelling ureteral stent, followed by dysuria (45.8%), frequency (42.2%), lower abdominal pain during voiding (32.2%), and flank pain (25.4%). Except for urgency, most of the symptoms showed no significant time-dependent differences until ureteral stent removal.
Additionally, in the current study, patients who had an indwelling double-J stent for 2 weeks following URS experienced a mean VAS score for flank pain of 2.60±0.87 points at postoperative week 1 and 2.5±1.10 points at postoperative week 2. IPSS values for frequency, urgency, and nocturia were relatively higher in patients who had an indwelling double-J ureteral catheter for 2 weeks than they were in those who had an indwelling of an open-ended ureteral catheter for only 1 day. These results suggest that bladder irritation occurred as a result of the presence of the double-J ureteral stent.
Ideally, patients should undergo cystoscopy following placement of an indwelling, double-J ureteral stent and then also after the stent has been removed. However, this procedure is burdensome for patients. According to Hollenbeck et al, because of the additonal mechanical maneuvers required to remove the ureteral stent, patients might suffer injuries to the urinary tract, such as the urethra and bladder [13]. Kim et al evaluated pain that occurred on cystoscopy following an intramuscular injection of diclofenac 90 mg [14]. According to these authors, the mean VAS score during the procedure was 7.8±0.7 points, which indicated severe pain. In addition, only 22.5% of patients responded "Yes" to a questionnaire about their willingness to submit to the same procedure again. In our series,the mean score of the severity of pain was also found to be 4.96±1.29 points during removal of the double-J ureteral stent; this corresponded to a moderate severity of pain.
Controversy exists regarding the necessity of leaving a conventional type of ureteral stent indwelling following URS because of the problems caused by the long-term placement of the stent. Denstedt et al equally divided 58 patients who underwent URS into two groups: a ureteral stent-indwelling group (n=29) and a non-ureteral-stentindwelling group (n=29) [15]. These authors reported that there were no significant differences in complications or the success rates of ureteral stone removal between the two groups. This finding implies that indwelling ureteral stents are not necessary when URS is performed without ureteral opening dilation. Through a systemic review and meta-analysis, Nabi et al compared the outcomes of patients both with and without stenting after uncomplicated ureteroscopy. They concluded that there were no significant differences in postoperative requirements for analgesia, urinary tract infection, the stone-free rate, or ureteric stricture formation [16]. However, Djaladat et al reported that when ureteroscopy was performed without catheterization, flank pain and renal colic can result from early ureteral edema; in this study, having a ureteral catheter for the first 24 h seemed to eliminate the possibility of early ureteral edema, secondary hydronephrosis, and pain [7].
Because of the possibility of flank pain or renal colic, which could arise from early ureteral edema after URS, we did not perform surgery without ureteral stenting.
Four patients (15.4%) in group 1 experienced flank pain of such severity that they required intravenous analgesics. This flank pain was also seen in five patients (17.9%) of group 2. These results indicate that there was no significant difference in the rate of intravenous analgesic use between the two groups. In addition, there were no significant differences in the types and amounts of analgesics used in the current study.
When we asked our patients the following question: "Are you willing to undergo the same surgery if you experience ureteral stones again?", 23 patients in group 1 and 17 patients in group 2 responded "Yes." Thus, the possibility that the same surgical procedure might be performed again was 88.5% and 60.7%, respectively. This implied that patients left with an indwelling ureteral catheter for 1 day following URS had greater compliance than did patients who received conventional double-J ureteral stent placement.
The limitations of the current study are that the sample size was small; the study focused on lower ureteral stones only; the study did not account for the skill of the surgeons; and the study compared only the patients' subjective pain scores.
The current study is significant, however, because no other Korean studies thus far have examined the period of ureteral stenting following URS. Further studies are therefore warranted to examine ureteral stones at various locations in a larger sample of patients.
Go to : 
In patients with lower ureter stones, no ureteral orifice stricture, no need for ureteral balloon dilation, and no mucosal injury during surgery, a 1-day indwelling period for a ureteral catheter following URS may reduce discomfort more than a double-J ureteral stent left indwelling for 2 weeks. In the present study, there were no significant differences in the incidences of postoperative complications between the two groups.
Go to : 
References
1. Finney RP. Experience with new double J ureteral catheter stent. J Urol. 1978; 120:678–681. PMID: 731804.

2. Hepperlen TW, Mardis HK, Kammandel H. Self-retained internal ureteral stents: a new approach. J Urol. 1978; 119:731–734. PMID: 77917.

3. Lee JH, Woo SH, Kim ET, Kim DK, Park J. Comparison of patient satisfaction with treatment outcomes between ureteroscopy and shock wave lithotripsy for proximal ureteral stones. Korean J Urol. 2010; 51:788–793. PMID: 21165201.

4. Harmon WJ, Sershon PD, Blute ML, Patterson DE, Segura JW. Ureteroscopy: current practice and long-term complications. J Urol. 1997; 157:28–32. PMID: 8976208.

5. Boddy SA, Nimmon CC, Jones S, Ramsay JW, Britton KE, Levison DA, et al. Acute ureteric dilatation for ureteroscopy. An experimental study. Br J Urol. 1988; 61:27–31. PMID: 3342296.

6. Hosking DH, McColm SE, Smith WE. Is stenting following ureteroscopy for removal of distal ureteral calculi necessary? J Urol. 1999; 161:48–50. PMID: 10037365.

7. Djaladat H, Tajik P, Payandemehr P, Alehashemi S. Ureteral catheterization in uncomplicated ureterolithotripsy: a randomized,controlled trial. Eur Urol. 2007; 52:836–841. PMID: 17258387.
8. Stoller ML, Wolf JS Jr, Hofmann R, Marc B. Ureteroscopy without routine balloon dilation: an outcome assessment. J Urol. 1992; 147:1238–1242. PMID: 1569657.

9. Netto Junior NR, Claro Jde A, Esteves SC, Andrade EF. Ureteroscopic stone removal in the distal ureter. Why change? J Urol. 1997; 157:2081–2083. PMID: 9146584.
10. Bregg K, Riehle RA Jr. Morbidity associated with indwelling internal ureteral stents after shock wave lithotripsy. J Urol. 1989; 141:510–512. PMID: 2918584.

11. Pollard SG, Macfarlane R. Symptoms arising from Double-J ureteral stents. J Urol. 1988; 139:37–38. PMID: 2961892.

12. Han CH, Ha US, Park DJ, Kim SH, Lee YS, Kang SH. Change of symptom characteristics with time in patients with indwelling double-J ureteral stents. Korean J Urol. 2005; 46:1137–1140.
13. Hollenbeck BK, Schuster TG, Faerber GJ, Wolf JS Jr. Routine placement of ureteral stents is unnecessary after ureteroscopy for urinary calculi. Urology. 2001; 57:639–643. PMID: 11306367.

14. Kim KS, Kim JS, Park SW. study on the effects and safety of propofol anesthesia during cytoscopy. Korean J Urol. 2006; 47:1230–1235.
15. Denstedt JD, Wollin TA, Sofer M, Nott L, Weir M, D'A Honey RJ. A prospective randomized controlled trial comparing nonstented versus stented ureteroscopic lithotripsy. J Urol. 2001; 165:1419–1422. PMID: 11342889.

16. Nabi G, Cook J, N'Dow J, McClinton S. Outcomes of stenting after uncomplicated ureteroscopy: systematic review and meta-analysis. BMJ. 2007; 334:572. PMID: 17311851.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download