Abstract
Purpose
To assess the efficacy of percutaneous unroofing in the treatment of simple renal cysts instead of laparoscopic decortication and open surgeries.
Materials and Methods
From November 2009 to October 2010 at our department, 11 patients with 12 simple cyst units were managed by percutaneous unroofing. All cysts were evaluated with ultrasonography and abdominal computed tomography. If there were no contraindications, cyst wall resection was performed. A standard transurethral resectoscope was used to resect the cyst wall, and the parenchymal portion of the cyst was subsequently cauterized. The drain was left in place for 2 days.
Results
At the 5-month follow-up, patients were asked about their symptoms and ultrasonography was performed. From 12 cyst units, 8 were completely resolved, 3 were reduced to less than 50%, and 1 was persistent to near its original size. Success was defined as a more than 50% reduction in cyst volume.
Conclusions
Simple renal cysts can be safely managed by percutaneous unroofing with a success rate of more than 90%. This technique can offer several advantages over open surgery, such as decreased length of hospital stay, improved convalescence, and reduced risk of complications. Percutaneous resection also avoids the multiple trocar sites, extensive dissection, and technical difficulty associated with laparoscopy.
Go to : 
Renal cysts are common benign lesions of the kidney that are estimated to occur in at least 24% of individuals older than 40 years and 50% of individuals older than 50 years [1]. The incidence of renal cysts is about 10% in the general population, and the prevalence increases with age [2]. With the recent widespread and increased use of abdominal cross-sectional radiographic imaging, the incidence of asymptomatic renal cysts is likely higher than previous estimates. Most renal cysts are simple, asymptomatic, and of unknown etiology. However, some patients develop abdominal or flank pain, hematuria, hypertension, recurrent infection, or obstructive uropathy as a result of a renal cyst [3].
Fortunately, in most patients, for an asymptomatic simple renal cyst, intervention is not necessary unless symptoms or complications develop. Cyst decompression can be
performed by percutaneous aspiration with or without sclerosis, open surgery, antegrade or retrograde endoscopic marsupialization, and laparoscopic decortication. Percutaneous unroofing is a novel technique in the treatment of simple renal cysts.
Go to : 
From November 2009 to October 2010 at our department, 11 patients with 12 simple cyst units were managed by percutaneous unroofing. Indications for intervention included
flank or abdominal pain in 7, recurrent infection in 2, hypertension secondary to cyst compression of the renal parenchyma in 1, and segmental hydronephrosis secondary to cyst encroachment on the renal collecting system in 1.
All cysts were evaluated with ultrasonography and abdominal computed tomography (CT) (Fig. 1). If there were no contraindications, such as risk of malignancy, abscess, pyonephrosis, peripelvic location, or coagulopathy, cyst wall resection was performed. To make the diagnosis of a benign simple cyst on sonography, it should have a sharply defined, thin, distinct, smooth wall; be spherical or oval with no internal echoes; and have good transmission of ultrasound waves with acoustic enhancement behind the cyst (class I in Bosniak classification) [4].
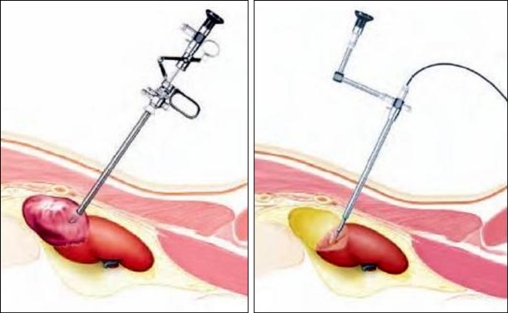
With the patient under general anesthesia and in the prone position, before resection was attempted, the cyst was percutaneously punctured under ultrasonographic guidance from a subcostal approach and aspirated for cytologic examination and creatinine measurement. If the obtained fluid was consistent with a benign cyst and there was no communication with the renal collecting system, a guide wire was placed and the tract was dilated with a metal coaxial dilator up to 30 French adjacent to the exophytic portion of the cyst.
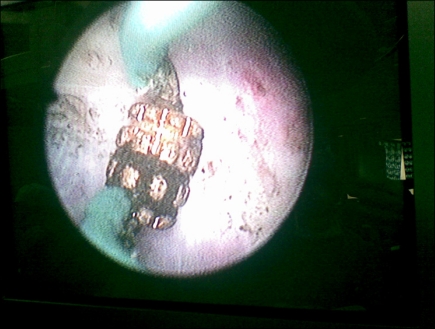
The nephroscope was placed adjacent to the cyst in an extraparenchymal location. A hydro-dissection technique using irrigation fluid (distilled water) was performed to make a proper plane between the extra-parenchymal portion of the cyst wall and the surrounding structures. The nephroscope was then inserted into the exophytic portion of the cyst following the guide wire, and the interior cyst wall was inspected. If there were no abnormalities, a standard transurethral resectoscope was used to resect the exophytic portion of the cyst wall, and the parenchymal portion of the cyst was subsequently cauterized (Figs. 2, 3). A 26-F drainage tube was left in place for 2 days. Patients were discharged on the second postoperative day after the drains were removed.
Go to : 
Of the 11 patients, 8 were male and 3 were female. The patients' mean age was 59 years, ranging from 47 to 78 years. Seven cysts were in the right kidney and 5 were in the left. Three were in the lower pole, 6 were in the mid portion, and 3 were in the upper pole location. The median cyst diameter was 92 mm (range, 65 to 130 mm). All of the cysts were primary, and no therapeutic intervention had been done previously. Preoperative evaluation with ultrasonography and CT categorized all of the cysts in the class I Bosniak classification. The longest operation required 70 minutes and the mean operative time was 45 minutes (Table 1).
There were no major complications such as bleeding, urinary leakage, adjacent organ injury, or parenchymal damage. At the 5-month follow-up, the patients were asked about their symptoms and ultrasonography was performed. Of the 12 cyst units, 8 were completely resolved, 3 were reduced to less than 50%, and 1 was persistent to near its original size. Six of 7 patients with preoperative pain noted significant improvement; the remaining patient had moderate pain. None of the patients had urinary tract infection during the follow-up. The patient who had hypertension did not benefit from surgery, but the upper pole hydronephrosis was resolved in the cyst encroaching on the renal collecting system (Table 2).
Go to : 
The principles of simple renal cyst management are based on eliminating the clinical symptoms and preventing complications such as bleeding, infection, and conditions secondary to cyst encroachment on the renal parenchyma and collecting system.
Open surgical exploration of renal cysts has been reported since the early 1900s. One of the earliest descriptions of open surgical management of renal cysts was performed
by Kretschmer in 1920 [5]. Of 35 patients who were explored through flank or abdominal incisions, 18 underwent resection of a renal cyst, 16 required nephrectomy, and in 1 patient the cyst was marsupialized. Because the surgical treatment of a benign condition such as a renal cyst did not generally require organ extirpation but rather only excision of the cyst wall and evacuation of its fluid contents, less invasive means of treating symptomatic renal cysts that did not require a large flank or abdominal incision were sought. Open renal cyst ablation remained the gold standard approach until the late 1980s, when minimally invasive methods were introduced.
In 1989, Holmberg and Hietala described percutaneous puncture and drainage of peripheral renal cysts under local anesthesia followed by instillation of bismuth-phosphate
sclerosant [6]. Many agents have reportedly been used for this purpose, including glucose, phenol, ethanol, iophendylate, morrhuate sodium, lipidol, povidone-iodine, tetracycline, n-butyl cyanoacrylate, laureth 9 (also called polidocanol), and bismuth phosphate [7,8]. Although short-term success was high, the limitations of this technique included a high cyst recurrence rate (54%) and the risk of collecting system strictures as a result of scarring caused by the sclerosing agent, making this technique ill advised for cysts located in the peripelvic region [9].
Hulbert and coworkers presented the first description of the advantages of laparoscopic decortication of symptomatic renal cysts in 1992 [10]. This technique included the ability to address multiple, peripelvic, and bilateral renal cysts in a single operation by both transperitoneal and retroperitoneal approaches.
Numerous series of laparoscopic ablation of symptomatic simple renal cysts can be found in the literature [11,12]. The mean operative time is 111 minutes (range, 75 to 164 minutes), and the mean length of hospital stay is 3 days. A complication rate of 0% to 20% (mean 3.5%) and a 0% mortality rate in these series compares favorably with a historical series of open renal cyst ablation reporting a complication rate of 37% and mortality rate of 1.6% [13].
Success of laparoscopic renal cyst ablation as defined by relief of symptoms (symptomatic success) averages 97% when comparing all series, with 92% of patients showing no evidence of cyst recurrence on follow-up imaging studies (radiographic success).
Endoscopic retrograde marsupialization for treatment of simple renal cysts with the use of a flexible ureteroscope has been described, but there are many limitations to this
technique. It is technically difficult, is limited to peripelvic cysts, and requires a second procedure for removal of the ureteral stent.
Percutaneous unroofing is another modality under development for the management of symptomatic renal cysts. Gelet and colleagues described six cases of symptomatic benign renal cysts in which a standard transurethral resectoscope was used to resect the cyst wall. At follow-up, 66% of these six patients showed no recurrence on imaging
studies and all were asymptomatic [14]. Plas and Hübner reported a series of 10 patients who underwent long-term follow-up after percutaneous resection. At an average follow-up of 46 months (range, 26-66 months) 50% were cyst-free, 20% showed residual cysts, and 30% had developed a distinct new cyst. All 10 patients were asymptomatic [15].
In our study, 66% of the patients experienced no recurrence, 25% had residual cysts, and in 9% the operation had failed at the 5-month follow-up. All of the patients were symptom free, and the radiologic success was 91% (11 of 12 cysts).
The most commonly applied technique for the treatment of a renal cyst is the multiple-session prolonged ethanol retention technique. Cyst aspiration is an easily performed
procedure. It can be done under local anesthesia on an outpatient basis and has low morbidity. The disadvantages of the multiple-session technique include the following: it is
time-consuming to perform repeated aspiration and injection procedures in each session, and multiple sessions result in additional patient discomfort and inconvenience and an increased risk of ethanol leakage.
With regard to good short-term results, the recurrence rate for large renal cysts is 54% and stricture formation can occur secondary to sclerosing-induced peripelvic fibrosis. The rate of early recurrence of pain is 15%, and 8% of the procedures are complicated by hemorrhage. Ureteral pelvic junction obstruction secondary to stricture formation caused by extravasation of the sclerosing agent has also been reported. Rates of major or minor complications of percutaneous aspiration are reported in up to 1.4% and 10% of cases, respectively.
Laparoscopic unroofing is superior to percutaneous aspiration with sclerotherapy for treating renal cysts. The advantages of the laparoscopic approach are similar to other laparoscopic cases and include minimal postoperative pain and scaring, decreased blood loss, shorter hospital stay, more rapid patient recovery, and shorter time for resumption
of usual activity. The incision is minimal. Bilateral and multiple cysts are treated under a single anesthesia session and both peripheral and peripelvic cysts can be effectively and safely ablated.
Disadvantages to laparoscopic cyst ablation include a longer operative time, the use of expensive equipment, and the requirement for significant technical experience in performing surgery; laparoscopic cyst ablation carries the risks of laparoscopic surgery, including bowl injury and hemorrhage. The incidence of malignancy in radiographically
proven simple renal cysts is less than 0.7%. Therefore, the theoretical risk of tumor seeding is a potential disadvantage of this approach and other minimally invasive procedures for symptomatic renal cysts.
Laparoscopic removal of renal cysts frequently requires three or even more ports. Compared with the simple percutaneous access through one Amplatz sheath, the laparoscopic approach seems to be more invasive if only one peripheral cyst needs treatment. Furthermore, laparoscopic ablation of renal cysts requires equipment and experience that is not available in many urological departments. Percutaneous decortication is performed with the nephroscope and scissors or a resectoscope and loop electrocautery, which are familiar instruments to the urologist. Percutaneous resection also avoids the multiple trocar sites, extensive dissection, and technical difficulty associated with laparoscopy. Disadvantages include the inability to access anteromedial cysts without compromising the renal parenchyma. In addition, as the cyst is resected, the cavity collapses, impairing visualization of the remaining cyst wall, and the irrigant may extravasate and could theoretically cause hyponatremia.
Go to : 
References
1. Laucks SP Jr, McLachlan MS. Aging and simple cysts of the kidney. Br J Radiol. 1981; 54:12–14. PMID: 7448493.

2. McAninch JW. Tanagho EA, Mcaninch JW, editors. Disorders of the Kidneys. Smiths general urology. 2008. 17th ed. New York: Mc Graw Hill;p. 510–511.
3. Amar AD, Das S. Surgical management of benign renal cysts causing obstruction of renal pelvis. Urology. 1984; 24:429–433. PMID: 6495450.

4. Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986; 158:1–10. PMID: 3510019.

6. Holmberg G, Hietala SO. Treatment of simple renal cysts by percutaneous puncture and instillation of bismuth-phosphate. Scand J Urol Nephrol. 1989; 23:207–212. PMID: 2799295.

7. Ohta S, Fujishiro Y, Fuse H. Polidocanol sclerotherapy for simple renal cysts. Urol Int. 1997; 58:145–147. PMID: 9188134.

8. Phelan M, Zajko A, Hrebinko RL. Preliminary results of percutaneous treatment of renal cysts with povidone-iodine sclerosis. Urology. 1999; 53:816–817. PMID: 10197864.

9. Su Li-Ming. Gill IS, editor. laparoscopic renal cyst ablation. Textbook of laparoscopic urology. 2006. 1st ed. New York: Informa Healthcare;p. 259.
10. Hulbert JC, Shepard TG, Evans RM. Laparoscopic surgery for renal cystic disease. J Urol. 1992; 147:882.
11. Rubenstein SC, Hulbert JC, Pharand D, Schuessler WW, Vancaillie TG, Kavoussi LR. Laparoscopic ablation of symptomatic renal cysts. J Urol. 1993; 150:1103–1106. PMID: 8371363.

12. Roberts WW, Bluebond-Langner R, Boyle KE, Jarrett TW, Kavoussi LR. Laparoscopic ablation of symptomatic parenchymal and peripelvic renal cysts. Urology. 2001; 58:165–169. PMID: 11489690.

13. Kropp KA, Grayhack JT, Wendel RM, Dahl DS. Morbidity and mortality of renal exploration for cyst. Surg Gynecol Obstet. 1967; 125:803–806. PMID: 6041724.
14. Gelet A, Sanseverino R, Martin X, Levegue JM, Dubernard JM. Percutaneous treatment of benign renal cysts. Eur Urol. 1990; 18:248–252. PMID: 2289516.

15. Plas EG, Hübner WA. Percutaneous resection of renal cysts: a long-term followup. J Urol. 1993; 149:703–705. PMID: 8455226.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download