This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Traditionally, an interval of 4 to 6 weeks has been recommended after prostate biopsy before open radical prostatectomy. However, such an interval is not explicitly specified in robot-assisted laparoscopic radical prostatectomy (RALP). This study was designed to determine whether the interval from prostate biopsy to RALP affects surgical difficulties.
Materials and Methods
Between January 2008 and May 2009, a total of 237 men underwent
RALP in our institution. The interval from biopsy to RALP was categorized as follows: ≤ 2 weeks, >2 to ≤ 4 weeks, >4 to ≤ 6 weeks, >6 to ≤ 8 weeks, and >8 weeks. Multivariate analysis was used to identify whether the interval from prostate biopsy to RALP was an independent predictor of operative time, estimated blood loss (EBL), margin positivity, continence, and potency.
Results
Among the 5 groups, there were no significant differences in age, body mass index (BMI), preoperative serum prostate-specific antigen (PSA), prostate volume, or preoperative International Index of Erectile Dysfunction-5 score (all p>0.05). In the multivariate analysis, operative time was significantly associated with prostate volume. EBL was associated with prostate volume and BMI. Margin positivity was associated with preoperative serum PSA, prostate volume, and biopsy Gleason score. Postoperative continence and potency were significantly associated with age. However, in univariate and multivariate analyses, the interval from biopsy to RALP was not significantly associated with operative time, EBL, margin positivity, postoperative continence, or potency (all p>0.05).
Conclusions
Our data suggest that the interval from prostate biopsy to RALP is not related to surgical difficulties.
Go to :

Keywords: Prostate biopsy, Prostate neoplasms, Robot-assisted prostatectomy
INTRODUCTION
Prostate cancer is the most prevalent type of cancer in American men. In Korea, its rate of incidence has increased 20 times over the past two decades, which has motivated continuous efforts for the early diagnosis and complete treatment of prostate cancer. Prostate cancer can be cured through radical prostatectomy when the cancer is in the early stage of development and thus confined to the prostate. Radical prostatectomy is currently the most prevalent treatment option for prostate cancer. Prostate cancer is diagnosed through a prostate biopsy. Traditionally, an interval of 4 to 6 weeks has been recommended after transrectal prostate needle biopsy before open radical prostatectomy, because the hematoma or inflammatory reactions caused by the biopsy may interrupt determination of surgical planes during the surgery. This guideline, however, is not explicitly specified in cases of robot-assisted laparoscopic radical prostatectomy (RALP). This study was designed to determine whether the interval from prostate biopsy to RALP affects surgical difficulties.
Go to :

MATERIALS AND METHODS
1. Materials
For this study, 202 patients were selected from a group of 237 patients who underwent RALP from January 2008 to May 2009; patients who underwent hormonal therapy before the surgery, those whose medical records about the time of biopsy were missing, and those who underwent pelvic surgery in the past were excluded. The medical records and pathological reports of the patients were analyzed retrospectively. Postoperative urinary continence and recovery of erectile function were analyzed by using the data for the 68 patients who had been observed for more than 1 year in the follow-up period.
2. Methods
The interval between the prostate biopsy and RALP was categorized into five groups as follows: within 2 weeks (28 patients), 2 to 4 weeks (74 patients), 4 to 6 weeks (59 patients), 6 to 8 weeks (20 patients), and beyond 8 weeks (21 patients). Univariate and multivariate statistical analyses were performed to verify whether the interval between biopsy and surgery had any effect on the duration of surgery, estimated blood loss, positive margin rate, postoperative urinary continence, or recovery of erectile function. We classified our data into two categories; the cutoff points were an operative time of 140 minutes and estimated blood loss of 100 cc, separately. Urinary continence was defined as the cessation of urinary leaks or no use of a pad at 6 months after the surgery, and potency was defined as successful vaginal penetration.
3. Statistical analysis
Statistical analysis was done with SPSS ver. 17 (SPSS Inc., Chicago, IL, USA). Differences in demographics and clinical and pathological factors were examined by using the Kruskal-Wallis test and chi-square test for continuous and categorical variables, respectively. Logistic regression was used for univariate and multivariate analyses. A p-value less than 0.05 was considered to be statistically significant.
Go to :

RESULTS
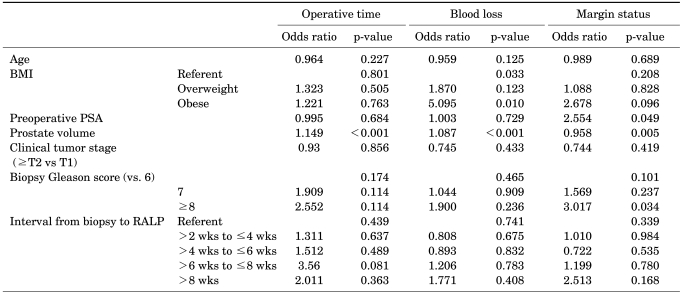
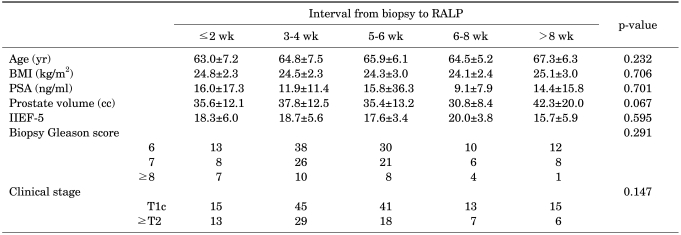
No significant differences were found between the categories in age, body mass index (BMI), preoperative prostate-specific antigen (PSA), prostate volume , preoperative International Index of Erectile Function-5 score, Gleason score, or clinical stage (all p>0.05) (
Table 1) after the transrectal ultrasound biopsy.
TABLE 1
Clinicopathological characteristics classified by interval from biopsy to RALP

Univariate analysis revealed that BMI (p=0.045, p<0.001) and prostate volume (all p<0.001) were associated with operative time and estimated blood loss. Positive margin status was correlated with preoperative PSA (p=0.002), prostate volume (p=0.006), and biopsy Gleason score (p=0.005). Postoperative urinary continence and potency showed statistically significant correlations with age (p=0.027, p=0.002).
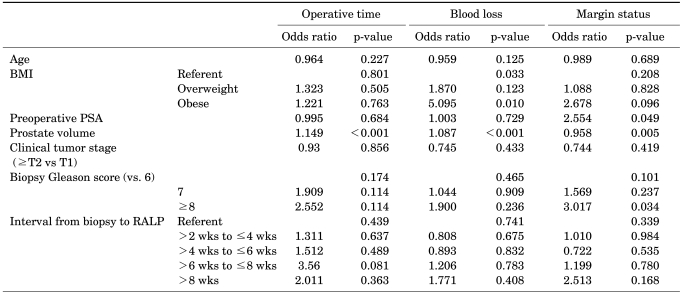
In the multivariate analysis, operative time was significantly associated with prostate volume (p<0.001). Estimated blood loss was associated with prostate volume (p<0.001) and BMI (p=0.033). Margin status was associated with preoperative serum PSA (p=0.049), prostate volume (p=0.005), and biopsy Gleason score (p = 0.034) (See
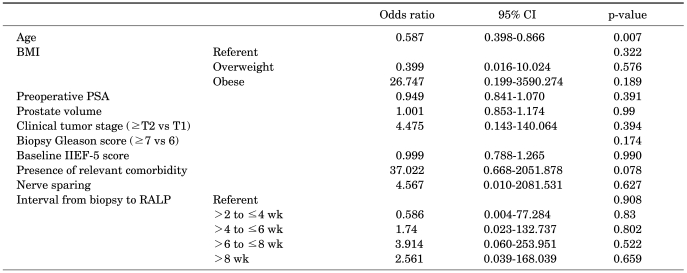
Table 2). Postoperative continence and potency were significantly associated with age (p=0.023, p=0.007) (
Tables 3,
4). Both the univariate and multivariate analyses, however, failed to show that the interval from biopsy to surgery had any significant relations with surgery time, blood loss, positive margin rate, postoperative urinary continence, or potency (all p>0.05).
TABLE 2
Multivariate logistic regression analysis of the predictive factors of operative time, blood loss, and margin status
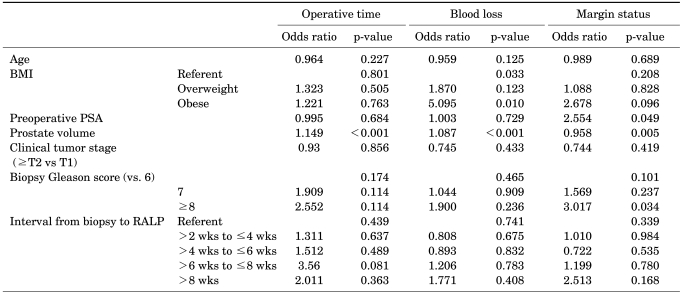

TABLE 3
Multivariate logistic regression analysis of the predictive factors of postoperative continence
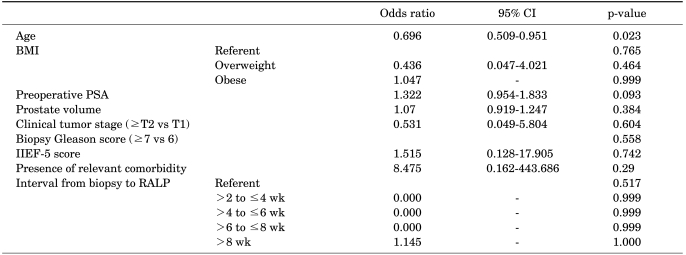

TABLE 4
Multivariate logistic regression analysis of the predictive factors of postoperative potency

Go to :

DISCUSSION
Recently, nearly all prostate cancer cases are diagnosed through a transrectal prostate biopsy. The mean number of removed cores increased from 6.9 to 10.2 in the past decade, and it is highly advised that open radical prostatectomy be executed in about 4 to 6 weeks after a prostate biopsy. This is because the hematoma or inflammatory reactions caused by a biopsy may interrupt the determination of the surgical planes in the prostatectomy [
1,
2]. Transrectal prostate biopsy can cause inflammatory reactions, bleeding, hematoma, and other reactions around the prostate. Ikonen et al reported that a transrectal magnetic resonance imaging executed after a prostate biopsy revealed bleeding in 77% of the patients, and the total bleeding amount evidently decreased only after a lapse of 28 days since the biopsy [
3].
A fair number of studies have been carried out on surgical outcomes compared according to the interval from prostate biopsy to surgery. Among them, Lee et al compared the surgical outcome and the postoperative recovery of erectile function in the category of post-biopsy delay. The outcome of and complications associated with the surgery and postoperative continence had no relation to the interval between biopsy and surgery, but intraoperative blood loss showed significant differences. The authors concluded that a shorter interval between biopsy and surgery makes the remaining inflammatory reactions more severe and thus makes it more difficult to determine the surgical planes for prostatectomy, leading to more bleeding [
4]. In another study, Eggener et al analyzed the postoperative outcome according to the interval from prostate biopsy to open radical prostatectomy. Their univariate analysis demonstrated that blood loss and surgery time increased when the interval between biopsy and surgery was short, but a multivariate analysis did not reveal any significant differences [
5].
On the other hand, few studies have been done on postoperative outcomes according to the interval between prostate biopsy and RALP. Martin et al, after analyzing this issue, reported that RALP executed within 6 weeks after biopsy was associated with significantly more cases of surgery-related complications. They also reported that the RALP caused less blood loss and was less invasive than was open prostatectomy. The interval between biopsy and surgery exerts greater effects on postoperative outcomes because this surgery is carried out on the basis of visual rather than tactile sensations [
6]. By contrast, Menon et al and Tewari et al demonstrated that the visual assistance provided by the 3-D display of the RALP could sufficiently compensate for the lack of the tactile feedback of open prostatectomy [
7,
8]. Similar outcomes were reported by Choi et al [
9]. In that study, the authors concluded that there is no reason to delay RALP to more than 4 weeks after prostate biopsy and that RALP is a feasible procedure regardless of the biopsy-related prostate state.
The present study was carried out with 202 patients who underwent RALP in our institution. Our results suggest that the interval from biopsy to surgery had no significant correlations with surgery time, intraoperative blood loss, positive margin rate, or postoperative continence and potency. These findings are consistent with the results obtained from the above-mentioned studies on postoperative outcomes compared by the interval between prostate biopsy and open radical prostatectomy. These results could be interpreted to mean that the hematoma and inflammatory reactions generated by a prostate biopsy cause no significant differences in the postoperative outcome even though they make it difficult to determine the surgical planes. Many factors such as the operator's experiences and the 3-dimensional visualization of the RALP that compensates for the lack of tactile feedback could explain these insignificant differences. Concerning the operator's experience, Lee et al reported that operation time and estimated blood loss showed a steep learning curve for RALP during the early 24 cases and then stabilized [
10]. To reach more definite conclusions on this issue, more studies are necessary.
In this study, long-term postoperative outcomes such as the rates of biochemical recurrence and tumor-specific survival were excluded. In a few studies, findings were presented on the effects that the interval from biopsy to surgery exerted on outcomes observed in a long-term follow-up period. Several recent studies reported that the risks of biochemical recurrence and elevated Gleason score were not increased even when the interval from biopsy to surgery exceeded 5 months [
11-
13].
The potential limitations of this study should be acknowledged as a means for improvement or for mapping of strategies for further study. Such limitations include the fact that there were only a small number of reported cases, as well as the retrospective nature of the study and the susceptibility to bias inherent in such a design. Moreover, the duration of follow-up was brief for assessing postoperative urinary incontinence and recovery of erectile function. However, in 68 patients who had been observed for more than 1 year, many factors that could influence the functional outcomes were well controlled in our analysis. Thus, it is unlikely that the equivalent results associated with the different intervals from biopsy were an artifact of an imbalance of the predicting factors. Also, it should not be ignored that the potential for selection bias exists because the analysis was based on a group of subjects who underwent surgery by one surgeon at the same institution. Last, the composition of the subject group analyzed in this study differed from those used in other studies. In this study, the majority of the subject group (161 patients out of 202, 79.7%) underwent RALP within 6 weeks after prostate biopsy. This skewness in the sample may be attributed to the short history and limited use of RALP. The biggest reason, however, may be the inclination of the patients to undergo treatment as soon as possible after the diagnosis owing to fear of prostate cancer. In this respect, further studies are recommended with a prospective experimental design and in a larger subject group.
Go to :

CONCLUSIONS
The interval from prostate biopsy to RALP did not show any significant correlations with surgery time, intraoperative blood loss, positive margin rate, or postoperative continence and potency. In this respect, post-biopsy delay until RALP is not estimated to render any effect on the operative difficulties of the surgery.
Go to :