Abstract
Oncocytoma is a neoplasm consisting of oncocytes that is found in the salivary gland, kidney, and thyroid. Adrenocortical oncocytoma is particularly uncommon, and most cases reported are benign and nonfunctioning. Here, we report a 20 cm adrenal mass associated with necrosis that was identified as an oncocytic adrenocortical tumor with uncertain malignant potential through histopathological evaluation after its resection.
Oncocytoma consists of oncocytes, which are acidophilic epithelial cells with mitochondria accumulated in the cytoplasm on electron microscopy [1]. Oncocytoma has been observed in the salivary glands, kidney, and thyroid. Adrenocortical oncocytoma is particularly rare, and the reported cases are usually benign and nonfunctioning. However, there is no single, accurate parameter by which to discriminate between benign and malignant adrenocortical neoplasms. Benign and malignant tumors are classified mainly on the basis of a combination of clinical, biochemical, and histological features [2]. Here we report a case of an oncocytic adrenocortical tumor. Preoperative imaging studies revealed an approximately 20 cm mass associated with necrosis that was considered likely to be malignant cancer. After surgical resection, it was determined to be of uncertain malignant potential.
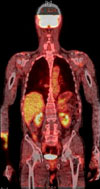
A 69-year-old male with no significant medical history presented to the hospital with abdominal discomfort that had lasted for about 1 month. There were no specific findings on the physical examination except for palpation of the abdominal mass. An 18.2×12.3×16.9 cm mixed solid and cystic mass lesion was observed in the retroperitoneal space on a computed tomography (CT) image of the abdomen and pelvis (Fig. 1A). Open abdominal biopsy of the mass was conducted in the hospital in October 2010 and the mass was identified as an adrenocortical neoplasm, but the adrenal mass could not be differentiated from carcinoma or adenoma. The patient was then referred to our hospital for treatment. Preoperative positron emission tomography-CT (PET-CT) showed a huge, necrotic, suprarenal mass with fludeoxyglucose uptake. No sites of suspected distant metastasis were seen. The patient underwent a left radical adrenalectomy, and the mass showed hypervascularity and severe adhesion to the surrounding tissues. The surgical specimen was 20×18.5×9 cm in size and weighed 1,700 g (Fig. 1B).
Postoperative pathological examination showed necrosis and that less than 25% of the tumor cells were clear cells (Fig. 2A). Immunohistochemical examination showed histone H3 phosphorylation and vimentin positivity (Fig. 2B, C). This case was thus diagnosed as an oncocytic adrenocortical tumor with uncertain malignant potential according to the Weiss system.
The postoperative course showed no specific findings, and the patient was discharged on the 9th day after the operation. A follow-up PET-CT around 3 months after surgery showed no recurrence of the tumor (Fig. 3).
An adrenocortical neoplasm is a common abnormality observed within the adrenal cortex. Most lesions are asymptomatic and are detected incidentally on evaluation for abdominal pain or hypertension [3,4].
Oncocytoma consists of oncocytes, which are acidophilic epithelial cells that show accumulation of mitochondria in the cytoplasm on electron microscopy. Oncocytoma is found mainly in the salivary gland, kidney, and thyroid. Adrenocortical oncocytoma is very uncommon [5]. Peppa et al reported 53 cases of adrenocortical oncocytoma; in that series, the age at diagnosis of adrenocortical oncocytoma ranged from 15 to 77 years and the ratios of males to females and of left to right were 1:2.5 and 3.5:1, respectively [3]. The size and weight of the tumors were 3 to 17 cm and 30 to 1,800 g, respectively. The distribution of benign, borderline, and malignant cases were 28, 14, and 11, respectively. Most adrenocortical oncocytomas observed are benign and nonfunctioning [3,6].
To discriminate between benign and malignant tumors, size and weight have been emphasized as predictors of biological behavior. These are not accurate parameters, however; accordingly, other systems such as the combination of clinical, biochemical, and histological features have been used to distinguish between benign and malignant tumors. In particular, the Weiss system is widely used, which assesses a total of nine histologic features; Fuhrman nuclear grade, mitotic rate >5 per 50 high power field, atypical mitoses, clear cell composition less than 25% of the entire tumor mass, diffuse architecture, necrosis, venous invasion, sinusoidal invasion, and capsular invasion. Cases meeting zero, two, or more of these criteria and the others are classified into benign, malignant, and borderline of uncertain malignant potential, respectively [2,3,7].
In addition, the immunohistochemical and molecular profile is used to investigate the nature of tumors [2]. This profile evaluates immunoreactivity to anti-mitochondrial antibody mES-13, vimentin, inhibin, and melan A. However, its usefulness for diagnosis is limited because of low immunohistochemical sensitivity. Therefore, histological assessment remains important in the diagnosis of adrenocortical neoplasms.
Our case was interesting because malignancy was clinically suspected before the operation, but the mass was found to be an oncocytic adrenocortical tumor with uncertain malignant potential through postoperative histologic assessment. The immunohistochemical findings from preoperative biopsy were as follows: positive for cytokeratin, synaptophysin, inhibin, and melan A. Moreover, because an 18.2×12.3×16.9 cm large, mixed solid and cystic mass associated with necrosis was observed on the abdomen-pelvis CT image, malignancy was clinically suspected.
Oncocytic adrenocortical tumors with uncertain malignant potential are a rare neoplasm and their clinical significance and management are uncertain. Therefore, review of similar borderline tumors is necessary. One such tumor is the prostatic stromal tumor of uncertain malignant potential, or STUMP. Fukuhara et al reported that most STUMPs do not show aggressive behavior but did recur or progress to stromal sarcoma after resection in a few cases [8].
Therefore, an oncocytic adrenocortical tumor with uncertain malignant potential as in this case is considered to require long-term follow-up through clinical, hormonal, and imaging evaluation owing to its malignant potential.
Figures and Tables
FIG. 1
(A) Preoperative computed tomography (CT) findings. The CT image shows a huge, mixed solid and cystic mass lesion in the retroperitoneal space (axial view A-1, coronal view A-2). (B) Gross pathology image of the tumor showing a large, multilobulated, mass-like lesion measuring about 20×18.5×9 cm and weighing 1,700 g.

References
1. Xiao GQ, Pertsemlidis DS, Unger PD. Functioning adrenocortical oncocytoma: a case report and review of the literature. Ann Diagn Pathol. 2005. 9:295–297.
2. Bisceglia M, Ludovico O, Di Mattia A, Ben-Dor D, Sandbank J, Pasquinelli G, et al. Adrenocortical oncocytic tumors: report of 10 cases and review of the literature. Int J Surg Pathol. 2004. 12:231–243.
3. Peppa M, Karamitopoulou E, Nikolopoulos P, Peros G, Economopoulos T, Raptis SA, et al. Large adrenal oncocytoma with uncertain malignant potential: case report and review of literature. Endocr Pract. 2010. 16:641–645.
4. Poretti D, Mazzarol G, Bonomo G, Casadio C, Bellomi M. Adrenocortical oncocytoma: case report. Clin Imaging. 2003. 27:426–430.
5. Ohtake H, Kawamura H, Matsuzaki M, Yokoyama E, Kitajima M, Onizuka S, et al. Oncocytic adrenocortical carcinoma. Ann Diagn Pathol. 2010. 14:204–208.
6. Chang HS, Sohn JC, Park CH, Kim CI, Kwon SY. Adrenocortical Oncocytoma. Korean J Urol. 2007. 48:103–106.
7. Weiss LM. Comparative histologic study of 43 metastasizing and nonmetastasizing adrenocortical tumors. Am J Surg Pathol. 1984. 8:163–169.
8. Fukuhara S, Matsuoka Y, Hanafusa T, Nakayama M, Takayama H, Tsujihata M, et al. A case report of prostatic stromal tumor of uncertain malignant potential (STUMP). Hinyokika Kiyo. 2008. 54:377–381.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download