This article has been corrected. See "Erratum: pT3 Predictive Factors in Patients with a Gleason Score of 6 in Prostate Biopsies" in Volume 52 on page 721.
Abstract
Purpose
Often, a diagnosis of pT3 is made on the basis of radical retropubic prostatectomy specimens, despite a Gleason score of 6 on the preoperative prostate biopsy. Thus, we investigated the preoperative variables in patients displaying these characteristics.
Materials and Methods
Study subjects comprised patients at our institute from 1996 to July 2010 who had exhibited a Gleason score of 6 on their prostate biopsies and had undergone a radical retropubic prostatectomy. Through univariate and multivariate analysis, we investigated pT3 predictive factors including age, preoperative prostate-specific antigen (PSA) levels, transrectal ultrasonography (TRUS)-weighted prostate volume, digital rectal examination findings, bilaterality via prostate biopsy, prostatic cancer in prostate base cores via prostate biopsy, maximum length and percent of prostatic cancer, and number of cores detected in prostatic cancer via prostate biopsy.
Results
In the univariate logistic regression mode, a PSA value of 7.4 ng/ml or higher, TRUS-weighted PSA density of 0.2 ng/ml/cc or higher, prostate cancer detected in the basal core, and prostate cancer detected in 2 or more cores out of 12 were predictive factors for extraprostatic extension. Independent predictive factors for stage pT3 were a PSA of 7.4 ng/ml or higher and prostate cancer detected in 2 or more cores out of 12.
In cases of low-grade prostate cancer with a Gleason score (GS) of 6, extraprostatic extension and metastasis have been shown to be less likely to occur, and such cases generally accompany a good prognosis. Accordingly, such cases have been known to be suitable for radical prostatectomy [1]. In addition, since the application of prostate-specific antigen (PSA) screening to prostate cancer, there have been increasing cases in which early-stage prostate cancer has been cured through surgeries [2]. In prostate cancer, extraprostatic extension has been closely related to prostate biopsy, positive resection margin, and disease-free survival [3-8]. Cases of prostate cancer that turn out to be low grade on biopsy have shown a low incidence rate of extraprostatic extension and thus have usually been completely resected. Moreover, such cases have been reported to have a lower mortality rate related to prostate cancer [4,9,10].
In some studies, the probability of extraprostatic extension was analyzed with the use of standards and nomograms related to the clinical stage, PSA level, and the prostate biopsy [3,6-8]. One study dealt with a high-risk group of extraprostatic extension [5]; however, there have been very few studies focusing on the risk of extraprostatic extension in patients with GS6 prostate cancer.
For GS6 prostate cancer, many surgeons have confidently performed nerve-sparing surgery along with radical prostatectomy. In many cases, however, such procedures cause positive resection margins and thus increase recurrence rates [9].
Ordinarily, a positive resection margin is caused by ill-considered nerve-sparing surgeries [4,5], which have been known to affect progression-free survival [4]. In many studies, it has been reported that the results of preoperative biopsies were not consistent with those of postoperative specimen pathologies in relation to prostate cancer. This study aimed to identify the predictive factors for extraprostatic extension of GS6 prostate cancer in addition to identifying cases suitable for nerve-sparing surgeries.
This study was conducted on 55 patients who had been diagnosed with prostate cancer through prostate biopsy and had undergone radical prostatectomy at our hospital between February 1996 and July 2010. Their GS was 6 and their clinical stages were between T1c and T2N0M0. There were no cases in which neoadjuvant therapy was performed. Their age was calculated on the basis of their hospital registration numbers, and biopsies were performed through transrectal ultrasonography (TRUS) after digital rectal examinations (DREs) and PSA tests. The total prostate volume was calculated through the ellipsoid formula by using an ultrasonograph machine (Type 1202 and 2001; BK-Medical Aps, Denmark). The PSA density (PSAD) was calculated as the ratio of prostate volume to serum PSA (ng/ml/cc). The prostate biopsy was performed with an 18-gauge needle under TRUS. Prostate biopsy-related factors included whether the prostate cancer was bilateral, whether the prostate cancer was detected in the basal core, the maximum length of the tumor, the cancer percentage of the cancer core, and the numbers of cores in which prostate cancer was detected. Clinical factors were limited to age, PSA level measured before the biopsy, prostate volume, findings of the DRE, and how univariate and multivariate analyses were conducted to investigate their influence on extraprostatic extension. The statistical analysis was conducted by using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) utilizing the univariate and multivariate logistic regression models. Statistical significance was defined as p-values less than 0.05.
The median age of the 55 patients was 66 years (range, 51 to 74 years), and their median PSA was 6 ng/ml (range, 3.2 to 46.9 ng/ml). The PSA levels of 4 patients (7.2%) were less than 4 ng/ml, and those of 38 patients were between 4 and 10 ng/ml. TRUS-weighted PSAD averaged 0.3 ng/ml/cc (range, 0.07 to 1.27 ng/ml/cc). The mean prostate volume was 31.8 cc (range, 20 to 65 cc), and the mean specimen weight was 33 g (range, 15.9 to 72.1 g).
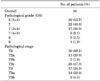
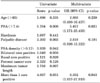
According to the pathological analyses of the prostatectomy specimens, an adverse pathological outcome occurred in 26 patients (47.3%). In the postoperative pathological examinations, the GS was worsened in 26 patients (47.3%). The pathological stages of 38 patients (69.1%) were rated pT2, and those of 17 patients (30.9%) were rated pT3 (Table 1). In the univariate logistic regression model, a PSA of 7.4 ng/ml or more, a TRUS-weighted PSAD of 0.2 ng/ml/cc or more, prostate cancer detected in the basal core, and prostate cancer detected in 2 or more cores out of 12 were the predictive factors for extraprostatic extension. After factors unsuitable for the multivariate logistic regression model were excluded, the results indicated that the independent predictive factors for stage-pT3 were a PSA of 7.4 ng/ml or more and prostate cancer detected in 2 or more cores out of 12 (Table 2).
Pathological upgrading was significantly correlated with the adverse outcome of seminal vesicle involvement, extraprostatic extension, and positive surgical margin. These analyses were composed of cross-tabulations and chi-square (Table 3). In cases in which the GS was increased to 7 or more, extraprostatic extension comprised a high proportion (6.8% vs 57.6%; p<0.001), and a positive surgical margin comprised a higher proportion (20.6% vs 53.8%; p=0.007). When the cutoff value of TRUS-weighted PSAD was adjusted to 0.20 ng/ml/cc, it was possible to predict pT3 prostate cancer with a sensitivity of 92.3% and a specificity of 50%. When the PSA cutoff value was 7.4 ng/ml, sensitivity and specificity were 69.2% and 76.5%, respectively. Table 4 shows cases of upgrading or upstaging in relation to TRUS-weighted PSAD.
The GS of prostatectomy specimens has been known to be a predictive factor for survival [11]. Clinically, the GS directly affects the decision of how to treat prostate cancer given that there is a general belief that biopsy findings correlate with prostatectomy specimens [12]. In previous studies, however, it was reported that 35% to 58.3% of cases showed inconsistency in the GS [13-15]. Also, in this study, 47.3% of cases showed inconsistency of biopsy-based GS with specimen-based scores. In overall cases from this hospital, such inconsistency reached 52.3%. Cupp et al reported pathological factors as the cause of such wide variation [16], and Allan et al and Divrik et al reported that inexperienced clinicians, interobserver variability, needle size, and the frequency of biopsies might also be a cause [17,18]. Further, Cupp et al reported that there was a significant difference between the percentage of biopsy core involvement and the whole mount measured through the serial section performed on the radical prostatectomy specimen [16]. According to the Allan et al report, on a 12-core biopsy, 10% of cases showed upgrading or upstaging of GS6 prostate cancer, and when the number of cores was less than 12, 23% of cases showed this [17]. This finding demonstrates that biopsy pathology-prostatectomy pathology differences become more extensive in smaller amounts of prostate tissue.
Allan et al reported that when GS6 prostate cancer was detected through needle biopsy, approximately 22% of prostatectomy specimens were stage-pT3 or GS7 and higher forms of prostate cancer [17]. In our study, 26 of 55 patients (47.6%) exhibited upgrading, and 17 (30.7%) showed upstaging. Overall, 28 patients (50.9%) showed upstaging or upgrading (Table 1), and GS6 and stage T3 prostate cancer was reported in 2 (3.6%). This implies that there is a limit as to what the biopsy can predict with respect to tumor grade [16,19]. These results were presumed to be caused by the heterogeneous and multifocal characteristics of prostate cancer [12], and pathological upgrading is known to be significantly correlated with adverse pathological outcomes and biochemical recurrence [20]. Thus, from a clinical perspective, the accurate prediction of inconsistency carries important meaning.
Prostate biopsy-related factors were limited to whether prostate cancer was bilateral, whether it was detected in the basal core, the maximum length of the tumor, the percentage of the cancer core, and the numbers of cores in which prostate cancer was detected. Clinical factors were limited to age, PSA, TRUS-weighted PSAD, and findings of the DRE. In many studies, it has been reported that the incidence rate of prostate cancer aggressively increases as men age [21]. In our studies, however, the risk of extraprostatic extension was not higher in older people.
The percentage of cores that turn out to be positive on prostate biopsy is known to be a predictive factor for extraprostatic extension and to significantly affect the prognosis [3,5-8,22,23]. Graefen et al reported that prostate cancer detected in two or more cores made it possible to predict extraprostatic extension [3], and Teneja et al reported that the GS, the number of ipsilateral positive cores, and prostate cancer detected in the fundus were significant predictive factors for extraprostatic extension [7]. It was reported in another study that extraprostatic extension could be predicted through tumor volume [24,25]. In our study, PSA of over 7.4 ng/ml (p=0.006), prostate cancer detected in the basal core (p=0.029), prostate cancer detected in two or more cores out of 12 (p=0.031), and a PSAD of 0.20 ng/ml/cc or more (p=0.042) were univariate predictive factors for extraprostatic extension. In the multivariate analysis, PSA of 7.4 ng/ml or more and prostate cancer detected in two or more cores out of 12 were predictive factors for extraprostatic extension.
Ordinarily, extraprostatic extension of prostate cancer is known to progress posterolaterally. Naya et al conducted a multivariate analysis on 430 subjects (720 lobes) and reported that the risk of extraprostatic extension increased by 10% in cases in which prostate cancer was detected in the basal core and in which the cancer core was 7 mm long or longer [5]. Owing to the directivity of extraprostatic extension, prostate cancer detected in the basal core might be considered to be a significant univariate factor for predicting extraprostatic extension. In this study, the maximum length of the tumor turned out not to be a significant factor, unlike the study of Naya et al [5]. In our study, it was analyzed irrespective of direction, but in the case of Naya et al, it was not certain whether the analyses were conducted with specimens extracted from lateral cores or irrespective of direction [5]. The inconsistency between the two studies is presumed to be related to different methods or different subjects (this study was focused on patients with GS6 prostate cancer). Thus, further study is needed involving a larger number of patients.
Graefen et al and Shah et al reported that PSA was a predictive factor for extraprostatic extension of localized prostate cancer [3,25]; however, Naya et al reported that PSA was not significantly correlated with extraprostatic extension [5]. In the case of PSAD, many studies have reported it to be a predictive factor for the extraprostatic extension of localized prostate cancer as well as a predictive factor for the aggressiveness of tumors [3,26]. However, a few studies have reported that in comparison with PSA, PSAD was not more advantageous in the prediction of extraprostatic extension [27]. In our study, when the cutoff value of PSAD was adjusted to 0.20 ng/ml/cc, it made it possible to predict extraprostatic extension with a sensitivity of 92.3% and a specificity of 50%. With a PSA cutoff value of 7.4 ng/ml, sensitivity and specificity were 69.25% and 76.5%, respectively. The weight of the pathologic specimen was reported to be significantly correlated with TRUS volume [28]. In our study, a linear regression analysis showed that the two variables were correlated with each other (p<0.001).
In many studies, radical prostatectomy has been reported to make it possible to cure localized high-grade prostate cancer completely. In contrast, Manoharan et al reported that the biochemical failure rate reached 38% and that the 10-year disease-free survival rate reached 74% in radical prostatectomy for GS6 and less-localized prostate cancer [10]. In this regard, they reported that biochemical recurrence was closely related to the problem of whether nerve-sparing surgery was performed and whether the resection margin was positive [4,5].
Concerning the limitations of our study, the study was carried out retrospectively, and long-term data could not be gathered. Furthermore, an in-depth investigation was not made into whether prostate cancer was related to the death of patients and whether nerve-sparing surgeries were performed on patients with GS6 prostate cancer. Also, this study did not deal with adverse long-term outcomes or adverse long-term survival outcomes. With respect to radical prostatectomy specimens rated pT3, prostatectomy specimens need to be analyzed for prostate cancer detected in the basal core because extraprostatic extension progresses posterolaterally. In addition, further investigation is needed to examine the influence of nerve-sparing surgery and a positive resection margin on adverse pathological and adverse long-term outcomes.
In relation to clinical factors, the risk of extraprostatic extension became higher with higher PSA (7.4 ng/ml) and when the TRUS-weighted PSAD was 0.2 ng/ml/cc or higher. In relation to biopsy-related factors, it was higher in prostate cancer detected in the basal cores and in prostate cancer detected in two or more cores out of 12. Our results suggest that surgeons need to understand the uncertainty of GS in relation to biopsy. In patients with the previously mentioned risk factors, it is advisable that nerve-sparing surgery not be performed but rather that the patients prepare for the possibility of stage pT3 prostate cancer.
References
1. Partin AW, Lee BR, Carmichael M, Walsh PC, Epstein JI. Radical prostatectomy for high grade disease: a reevaluation 1994. J Urol. 1994. 151:1583–1586.
2. Loeb S, Gonzalez CM, Roehl KA, Han M, Antenor JA, Yap RL, et al. Pathological characteristics of prostate cancer detected through prostate specific antigen based screening. J Urol. 2006. 175:902–906.
3. Graefen M, Haese A, Pichlmeier U, Hammerer PG, Noldus J, Butz K, et al. A validated strategy for side specific prediction of organ confined prostate cancer: a tool to select for nerve sparing radical prostatectomy. J Urol. 2001. 165:857–863.
4. Mian BM, Troncoso P, Okihara K, Bhadkamkar V, Johnston D, Reyes AO, et al. Outcome of patients with Gleason score 8 or higher prostate cancer following radical prostatectomy alone. J Urol. 2002. 167:1675–1680.
5. Naya Y, Slaton JW, Troncoso P, Okihara K, Babaian RJ. Tumor length and location of cancer on biopsy predict for side specific extraprostatic cancer extension. J Urol. 2004. 171:1093–1097.
6. Ohori M, Kattan MW, Koh H, Maru N, Slawin KM, Shariat S, et al. Predicting the presence and side of extracapsular extension: A nomogram for staging prostate cancer. J Urol. 2004. 171:1844–1849.
7. Taneja SS, Penson DF, Epelbaum A, Handler T, Lepor H. Does site specific labeling of sextant biopsy cores predict the site of extracapsular extension in radical prostatectomy surgical specimen. J Urol. 1999. 162:1352–1357.
8. Tsuzuki T, Hernandez DJ, Aydin H, Trock B, Walsh PC, Epstein JI. Prediction of extraprostatic extension in the neurovascular bundle based on prostate needle biopsy pathology, serum prostate specific antigen and digital rectal examination. J Urol. 2005. 173:450–453.
9. Berglund RK, Jones JS, Ulchaker JC, Fergany A, Gill I, Kaouk J, et al. Radical prostatectomy as primary treatment modality for locally advanced prostate cancer: a prospective analysis. Urol. 2006. 67:1253–1256.
10. Manoharan M, Bird VG, Kim SS, Civantos F, Soloway MS. Outcome after radical prostatectomy with a pretreatment prostate biopsy Gleason score of ≥8. BJU Int. 2003. 92:539–544.
11. Kupelian P, Katcher J, Levin H, Zippe C, Klein E. Correlation of clinical and pathologic factors with rising prostate-specific antigen profiles after radical prostatectomy alone for clinically localized prostate cancer. Urol. 1996. 48:249–260.
12. Allsbrook WC Jr, Mangold KA, Johnson MH, Lane RB, Lane CG, Amin MB, et al. Interobserver reproducibility of Gleason grading of prostatic carcinoma: Urologic pathologists. Hum Pathol. 2001. 32:74–80.
13. Cookson MS, Fleshner NE, Soloway SM, Fair WR. Correlation between Gleason score of needle biopsy and radical prostatectomy specimen: accuracy and clinical implications. J Urol. 1997. 157:559–562.
14. Emiliozzi P, Maymone S, Paterno A, Scarpone P, Amini M, Proietti G, et al. Increased accuracy of biopsy Gleason score obtained by extended needle biopsy. J Urol. 2004. 172:2224–2226.
15. San Francisco IF, DeWolf WC, Rosen S, Upton M, Olumi AF. Extended prostate needle biopsy improves concordance of Gleason grading between prostate needle biopsy and radical prostatectomy. J Urol. 2003. 169:136–140.
16. Cupp MR, Bostwick DG, Myers RP, Oesterling JE. The volume of prostate cancer in the biopsy specimen cannot reliably predict the quantity of cancer in the radical prostatectomy specimen on an individual basis. J Urol. 1995. 153:1543–1548.
17. Allan RW, Sanderson H, Epstein JI. Correlation of minute (0.5 mm or less) focus of prostate adenocarcinoma on needle biopsy with radical prostatectomy specimen: role of prostate specific antigen density. J Urol. 2003. 170:370–372.
18. Divrik RT, Eroglu A, Sahin A, Zorlu F, Ozen H. Increasing the number of biopsies increases the concordance of Gleason scores of needle biopsies and prostatectomy specimens. Urol Oncol. 2007. 25:376–382.
19. D'Amico AV, Wu Y, Chen MH, Nash M, Renshaw AA, Richie JP. Pathologic findings and prostate specific antigen outcome after radical prostatectomy for patients diagnosed on the basis of a single microscopic focus of prostate carcinoma with a gleason score ≤7. Cancer. 2000. 89:1810–1817.
20. Freedland SJ, Kane CJ, Amling CL, Aronson WJ, Terris MK, Presti JC Jr. SEARCH Database Study Group. Upgrading and downgrading of prostate needle biopsy specimens: risk factors and clinical implications. Urol. 2007. 69:495–499.
21. Magheli A, Rais-Bahrami S, Humphreys EB, Peck HJ, Trock BJ, Gonzalgo ML. Impact of patient age on biochemical recurrence rates following radical prostatectomy. J Urol. 2007. 178:1933–1937.
22. Ku JH, Moon KC, Kwak C, Kim HH. Significance of predicted tumor volume as a predictor of pathologic stage in patients undergoing radical prostatectomy. Korean J Urol. 2011. 52:24–30.
23. Moon SJ, Park SY, Lee TY. Predictive factors of gleason score upgrading in localized and locally advanced prostate cancer diagnosed by prostate biopsy. Korean J Urol. 2010. 51:677–682.
24. Elliott SP, Shinohara K, Logan SL, Carroll PR. Sextant prostate biopsies predict side and sextant site of extracapsular extension of prostate cancer. J Urol. 2002. 168:105–109.
25. Shah O, Robbins DA, Melamed J, Lepor H. The New York University nerve sparing algorithm decreases the rate of positive surgical margins following radical retropubic prostatectomy. J Urol. 2003. 169:2147–2152.
26. Epstein JI, Chan DW, Sokoll LJ, Walsh PC, Cox JL, Rittenhouse H, et al. Nonpalpable stage T1c prostate cancer: Prediction of insignificant disease using free/total prostate specific antigen levels and needle biopsy findings. J Urol. 1998. 160:2407–2411.
27. Shinohara K, Wolf JS, Narayan P, Carroll PR. Comparison of prostate-specific antigen with prostate-specific antigen density for 3 clinical applications. J Urol. 1994. 152:120–123.
28. Terris MK, Stamey TA. Determination of prostate volume by transrectal ultrasound. J Urol. 1991. 145:984–987.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download