Adrenal myelolipoma is a rare, nonfunctional benign tumor that is composed of mature adipose tissue and hematopoietic elements. The tumor was first described by Gierke in 1905, and the term myelolipoma was coined by Oberling in 1929 [1]. In the past, these tumors were accidentally discovered at autopsy, with an incidence ranging from 0.08% to 0.4% [2]. Today, with the widespread use of noninvasive imaging with ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI), incidental detection of myelolipoma has become more common, constituting up to 10% to 15% of incidental adrenal masses [3]. Most lesions are generally small, unilateral, and asymptomatic; nevertheless, a number of bilateral tumors have been described in the literature [4]. We report here on a case of incidentally found myelolipomas of both adrenal glands.
CASE REPORT
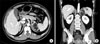
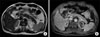
A 48-year-old man was incidentally detected as having a well-defined, heterogeneous enhancing soft tissue density lesion in the bilateral retroperitoneum. The lesions were found during CT while the patient was undergoing evaluation for a gallbladder polyp that was incidentally detected on ultrasonography. The CT showed bilateral masses in the anatomical position of the adrenal glands with densities indicating adipose tissue. The maximum diameter was 8.0 cm for the left mass and 1.8 cm for the right mass. The right adrenal gland was showing but the left was not (Fig. 1). He had a 4-year history of hypertension, for which he was receiving antihypertensive medication. He had no specific symptoms and the results of a physical examination were also nonspecific. The biochemistry profile showed an elevated level of plasma epinephrine of 67.8 pg/ml (range, 1-20 pg/ml), norepinephrine of 340.8 pg/ml (range, 15-80 pg/ml), and ACTH of 158 pg/ml (range, 10-90 pg/ml), and urinary 17-KS of 48.5 mg/day (range, 8-22 mg/day) and 17-OHCS of 55 mg/day (range, 5-23 mg/day). Plasma cortisol, renin, aldosterone, and 24-hour urinary cortisol, free cortisol, metanephrine, vanillylmandelic acid, and homovanillic acid were all within normal limits. In the abdominal MRI, the left tumor measured 8.2 cm and the right tumor measured 2.0 cm in maximum diameter, had high signal intensity on both T1- and T2-weighted images, and low signal intensity on T1 fat-suppressed images and chemical-shift images (Fig. 2). In the (123) I-metaiodobenzylguanidine (MIBG) scan there was no significant uptake region. This suggested the diagnosis of incidental retroperitoneal masses, probably a myelolipoma. A differential diagnosis for malignant tumors was necessary, so the patient was subjected to transperitoneal laparoscopic left adrenalectomy. On macroscopic examination of the surgically removed specimen, the tumor was measured as 9.1×4.9 cm, weighed 128 g, and was yellowish-brown in color. Microscopic examination revealed that the tumor was composed of mature fat mixed with hematopoietic elements including megakaryocytes (Fig. 3). These findings established the diagnosis of adrenal myelolipoma. There was no evidence of malignancy. The patient recovered well without any major complications.
DISCUSSION
Myelolipomas are rare, benign tumors composed of mature adipose tissue and hematopoietic elements. The adrenal gland is the most common site, but myelolipomas are also rarely present in extra-adrenal sites, including the pelvis, mediastinum, retroperitoneum, and paravertebral region, as an isolated soft tissue mass [5]. Adrenal myelolipoma, affecting both sexes in similar rates, usually presents late in adult life, and most cases are diagnosed during the fourth to seventh decade. The association of myelolipoma with obesity, hypertension, chronic disease, and malignancies has been described [3].
Adrenal myelolipomas are in the majority of cases unilateral and often less than 4 cm in diameter. However, they may attain very large sizes and also be bilateral. The term giant myelolipoma is preferred when the size exceeds 8 cm. In the literature, the largest adrenal myelolipoma (diameter 31 cm, weight 6.0 kg) was described by Akamatsu and colleagues [6]. To our knowledge, 10 cases of adrenal myelolipoma were reported in Korea. However, these cases were all unilateral [7]. Therefore, our case is characterized by the presence of bilateral adrenal myelolipomas.
Adrenal myelolipoma, which is usually asymptomatic, is generally diagnosed during surgical interventions and imaging procedures performed for other purposes. Our patient also performed CT for evaluation of a gallbladder polyp that was incidentally detected on ultrasonography. In symptomatic cases, the most common symptom is nonspecific abdominal pain, probably due to hemorrhage, tumor necrosis, or mechanical compression of adjacent organs from large tumor bulk. Also, hematuria and renovascular hypertension were seen. Although rare, surgical emergencies such as a retroperitoneal hemorrhage may be encountered.
Adrenal myelolipomas are generally hormonally inactive, although there are case reports of their association with overproduction of adrenal hormones. They have been associated with overproduction of dehydroepiandrosterone-sulphate (DHEAS), congenital adrenal hyperplasia caused by 21-hydroxylase deficiency, congenital adrenal 17 α-hydroxylase deficiency, Cushing disease, Conn's syndrome, adrenal insufficiency, and pheochromocytoma [8]. Some of these tumors coexist with adrenal adenomas, which may in part account for the hormonal activity. Among them, congenital adrenal hyperplasia and Cushing syndrome appear to be the two most common endocrine disorders described. In our case, the levels of plasma epinephrine, norepinephrine, and ACTH were elevated, but there was no evidence of a functioning pheochromocytoma in the MIBG scan or other hormone-producing tumors in the histopathology. His hypertension remained after the operation, so it was considered essential hypertension.
The pathogenesis of myelolipoma is uncertain, with the prevalent hypothesis suggesting that they arise from the zona fasciculate of the adrenal cortex from metaplasia of undifferentiated stromal cells [3]. More specifically, they are assumed to arise from metaplasia of either previously uncommitted adrenal cortical mesenchymal cells or of groups of choristomatous hematopoietic stem cells that transmigrate during intrauterine life to the developing adrenal gland [9]. Other theories, less favored, propose embolism of bone marrow cells and development from intra-adrenal embryonic rests of bone marrow [9].
Diagnosis of myelolipoma is based on imaging, with ultrasonography, CT, and MRI being effective in more than 90% of cases. The classic myelolipoma is radiolucent on plain films and avascular on angiography. On ultrasonography, a myelolipoma is hyperechoic if it consists mostly of fat and hypoechoic if it is composed primarily of myeloid cells. Usually, the lesion has mixed hyperechoic and hypoechoic areas. CT is the most sensitive imaging modality, and the appearance of myelolipoma depends on its histological composition. Myelolipoma often has a discrete capsule and appears as well-delineated heterogeneous masses with regions of less than -30 Hounsfield units that correspond to low-density mature fat. In MRI, fat tissue has high signal intensity in both T1 and T2 images, whereas myeloid tissue has low signal intensity in T1 and moderate signal intensity in T2 images [10]. Differential diagnosis includes other fat-containing adrenal masses such as teratoma, lipoma, and liposarcoma, which are less common, and even rarely angiomyolipoma, mass-forming extramedullary hematopoiesis, and adenoma. In case a diagnosis has not been established, fine needle aspiration can be helpful to definitively rule out malignancy.
Previously, most patients with myelolipoma underwent surgical resection for a suspected malignant neoplasm. Nowadays, with the frequent detection of these myelolipomas incidentally, the treatment has been a matter of much debate. When the tumor is 4 cm or smaller and asymptomatic, follow-up with CT is recommended. If symptoms occur, surgery should be carried out promptly, especially for a large myelolipoma, because spontaneous rupture of the lesion with hemorrhage is possible. If laparoscopic expertise is available, then the excision is done laparoscopically. Previously, a tumor size exceeding 5 to 6 cm was thought to be a contraindication for the laparoscopic approach. But several recent studies have shown that the laparoscopic approach is technically feasible, safe, and comparable with the open approach in these patients. In the case of bilateral adrenal myelolipomas, a staged tumor removal is preferable, removing the larger one and continuing to observe the contralateral myelolipoma as long as possible in an effort to avoid adrenal insufficiency and a lifetime of steroid replacement [3]. Our patient had bilateral adrenal myelolipomas in which the left tumor was larger than the right, measuring 8.2 cm vs. 2.0 cm in maximum diameter on the MRI. The patient underwent transperitoneal laparoscopic left adrenalectomy. However, if there were bilateral, giant, symptomatic adrenal myelolipomas in a patient with congenital adrenal hyperplasia, bilateral surgical resection should be done.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download