Abstract
Purpose
To analyze the independent effect of metabolic syndrome (MS) on nephrolithiasis (NL) despite differences in gender compared with the known lithogenic factors.
Materials and Methods
From 1995 to 2009, 40,687 Koreans were enrolled in the study and observed for the development of NL at a health promotion center. The examination included anthropometric and biochemical measurements as well as kidney ultrasonography. A student's t-test or chi-square test was used to characterize the participants and a standard Cox proportional hazards model was used to calculate the adjusted odds ratio of lithogenic risk factors in the NL model.
Results
The mean age of the study cohort was 44.9 years (range, 13-100 years), and 22,540 (55.4%) of the cohort was male. The incidence of NL was 1.5% (609 participants), with males exhibiting a higher incidence than females (1.9% vs 1.0%, p<0.01). Among the total cohort, MS as well as each trait of MS were risk factors for NL. In males, high body mass index (BMI), high blood pressure, and abnormal glucose metabolism were significant lithogenic factors, whereas in females, lithogenic factors included only high BMI and abnormal glucose metabolism.
Recent articles from several countries have suggested a worldwide increase in the prevalence of nephrolithiasis (NL) in parallel with the escalating rate of metabolic syndrome (MS) [1-3]. People with MS are known to be at increased risk of diabetes and cardiovascular disease, and in addition to these associations, MS sufferers have recently been identified as being at high risk of chronic kidney diseases [4,5]. Furthermore, some of the traits of MS have been associated with the prevalence of NL [6,7]. Not only in Italy but also in the Republic of Korea, the incidence of NL and MS has increased with improvement in living conditions since the 1970s [8]. Although it has been suggested that this trend is a result of influence of Western lifestyles and dietary habits, it remains unclear as to whether the increased prevalence of NL relative to that of MS is due to such diet and lifestyle modifications.
In Korean people, obesity has been identified as a risk factor for NL or lithogenic factors in a few studies; however, these results either stemmed from hospital populations, not a generalized cohort, or had subjective evidence of NL only [9,10]. Therefore, we investigated the association between NL and MS in a large cohort and a generalized population, as well as the association between NL and MS over a 15-year period to show the real effects of MS on the incidence of NL by using objective evidence from the Korean population.
From 1995 to 2009, we enrolled 40,687 Korean participants from a health promotion center in our hospital. This study was approved by the Institutional Review Board, and the established health examinations included physical examinations, anthropometric measurements, biochemical measurements, and kidney ultrasonography (US). Data were analyzed retrospectively on the basis of information in the patients' medical records.
Weights and heights were measured, and body mass indexes (BMIs, the weight in kilograms divided by the square of the height in meters) were calculated. Systolic and diastolic blood pressure (BP) were measured while the subjects were seated, and fasting venous blood specimens were collected for the measurement of serum levels of glucose, HDL-cholesterol, triglycerides, total calcium, uric acid, phosphate, and creatinine. The estimated glomerular filtration rate (eGFR) was calculated by using the abbreviated equation developed by the Modification of Diet in Renal Disease (MDRD) study: eGFR=186×(serum creatinine level)-1.154×age-0.203 [11]. Ultrasonographic inspection of the renal pelvis and parenchyma in multiple anatomic planes was performed in each subject by using a 3.5-MHz transducer (Voluson 730, General Electronic, Milwaukee, WI, USA). According to Schepens et al renal calcifications were categorized as NL if the calcification was located in the collecting system and as nephrocalcinosis if the calcification occurred within the renal parenchyma [12]. All US evaluations were performed by technicians who were unaware of the patients' metabolic status.
The diagnosis of MS was made according to a recent report by the National Cholesterol Education Program's Third Adult Treatment Panel (NCEP ATP III). It was defined as the presence of three or more of the following metabolic criteria. Elevated BP was defined as a systolic BP≥130 mmHg and/or diastolic BP≥85 mmHg; abnormal glucose metabolism was defined as ≥110 mg/dl; high serum triglyceride level was defined as ≥150 mg/dl; and low HDL cholesterol level was defined as ≤40 mg/dl in men or ≤50 mg/dl in women. Finally, BMI was replaced with waist circumference (WC) in the obese range (>25 kg/m2) by using the standards for Asian populations [13].
SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA), was used for the statistical analysis, considering p-values of less than 0.05 as significant. The results were expressed as mean±standard deviation (SD) or proportion values. Data from participants with MS and those without were compared by using the Student's t-test or chi-square test. The data from participants with NL and those without were also analyzed by using the same methods. We compared not only MS and NL but also a number of MS traits, that is, individual components of MS and NL. To identify the risk factors of NL, the analyzed data were adjusted for multiple covariates. In the multivariate model, we included the following variables that may have confused the relationship between MS and NL: age, gender, GFR, serum uric acid, and phosphorus and calcium levels.
We studied 40,687 participants, including 22,540 (55.4%) men and 18,147 (44.6%) women. The participants' mean age was 44.9±11.5 years (range, 13 to 100 years). General characteristics of the study participants are presented in Table 1. Overall, 7,803 (19.2%) had MS, and 609 (1.5%) had NL. Male participants were older (p<0.01) and had a higher incidence of MS (p<0.01) and NL (p<0.01) than did female participants. Moreover, male participants had a higher incidence of all MS traits than did female participants.
We investigated the difference in clinical and metabolic characteristics according to the echographic evidence of NL in all participants, and these results are presented in Table 2. Among the entire cohort, participants with NL were older than participants without NL and had higher levels of serum uric acid, serum calcium, and serum creatinine as well as lower GFRs than did participants without NL. Furthermore, the incidence of MS was higher in participants with NL, and the incidences of each MS trait other than low serum HDL-cholesterol were higher in participants with NL.
When we divided the participants into genders and compared clinical and metabolic characteristics according to the presence of NL, male and female participants with NL were older, more obese, and showed lower GFRs than did the participants without NL. Moreover, the incidences of MS, high BP, and abnormal glucose metabolism were higher in participants with NL in both males and females. However, the levels of serum uric acid, serum calcium, and serum sodium were not significantly different between the male participants with NL and those without, although differences did exist in female participants.
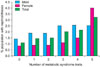
We also assessed whether the relationship between MS and NL was related to the number of MS traits in the total cohort. The prevalence of 0, 1, 2, 3, 4, and 5 traits of MS was 1.12%, 1.45%, 1.51%, 2.04%, 2.16%, and 3.23% in the total population; 1.42%, 1.91%, 1.90%, 2.54%, 2.58%, and 2.55% in males; and 0.85%, 0.90%, 0.90%, 1.13%, 1.51%, and 4.00% in females, respectively. As the number of MS traits increased, the frequency of echographic evidence of NL generally increased in the total cohort and also in male and female participants. In particular, echographic evidence of NL in females increased by almost 3-fold from 4 to 5 traits (1.51% to 4.00%) (Fig. 1).
To identify lithogenic factors, we performed a multivariate logistic regression analysis (Fig. 2). As reported in the figure, this model included the entire study population and confirmed that age (odds ratio [OR]: 1.022; 95% confidence interval [CI]: 1.014-1.029; p<0.05), male gender (OR: 2.030; 95% CI: 1.672-2.465; p<0.05), occurrence of MS (OR: 1.359; 95% CI: 1.128-1.638; p<0.05), and estimated GFR (OR: 0.994; 95% CI: 0.988-0.999; p<0.05) were each significantly and independently related to echographic evidence of NL. With respect to the total sum of MS traits, the results were as follows: one MS trait (OR: 1.173; 95% CI: 0.927-1.485; p<0.05), two MS traits (OR: 1.101; 95% CI: 0.856-1.415; p<0.05), three MS traits (OR: 1.419; 95% CI: 1.085-1.857; p<0.05), four MS traits (OR: 1.520; 95% CI: 1.073-2.152; p<0.05), five MS traits (OR: 2.353; 95% CI: 1.283-4.317; p<0.05). Regarding individual MS traits, high BMI (OR: 1.338; 95% CI: 1.124-1.593; p<0.05), high BP (OR: 1.264; 95% CI: 1.062-1.504; p<0.05), abnormal glucose metabolism (OR: 1.296; 95% CI: 1.028-1.635; p<0.05), high serum triglyceride (OR: 0.887; 95% CI: 0.735-1.072; p<0.05), and low HDL-cholesterol (OR: 0.926; 95% CI: 0.763-1.124; p<0.05) were each significantly and independently related to echographic evidence of NL upon adjustment for multiple covariates including age, GFR, serum uric acid, phosphorus, and calcium level.
A previous study demonstrated an increase in the prevalence and incidence of NL in the United States and other parts of the world. This article showed that diet and climate had the most significant impact on these trends [14]. It has been suggested that climatic factors may be associated with high temperature and low humidity and that dietary factors may be related to increased consumption of starch and fat, thus promoting MS through traits such as obesity, diabetes, and hypercholesterolemia [15,16].
Furthermore, there has been much research regarding the association between MS and NL. West et al reviewed data from 14,670 men and women older than 20 years who participated in the National Health and Nutrition Examination Survey (NHANES III) from 1988 and 1994 [7]. In that study, the presence of MS was associated with a two-fold increase in the OR of self-reported NL (2.13; 95% CI: 1.74 to 2.62) compared with adults without MS, and this OR decreased to 1.52 (95% CI: 1.22 to 1.89) after adjustment for age, sex, and race. In another study, Rendina et al reviewed 2,132 Caucasian inpatients in southern Italy and found that the presence of MS was independently related to echographic evidence of NL and was associated with a two-fold greater frequency of objectively demonstrated NL (OR: 2.01, 95% CI: 1.34 to 3.28) [8]. On the basis of these two studies, it is conceivable that MS is an independent risk factor of NL. In our study, we found a relationship between MS and NL; therefore, our results support the previous conclusions of MS as an independent risk factor for NL.
Insulin resistance (IR), which plays a critical role in the initiation and maintenance of the various clinical features of MS [17], has been identified as a common pathogenic background between MS and NL. It has been suggested that IR may manifest in the kidney as a defect in ammonium production and the ability to excrete acid, thus affecting urine pH [18]. In fact, recent data have confirmed that IR in humans is associated with lower urine pH [19]. Hyperinsulinemia could also lead to decreased urinary citrate and increased urinary excretion of calcium, uric acid, and oxalate, which are important risk factors for calcium and uric acid NL [19,20]. In our study, there was no significant statistical association between the number of traits of MS and the urine pH (data not shown). Probably, this irrelevance was due to the method of collecting the urine. Kamel et al measured the urine pH in 24-hour collected urine [18]; however, we measured the urine pH of a random spot urine sample. In the future, we will analyze 24-hour urine collections for measuring urine pH.
Our study had some limitations. The strengths of our study include the large number of cases and long average length of observation. A corresponding limitation of our study was a lack of exclusion criteria and a lack of patient history about previous NL. This problem could cause certain statistical biases. However, it was practically difficult to collect information about the approximately 40,000 participants. Likewise, the difference between the size of the cohort of each gender could cause a certain statistical bias. The male cohort numbered 22,106 and the female cohort numbered 17,972. Thus, statistical power would have a greater influence in the male cohort than in the female cohort.
Second, we lacked 24-hour urine collections and composition analyses of stones from most of the participants in our study. Thus, we were unable to determine whether MS increased the risk of certain NL types and not others. We also could not ascertain whether differences in urine composition (urinary calcium, phosphate, urate, oxalate, and citrate excretion) were responsible for the effect of the association between MS and NL.
Third, our participants were persons who visited a health promotion center. We can presume that they paid careful attention to their own health and they may have been members of middle-class families. Therefore, we need further large-scale studies in general populations of Koreans to evaluate the effect of MS on the risk of NL.
Fourth, US was used as the imaging modality to assess NL rather than noncontrast computed tomography (CT). The latter is known to be more sensitive for detecting NL and has largely replaced US for the evaluation of patients with symptoms of acute renal colic [21,22]. However, in our study, we used US as part of a comprehensive health examination because US had many advantages, including lack of radiation exposure, wide availability, and low cost despite its lower sensitivity than CT and false-positives. These findings may warrant future prospective studies using imaging modalities with higher sensitivity and less invasiveness.
Finally, we used a modified NCEP ATP III of MS using BMI instead WC. However, a number of studies have shown that BMI should be used instead of WC for predicting the development of type 2 diabetes and other metabolic disturbances, and BMI rather than WC recently was adopted for the analysis of MS [23]. Despite these potential limitations, this is the first study to show the association between MS and incident NL in healthy Korean populations. The strength of this study is the large sample size and objective US evaluation, which allowed us to perform stratified subgroup analysis according to gender over a 15-year period.
Metabolic syndrome is a significant lithogenic factor compared with other lithogenic factors. There was a correlated change in the prevalence of MS and NL and MS traits in Korea.
There was a significantly different gender distribution, and this difference was correlated with the prevalence of MS. There were particular changes in the prevalence of MS and NL and MS traits in Korea. Females exhibited a decreased tendency, whereas males showed an increased tendency, with respect to the prevalence of MS traits. Thus, in Korean men particularly, weight loss and exercise can serve as a protective factor against an increased risk of NL.
Figures and Tables
FIG. 2
Multivariate odds ratio of lithogenic factors for echographic evidence of nephrolithiasis. The sum of metabolic syndrome traits and individual metabolic syndrome traits were adjusted for age, GFR, serum uric acid, and phosphorus and calcium levels. GFR: glomerular filtration rate, MS: metabolic syndrome, BMI: body mass index, OR: odds ratio, CI: confidence interval.

References
1. Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003. 63:1817–1823.
2. Curhan GC. Epidemiology of stone disease. Urol Clin North Am. 2007. 34:287–293.
3. Serio A, Fraioli A. Epidemiology of nephrolithiasis. Nephron. 1999. 81:26–30.
4. Locatelli F, Pozzoni P, Del Vecchio L. Renal manifestations in the metabolic syndrome. J Am Soc Nephrol. 2006. 17:S81–S85.
5. Chen J, Muntner P, Hamm LL, Jones DW, Batuman V, Fonseca V, et al. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med. 2004. 140:167–174.
6. Park HS, Park CY, Oh SW, Yoo HJ. Prevalence of obesity and metabolic syndrome in Korean adults. Obes Rev. 2008. 9:104–107.
7. West B, Luke A, Durazo-Arvizu RA, Cao G, Shoham D, Kramer H. Metabolic syndrome and self-reported history of kidney stones: the national health and nutrition examination survey (NHANES III) 1988-1994. Am J Kidney Dis. 2008. 51:741–747.
8. Rendina D, Mossetti G, De Filippo G, Benvenuto D, Vivona CL, Imbroinise A, et al. Association between metabolic syndrome and nephrolithiasis in an inpatient population in southern Italy: role of gender, hypertension and abdominal obesity. Nephrol Dial Transplant. 2009. 24:900–906.
9. Kim MS, Moon YT. The relationship between obesity and the risk factors of urolithiasis. Korean J Urol. 2007. 48:505–511.
10. Jung TS, Yang WJ, Song YS. The correlation between metabolic syndrome and urinary pH in adult Korean men who visited a health promotion center. Korean J Urol. 2009. 50:694–698.
11. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999. 130:461–470.
12. Schepens D, Verswijvel G, Kuypers D, Vanrenterghem Y. Images in Nephrology. Renal cortical nephrocalcinosis. Nephrol Dial Transplant. 2000. 15:1080–1082.
13. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004. 363:157–163.
14. Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010. 12:e86–e96.
15. Prince CL, Scardino PL. A statistical analysis of ureteral calculi. J Urol. 1960. 83:561–565.
16. Steemburgo T, Dall'Alba V, Gross JL, Azevedo MJ. Dietary factors and metabolic syndrome. Arq Bras Endocrinol Metabol. 2007. 51:1425–1433.
17. Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among u.s. Adults. Diabetes Care. 2004. 27:2444–2449.
18. Kamel KS, Cheema-Dhadli S, Halperin ML. Studies on the pathophysiology of the low urine pH in patients with uric acid stones. Kidney Int. 2002. 61:988–994.
19. Abate N, Chandalia M, Cabo-Chan AV Jr, Moe OW, Sakhaee K. The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance. Kidney Int. 2004. 65:386–392.
20. Siener R, Glatz S, Nicolay C, Hesse A. The role of overweight and obesity in calcium oxalate stone formation. Obes Res. 2004. 12:106–113.
21. Ripollés T, Agramunt M, Errando J, Martínez MJ, Coronel B, Morales M. Suspected ureteral colic: plain film and sonography vs unenhanced helical CT. A prospective study in 66 patients. Eur Radiol. 2004. 14:129–136.
22. Ulusan S, Koc Z, Tokmak N. Accuracy of sonography for detecting renal stone: comparison with CT. J Clin Ultrasound. 2007. 35:256–261.
23. Stevens J, Couper D, Pankow J, Folsom AR, Duncan BB, Nieto FJ, et al. Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obes Res. 2001. 9:696–705.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download