INTRODUCTION
Due to the increased use of imaging modalities, the incidence of incidental renal cell carcinoma has increased [1]. Surgical resection remains the gold standard treatment for renal cell carcinoma but is no longer limited to open radical nephrectomy. Partial nephrectomy has emerged as the standard treatment for small renal tumors, particularly in cases with imperative indications [2]. During the past decade, technical refinements have resulted in laparoscopic partial nephrectomy (LPN) being equivalent to open surgery in terms of oncologic outcomes, perioperative complications, and renal function [3,4].
Transient vascular occlusion is an important surgical step in LPN to facilitate tumor excision and decrease blood loss. Laparoscopic bulldog or Satinsky clamps are tools widely used around the world to achieve renal pedicle clamping. The vessel loop and Hem-o-lok™ clip system (Weck Closure Systems, Research Triangle Pack, NC, USA) has been reported to make it possible to clamp renal vessels transiently during LPN [5,6]. Here we report another feasible technique for achieving transient vascular occlusion by using a vessel loop and Hem-o-lok clips during LPN.
MATERIALS AND METHODS
1. Patient characteristics and methods
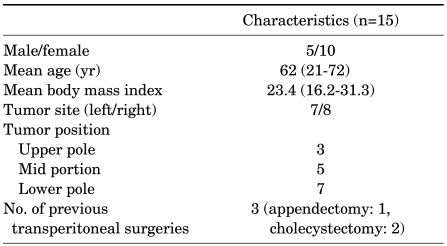
This study was conducted on 15 consecutive patients with renal tumors <4 cm in size who underwent LPN between March 2009 and March 2011 in our hospital. All surgeries were performed by a single surgeon using the transperitoneal approach. The subjects were 5 men and 10 women whose average age was 56 years and average body mass index (BMI) was 23.4; three of the patients had a history of abdominal surgeries. The tumors of seven subjects were in the left kidney, and those of eight subjects were in the right kidney. Regarding tumor location, three were in the upper pole of the kidney, five in the mid portion, and seven in the lower pole (Table 1). No patients had a solitary kidney or multiple renal tumors. Diagnoses were made by using abdominal computed tomography (CT).
The operating time, warm ischemia time, and intraoperative estimated blood loss were recorded for each patient. All patients had their pre- and postoperative serum creatinine and complete blood count. Postoperative tests were done on the 1st, 3rd, and 5th day, respectively, after surgery. A CT scan was done in the third month to detect any recurrence or subclinical complications, such as postoperative hematoma, urinoma, or hydronephrosis.
2. Surgical technique
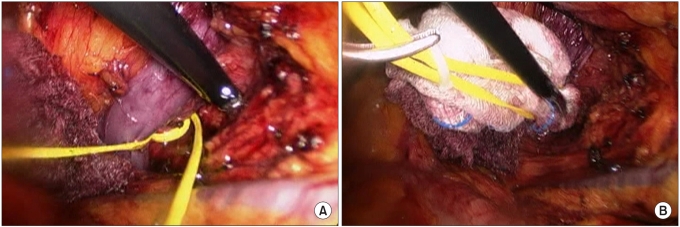
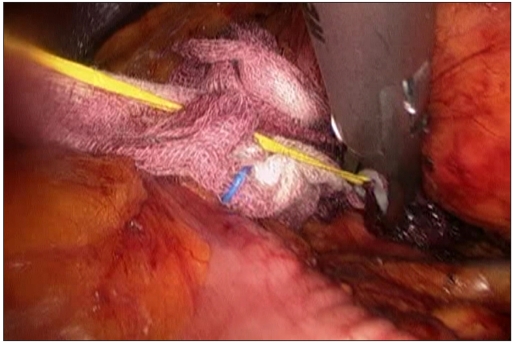
The surgery was performed through the transperitoneal approach. With the patient under general anesthesia, the patient was secured on the operating table in the lateral flank position with the affected side up. In the process of the surgery, four trocars were commonly used (two 10 mm trocars and two 5 mm trocars). We used a closed technique using a Veress needle to obtain the initial access and create pneumoperitoneum, which was typically maintained at 12 mmHg. After the colon was mobilized medially, the renal vessels were dissected. Next, the vessel loop was introduced via a 10 mm trocar and was winded twice around the vessel using a laparoscopic dissector and right-angle. After the vessel had been looped, both free ends of the vessel loop were clipped by a Hem-o-Lok clip so that it would not come untied. Barium gauze was inserted into the outer circle of the vessel loop to avoid vacular injury (Fig. 1). When this step was completed, the preparation for the transient vascular occlusion was finished. Next, the kidney was strategically defatted down to the renal capsule with the laparoscopic monopolar hook, preserving the fat overlying the tumor. The planed line of resection was then scored on the surface of the kidney with the laparoscopic hook. When vascular occlusion was required, the additional Hem-o-lok clip was applied to the proximal portion of the vessel loop pulling the distal portion (Fig. 2). After this simple procedure, the vascular occlusion was done. There was no need for additional ports. In three early cases, both the renal artery and the renal vein were clamped. After that time, only the renal artery was clamped. In situations in which excessive bleeding was encountered during resection of the tumor, the tension could be increased with the application of another Hem-o-lok clip on a more proximal portion of the vessel loop.
After warm ischemia was started, the tumor was excised with a 5 mm safety margin using curved laparoscopic scissors. Electrocautery was not used during resection of the tumor. The collecting system defect was reconstructed with 3-0 Vicryl, if necessary. The renal parenchyma was reconstructed with interrupted sutures with the use of the extracorporeal sliding knot technique using 2-0 Vicryl. When the vascular occlusion was no longer needed, the vessel loop was simply cut. This release of the tension allowed renal blood flow to resume. When the hemostasis was deemed to be adequate, the cellulose mesh (Surgicel®, Ethicon Inc., USA) and fibrin sealant (Tissucol®, Baxter, AG, Austria) were applied on the sutured region. The Gerota's fascia was also closed with interrupted sutures using 2-0 Vicryl. The specimen was entrapped in an endoscopic entrapment bag and extracted intact at the end of the surgery.
RESULTS
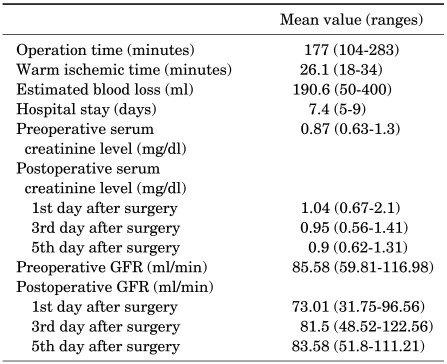
All 15 LPNs were successfully performed without conversion to open surgery. The mean operative time was 177 minutes (range, 104-283 minutes) and the mean warm ischemia time was 26.1 minutes (range, 18-34 minutes). The mean estimated blood loss was 190.6 ml (range, 50-400 ml) and 1 patient was given an intraoperative blood transfusion. The mean duration of postoperative hospitalization was 7.4 days (range, 5-9 days).
The mean baseline serum creatinine level and glomerular filtration rate (GFR) were 0.87 mg/dl (range, 0.63-1.3 mg/dl) and 85.58 ml/min (range, 59.81-116.98 ml/min), respectively. The serum creatinine level was checked at 1, 3, and 5 days after the operation and the GFR was calculated. The mean (range) serum creatinine level and GFR, respectively, were 1.04 mg/dl (0.67-2.1) and 73.01 ml/min (31.75-96.56) at day 1, 0.95 mg/dl (0.56-1.41) and 81.5 ml/min (48.52-122.56) at day 3, and 0.9 mg/dl (0.62-1.31) and 83.58 ml/min (51.8-111.21) at day 5. The serum creatinine level increased at postoperative day 1 and then gradually decreased (Table 2).
The mean tumor size was 2.5 cm (range, 1.5-3.1 cm). Renal cell carcinoma was seen in 8 cases, and all of them were the clear cell type. There was no case of a positive surgical margin. Angiomyolipoma was seen in 7 cases.
All hemostatic procedures were successful in the repair of the vascular and collecting system on the resection bed and renorrhaphy. In the case of intraoperative transfusion, neglect of an accessory vessel caused excessive bleeding, but it was controlled by prompt parenchymal reconstruction without open conversion. There was no uncontrollable intraoperative bleeding and no case of postoperative complications, such as bleeding, urinoma, or hydronephrosis.
DISCUSSION
At first, partial nephrectomy was applied to renal cell carcinoma of a solitary kidney or for bilateral renal cell carcinoma. The range of indicants has recently been enlarged, however, such that partial nephrectomy has been used for patients having normal contralateral kidneys [7-10]. Regarding localized renal cell carcinoma measuring 4 cm and less, partial nephrectomy does not differ from radical nephrectomy in terms of the long-term survival rate; besides, it has been regarded as being useful for preserving renal function [11,12]. In the case of partial nephrectomy, laparoscopic surgery is more effective for patient recovery, to relieve pain, and to shorten the hospitalization time in comparison with laparotomy; moreover, it is less invasive [13-15]. Accordingly, LPN has become the standard treatment for small sized renal cell carcinoma.
The goal of a partial nephrectomy is complete local excision of the tumor with minimal complications and optimal preservation of the renal remnant. Transient vascular occlusion is a crucial process to facilitate tumor excision with a relatively bloodless surgical field to achieve the goals of a partial nephrectomy. In laparoscopic surgery, a bloodless surgical field is even more important for these aims to be achieved without prolonging the warm ischemia time [16]. Relevant devices and instruments should not damage the vascular endothelium and should be easily taken down after the tumor excision and reconstruction of the defect are completed. The laparoscopic bulldog clamp or the Satinsky clamp, i.e., the metallic tools that have traditionally been used for transient vascular occlusion, are apt to damage the vascular endothelium because of their tight clamping [12]. In the case of the laparoscopic bulldog clamp, it may be difficult to apply it precisely and to take it down easily when there is imprecise alignment between the bulldog clamp and its applicator. In the case of the Satinsky clamp, one additional laparoscopic port is needed and kidney mobilization may be limited.
Such problems can be overcome by our technique using the Hem-o-lok clip and the vessel loop. Hem-o-lok clips are common tools used by all laparoscopic surgeons [17]. In the arena of LPN, Canales and associates described their use in the closure of renal parenchymal defects after tumor excision [18]. In our technique, the accessibility of devices and applicators is not a consideration and an additional laparoscopic port is not required. Because the vessel loop is elastic, the risk of mechanical injury to the vascular endothelium is minimal. In addition, vascular occlusion can be easily terminated because the laparoscopic scissors can snip at the vessel loop. Furthermore, our technique benefits from reasonably priced devices. We applied this technique to clamping of both the renal artery and the renal vein successfully, and thus the size and the multiplicity of vessels are not an issue.
Rosales et al and colleagues and Hacker et al and associates performed LPN by applying Rummel's tourniquet technique and reported its usefulness [5,19]. For reference, Rummel's tourniquet technique controls tension by making a once-folded vessel loop pass through a plastic feeding tube. Their method and our technique are similar in tools and mechanism. Although our technique is motivated by them, we simplified the technique and successfully performed operations.
In open partial nephrectomy, Ko and associates reported the efficacy of the parenchymal compression method [20]. They had acceptable outcomes in terms of complete tumor control, avoiding warm ischemic time, and minimizing bleeding, with good preservation of renal function and minimal complications. But this technique cannot be adopted because of the difficulty in the application of instruments in laparoscopic surgery.
The advancement of surgical techniques in laparoscopic and robotic surgery and the introduction of the ultrasonic knife have enabled operators to perform partial nephrectomy without renal artery clamping and to minimize the damage to renal function [21,22]. In the case of surgeries without renal artery clamping, however, operators may experience difficulty in performing the surgeries if they have not overcome the learning curve of laparoscopic or robotic surgeries. Furthermore, application of this technique is limited to patients with an exophytic, small renal tumor.
The greatest advantage of our technique is the simplicity and the ease by which transient vascular clamping is applied and released. This considerably shortened the warm ischemia time despite our limited experience with LPN. Although the cases in this study are all the cases of LPN that we have ever performed, the mean warm ischemia time was 26.1 minutes (range, 18-34 minutes), which is relatively short. Thus, our technique is a useful alternative for less-experienced surgeons as well as for laparoscopic experts.
For investigating precise ischemic renal function, a MAG3 or DTPA renal scan is needed. In our study, the method used to evaluate ischemic renal function was not complete because the serum creatinine level and GFR cannot reflect split renal function. The limitations of our study include the small number of patients, the small number of oncologic events, and that this was a noncomparative study. More cases of renal cell carcinoma and long-term follow-up are needed to determine oncologic results. Clinical comparative studies between the various occlusion devices (laparoscopic bulldog, Satinsky clamps, Rummel's tourniquet, and the vessel loop with Hem-o-lok clips) may show the effectiveness and the merits of each technique.
CONCLUSIONS
Our transient vascular occlusion technique that uses a vessel loop and Hem-o-lok clips was shown to be simple, expeditious, and safe in LPN. Although further comparative studies and long-term data are needed, we suggest that this technique can be a feasible and an acceptable alternative to standard vascular occlusion techniques, such as laparoscopic bulldog or Satinsky clamps, in LPN.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download