Abstract
Purpose
To evaluate the efficacy and tolerability of tamsulosin 0.4 mg once daily in Korean patients with symptomatic benign prostatic hyperplasia (BPH) and investigate whether tamsulosin 0.4 mg can improve symptoms in patients with refractory lower urinary tract symptoms (LUTS) who were previously receiving tamsulosin 0.2 mg once daily.
Materials and Methods
A total of 116 patients from 3 urology centers participated. All study subjects entered a nonblind phase consisting of 8 weeks of tamsulosin 0.2 mg monotherapy followed by an additional 8 weeks of tamsulosin 0.2 mg (0.2 mg group) or 8 weeks of tamsulosin 0.4 mg (0.4 mg group). At week 8, we chose the 0.4 mg group on the basis of International Prostate Symptom Score (IPSS), quality of life (QoL), maximal urinary flow rate (Qmax), and adverse effects. At week 16, we compared the efficacy and tolerability of tamsulosin between the 0.2 and 0.4 mg groups.
Results
A total of 26 patients (22.4%) were escalated to tamsulosin 0.4 mg at week 8. There were significant differences in IPSS, QoL, and Qmax at week 8 in both groups. There were significant differences in improvement in IPSS, QoL, Qmax, and postvoid residual urine volume from baseline to week 16 in both groups. There were no significant differences in efficacy or tolerability between the groups at week 16.
Lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH) are a common condition in older men. In epidemiological community-based surveys, approximately 25% of men aged 40 years and over indicate that they have LUTS [1-3]. Clinical BPH can interfere with daily activities and diminish health-related quality of life specific to urinary symptoms. Treatment options include watchful waiting or lifestyle modification, herbal preparations, prescription medications, and surgical procedures. Medical management of BPH is the first therapeutic option for many patients with symptomatic BPH [3]. The overall goal of the medical management of BPH involves improving short-term symptoms, minimizing adverse effects of treatment, and eventually preventing complications and preserving quality of life. At present, alpha-1-adrenergic receptor antagonists (alpha-blockers) and 5-alpha-reductase inhibitors (5-ARIs) are the only recommended medical treatments for BPH [4,5]. Alpha-blockers improve symptoms and increase the urinary flow rate by relaxing prostatic and bladder neck smooth muscle through sympathetic activity blockade.
Alpha-blockers are the most common prescription medications and include doxazosin, terazosin, prazosin, alfuzosin, and tamsulosin [6,7]. The alpha-1-adrenergic receptor appears to be the subtype mainly mediating prostate and bladder smooth muscle tone. Thus, they improve the dynamic component of bladder outlet obstruction (BOO) and can rapidly relieve LUTS. Unlike the other common alpha-blockers that are not selective for this subtype, such as doxazosin, alfuzosin, and terazosin, tamsulosin has high alpha-1a-adrenergic receptor affinity [7]. Because of this prostate selectivity, tamsulosin may improve urinary symptoms and flow with fewer adverse effects. Many studies have shown the efficacy and tolerability of tamsulosin at doses of 0.2 to 0.8 mg once daily in patients with symptomatic BPH. Seven trials were performed in Asia: 5 in Japan, 1 in China, and 1 in Korea. These studies were trials of tamsulosin 0.2 mg [8-10].
In our trial, we investigated whether tamsulosin 0.4 mg once daily can improve Korean patients with refractory LUTS suggestive of BPH who were previously receiving tamsulosin 0.2 mg once daily. Also, we investigated whether when making treatment decisions for Korean patients with symptomatic BPH, who are receiving tamsulosin 0.2 mg or 0.4 mg, we should incorporate evidence on convenience and dose-related efficacy versus adverse effects.
This study was a nonblinded, open-label, multicenter, prospective trial. From September 2009 to September 2010, a total of 133 patients from the outpatient clinics of three centers participated in this trial. In total, 116 patients were evaluated who were diagnosed as having symptomatic BPH and could be serially followed by our clinical trials. No patients had any life-threatening conditions such as acute cardiovascular disease, neurologic disease, or uncontrolled hypertension or diabetes mellitus. All patients consented to the purpose of the study and to the study itself after explanation. Informed consent was obtained from each subject, and the study was approved by the Institutional Review Board of each center.
On the patients' first visit to the outpatient clinics, blood samples were taken from all patients for measurement of serum prostate-specific antigen (PSA) including serum chemical battery, and the International Prostate Symptom Score (IPSS), transrectal ultrasonography (TRUS), and uroflowmetry were completed for all patients. Also, blood pressure and pulse rate were checked, and a digital rectal examination and routine physical examination were performed.
All patients with BPH eligible for treatment with tamsulosin were indicated in the locally approved prescribing information. The decision to enter the patient into the study must have been made after the clinical decision on the basis of the following inclusion criteria: patient's age ≥50 years, good overall mental and physical health, IPSS ≥8 and maximal urinary flow rate (Qmax) ≤12 ml/s, and prostate volume ≤40 ml as determined by TRUS.
Excluded were patients aged less than 50 years; patients judged to be inappropriate for a clinical trial; patients with urinary tract infection, urethral stricture, or neurogenic bladder; patients diagnosed with or thought to have prostate or bladder cancer; and patients with a history of any urethral or prostate operation.
All study subjects entered a nonblinded phase consisting of 8 weeks of tamsulosin 0.2 mg once daily monotherapy followed by an additional 8 weeks of tamsulosin 0.2 mg (maintenance therapy) monotherapy or 8 weeks of tamsulosin 0.4 mg once daily (dose-escalating therapy) monotherapy. At week 8, we estimated the efficacy and tolerability of tamsulosin 0.2 mg monotherapy according to the clinical presentation of BPH. We then chose the tamsulosin 0.4 mg group on the basis of the following criteria: improvement of IPSS <20% or improvement of Qmax <20% or aggravation of IPSS/quality of life (QoL) or development of clinically significant complications (Fig. 1). At week 16, we compared the improvement in the efficacy variables between the 0.2 mg group (tamsulosin 0.2 mg once daily for 16 weeks) and the 0.4 mg group (tamsulosin 0.2 mg once daily for 8 weeks+tamsulosin 0.4 mg once daily for an additional 8 weeks). In addition to these variables, the safety and tolerability of the treatment arms were evaluated by monitoring IPSS, QoL, Qmax, adverse events, clinical laboratory tests, and routine physical examinations. All statistical analyses were performed by using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA), and p<0.05 was considered statistically significant (unpaired t-test, paired t-test, Fisher's exact test).
Of the 116 patients who were evaluated for this study, a total of 26 patients (26/116, 22.4%) were escalated to tamsulosin 0.4 mg. The patients' mean age was 62.1±4.9 years, their mean body mass index (BMI) was 24.1±5.6 kg/m2, their mean initial serum PSA was 2.5±2.1 ng/ml, and their mean prostate volume was 27.4±12.7 ml. There were no significant differences in mean age, BMI, initial serum PSA, or prostate volume between the tamsulosin 0.2 mg group and the 0.4 mg group (Table 1). The follow-up period for all patients was 16 weeks (Fig. 1).
The mean IPSS of the 0.2 mg group at baseline, 8, 12 and 16 weeks was 23.8±7.0, 17.1±3.7, 17.0±4.4, and 16.8±4.5, respectively, and the mean IPSS of the 0.4 mg group at baseline, 8, 12, and 16 weeks was 22.4±5.3, 21.9±3.7, 17.8±3.2, and 17.4±3.4, respectively (Table 2). There were significant differences between the two groups in the IPSS and the mean change in the IPSS from baseline at week 8 (p<0.001) (Table 2, 3). In both groups, there were significant differences between the IPSS at baseline and that at week 16 (p<0.001) (Fig. 2, 3). At week 16, the mean change in the IPSS from baseline was -7.0±6.2 and -5.1±5.2 in the 0.2 and 0.4 mg groups, respectively, and there were no significant differences in the mean change in the IPSS between the two groups (p=0.164) (Table 3).
The mean QoL of the 0.2 mg group at baseline, 8, 12, and 16 weeks was 5.0±0.9, 3.6±0.7, 3.5±0.6 and 3.3±0.7, respectively, and the mean QoL of the 0.4 mg group at baseline, 8, 12, and 16 weeks was 5.3±0.6, 5.0±0.6, 4.2±0.4, and 3.5±0.8, respectively (Table 2). There were significant differences between the two groups in QoL and the mean change in QoL from baseline at week 8 (p<0.001) (Table 2,3). In both groups, there were significant differences between the QoL at baseline and that at week 16 (p<0.001). At week 16, the mean change in the QoL from baseline was -1.7±1.2 and -1.8±1.0 in the 0.2 and 0.4 mg groups, respectively, and there were no significant differences between the two groups (p=0.827) (Table 3).
The mean Qmax of the 0.2 mg group at baseline, 8, 12, and 16 weeks was 7.9±2.6, 10.6±2.1, 11.1±2.7, and 12.8±2.0, respectively, and the mean Qmax of the 0.4 mg group at baseline, 8, 12, and 16 weeks was 7.4±1.9, 8.3±2.1, 11.1±2.1, and 12.6±2.4, respectively (Table 2). There were significant differences between the two groups in Qmax and mean change in Qmax from baseline at week 8 (p<0.001) (Table 2, 3). In both groups, there were significant differences between the Qmax at baseline and that at week 16 (p<0.001). At week 16, the mean change in Qmax from baseline was 4.9±3.4 and 5.2±3.5 in the 0.2 and 0.4 mg groups, respectively, and there were no significant differences between the two groups (p=0.752) (Table 3).
The mean postvoid residual urine volume (PVR) of the 0.2 mg group at baseline, 8, 12, and 16 weeks was 20.8±21.3, 16.0±22.8, 15.8±20.0, and 13.5±17.7, respectively, and the mean PVR of the 0.4 mg group at baseline, 8, 12, and 16 weeks was 19.6±21.3, 15.2±17.6, 15.4±22.1, and 12.7±20.5, respectively (Table 2). There were no significant differences between the two groups in PVR at any week (Table 2). In the 0.2 and 0.4 mg groups, there were significant differences between the PVR at baseline and that at week 16 (p<0.001, p=0.028 respectively). At week 16, the mean change in the PVR from baseline was -7.4±16.4 and -6.9±15.2 in the 0.2 and 0.4 mg groups, respectively, and there were no significant differences between the two groups (p=0.897) (Table 3).
Reported side effects were rhinitis, rash, abnormal ejaculation, headache, and dizziness, and a total of 15 patients (12.9%) experienced these side effects. Ten patients in the 0.2 mg group (11.1%) and 5 patients in the 0.4 mg group (19.2%) complained of side effects, but there were no significant differences between the groups (p=0.321) (Table 4).
Complications such as acute urinary retention, bladder stone, urinary tract infection, and renal failure are the most common cause of the surgical management of BPH [11,12]. However, the expenses and complications associated with the surgical treatment of BPH have led to the search for effective and safe medical therapies [13]. The efficacy and tolerability of alpha-1-adrenergic receptor antagonists are of great interest in the treatment of BPH [14]. Pharmacologic and molecular studies have shown that the tension of prostatic smooth muscle is mediated by the alpha-1 subtype receptor and that this subtype is predominant in prostatic stroma [15]. To reduce the adverse effects of alpha blockers, many clinical trials have been undertaken to selectively target this receptor type. Of the recently available alpha-blockers (terazosin, doxazosin, alfuzosin, and tamsulosin), tamsulosin has the most favorable tolerability, efficacy, and safety, and tamsulosin is the most widely used medicine in clinical practice [16]. Tamsulosin, which is a third-generation alpha-1-adrenergic receptor antagonist, is the only agent able to discriminate between receptor subtypes [17]. Therefore, tamsulosin may represent a good therapeutic alternative to open prostatectomy or transurethral resection of the prostate in the absence of absolute indications for surgical treatment [17]. Also, tamsulosin has only a negligible effect on blood pressure that does not appear to be clinically relevant, and it can be safely administered in combination with cardiovascular drugs [18,19].
Many long-term, placebo-controlled, double-blind studies evaluating tamsulosin in BPH have been carried out in Western countries. In Asian countries including Japan and Korea, however, there have been few studies about the efficacy and tolerability of tamsulosin, and all studies were trials of tamsulosin 0.2 mg. Therefore, we became interested in the efficacy of tamsulosin 0.4 mg in Korean men. Normally, 4 weeks of treatment with tamsulosin is enough to improve symptoms [20]. The 2002 Expertise Meeting in Urology (EMU) study confirmed that 8 weeks of tamsulosin treatment showed efficacy in comparison with a nontreatment group. On the basis of these facts, the patients in this study were given 8 weeks of tamsulosin 0.2 mg before the assessment of efficacy to determine the 0.4 mg group at week 8. Many articles have used the primary criterion of improvement in urinary symptoms on the basis of improvement in the IPSS of more than 4 scores or 20% to 25%. Accordingly, we defined 'refractory LUTS' as improvement in the IPSS or Qmax of less than 20%.
To determine the efficacy and safety of tamsulosin for the medical treatment of BPH, numerous studies with doses of 0.2, 0.4, 0.6, and 0.8 mg have been done. The initial study by Abrams and associates was undertaken to help to establish the efficacy and safety of tamsulosin, as well as to determine the optimum dosage for treatment [21]. Patients were randomly assigned to placebo, 0.2, 0.4, or 0.6 mg of tamsulosin once daily for 1 month. The greatest reduction in symptoms occurred in those taking either 0.4 or 0.6 mg compared with 0.2 mg and placebo [21]. The two highest doses also provided the greatest improvement in Qmax compared with placebo. There were no dose-related changes in vital signs or laboratory variables [21].
Our study also showed that increasing the dosage improved some of the test results, but the improvements were not as great as in the other studies mentioned above. We believe that these differences were because of the study design and group selection bias. We only increased the dosage of tamsulosin in patients who were refractory to low-dose tamsulosin. If initially we gave tamsulosin 0.4 mg to the patients who were not refractory to tamsulosin 0.2 mg once daily, we would have gotten more positive results.
The most commonly reported adverse events that occur more frequently than with placebo are dizziness, rhinitis, and abnormal ejaculation. Asian men, especially Korean, Japanese, and Chinese men, are believed to have smaller BMIs than white men and accordingly increasing the dose of tamsulosin should result in more adverse effects than in white men. In our study, however, escalating the dose to 0.4 mg improved the symptoms of BPH and the adverse effects were similar to those with 0.2 mg. These encouraging results suggest that it is safe and feasible to titrate the dosage of tamsulosin according to the severity of the patients' symptoms without increasing the incidence of adverse effects.
As far as we know, our study is the first prospective clinical trial of the efficacy and tolerability of tamsulosin 0.4 mg once daily in Korea. We demonstrated that tamsulosin 0.4 mg has greater efficacy than tamsulosin 0.2 mg once daily in patients refractory to treatment with 0.2 mg and that the side effects appear to be similar to those with tamsulosin 0.2 mg.
Although our study was prospective, the double-dose group was too small in number (n=26). Accordingly, our study had limitations in analyzing the tolerability of the double-dose group. However, this is the initial study of tamsulosin 0.4 mg in Korea and the results are still preliminary. Long-term study will be carried out, which will give us more accurate data about the efficacy and tolerability of tamsulosin 0.4 mg.
Treating Korean patients with symptomatic BPH with tamsulosin 0.4 mg once daily was more efficacious than tamsulosin 0.2 mg once daily and showed similar rates of adverse effects. Especially, tamsulosin 0.4 mg once daily was shown to improve the IPSS, QoL, Qmax, and PVR in patients refractory to treatment with tamsulosin 0.2 mg once daily. Therefore, we believe it is safe to titrate the dosage of tamsulosin according to the severity of the patients' symptoms without increasing the incidence of adverse effects.
Figures and Tables
FIG. 1
Study design: tamsulosin 0.2 mg once daily monotherapy for 8 weeks followed by 8 weeks of additional tamsulosin 0.2 mg once daily or tamsulosin 0.4 mg once daily monotherapy.

FIG. 2
Mean total International Prostate Symptom Score (IPSS) at baseline and at week 16 in the 0.2 mg group (tamsulosin 0.2 mg once daily) and the 0.4 mg group (tamsulosin 0.4 mg once daily) (n=116). 0.2 mg group (n=90): tamsulosin 0.2 mg once daily, 0.4 mg group (n=26): tamsulosin 0.4 mg once daily, a: p<0.001 versus baseline, b: p<0.001 versus baseline.

FIG. 3
Change from baseline to week 8 and week 16 in total IPSS (International Prostate Symptom Score) in the 0.2 and 0.4 mg group, 0.2 mg group: 8 weeks tamsulosin 0.2 mg once daily+additional 8 weeks tamsulosin 0.2 mg once daily, 0.4 mg group: 8 weeks tamsulosin 0.2 mg once daily+additional 8 weeks tamsulosin 0.4 mg once daily.
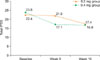
TABLE 2
Comparison of 0.2 mg group (tamsulosin 0.2 mg once daily) and of 0.4 mg group (tamsulosin 0.4 mg once daily) in improvement in IPSS, QoL, Qmax, and PVR

References
1. Garraway WM, Russell EB, Lee RJ, Collins GN, McKelvie GB, Hehir M, et al. Impact of previously unrecognized benign prostatic hyperplasia on the daily activities of middle-aged and elderly men. Br J Gen Pract. 1993. 43:318–321.
2. Chute CG, Panser LA, Girman CJ, Oesterling JE, Guess HA, Jacobsen SJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993. 150:85–89.
3. Chapple CR. BPH Disease Management. Introduction and concluding remarks. Eur Urol. 1999. 36:Suppl 3. 1–6.
4. Barkin J, Guimarães M, Jacobi G, Pushkar D, Taylor S, van Vierssen Trip OB. Alpha-blocker therapy can be withdrawn in the majority of men following initial combination therapy with the dual 5alpha-reductase inhibitor dutasteride. Eur Urol. 2003. 44:461–466.
5. Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the combAT study. Eur Urol. 2010. 57:123–131.
6. Djavan B, Chapple C, Milani S, Marberger M. State of the art on the efficacy and tolerability of alpha1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Urology. 2004. 64:1081–1088.
7. Djavan B. α1-adrenoceptor antagonists for the treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia. state of the art. Eur Urol Suppl. 2004. 3:23–30.
8. Li NC, Chen S, Yang XH, Du LD, Wang JY, Na YQ. Efficacy of low-dose tamsulosin in chinese patients with symptomatic benign prostatic hyperplasia. Clin Drug Investig. 2003. 23:781–787.
9. Park CH, Chang HS, Oh BR, Kim HJ, Sul CK, Chung SK, et al. Efficacy of low-dose tamsulosin on lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a nonblind multicentre Korean study. Clin Drug Investig. 2004. 24:41–47.
10. Lee E. Comparison of tamsulosin and finasteride for lower urinary tract symptoms associated with benign prostatic hyperplasia in Korean patients. J Int Med Res. 2002. 30:584–590.
11. Anderson JB, Roehrborn CG, Schalken JA, Emberton M. The progression of benign prostatic hyperplasia: examining the evidence and determining the risk. Eur Urol. 2001. 39:390–399.
12. Emberton M, Andriole GL, de la Rosette J, Djavan B, Hoefner K, Vela Navarrete R, et al. Benign prostatic hyperplasia: a progressive disease of aging men. Urology. 2003. 61:267–273.
13. Lepor H. Medical therapy for benign prostatic hyperplasia. Urology. 1993. 42:483–501.
14. Lepor H. Alpha blockade for the treatment of benign prostatic hyperplasia. Urol Clin North Am. 1995. 22:375–386.
15. Lepor H, Tang R, Kobayashi S, Shapiro E, Forray C, Wetzel JM, et al. Localization of the alpha 1A-adrenoceptor in the human prostate. J Urol. 1995. 154:2096–2099.
16. Djavan B, Marberger M. A meta-analysis on the efficacy and tolerability of α1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic obstruction. Eur Urol. 1999. 36:1–13.
17. Lepor H. Long-term evaluation of tamsulosin in benign prostatic hyperplasia: placebo-controlled, double-blinded extenstion of phase III trial. Tamsulosin Investigator Group. Urology. 1998. 51:901–906.
18. Schulman CC, Cortvriend J, Jonas U, Lock TM, Vaage S, Speakman MJ. European Tamsulosin Study Group. Tamsulosin, the first prostate-selective alpha 1A-adrenoceptor antagonist: analysis of a multinational, multicentre, open-label study assessing the long-term efficacy and safety in patients with benign prostatic obstruction (symptomatic BPH). Eur Urol. 1996. 29:145–154.
19. Lowe FC. Coadministration of tamsulosin and three antihypertensive agents in patients with benign prostatic hyperplasia: pharmacodynamic effect. Clin Ther. 1997. 19:730–742.
20. Wilt TJ, Mac Donald R, Rutks I. Tamsulosin for benign prostatic hyperplasia. Cochrane Database Syst Rev. 2003. (1):CD002081.
21. Abrams P, Speakman M, Stott M, Arkell D, Pocock R. A dose-ranging study of the efficacy and safety of tamsulosin, the first prostate-selective alpha 1A-adrenoceptor antagonist, in patients with benign prostatic obstruction (symptomatic benign prostatic hyperplasia). Br J Urol. 1997. 80:587–596.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download