Abstract
We report a case of laparoendoscopic single-site surgery (LESS) for a symptomatic left seminal vesicular cyst and ipsilateral renal agenesis. A 49-year-old man presented with a 1-year history of severe irritation upon voiding and intractable, recurrent hematospermia. A computed tomography scan showed a 68×41×38 mm sized left seminal vesicular cyst with ipsilateral renal agenesis. LESS was performed successfully to treat the seminal vesicle cyst. The total operative time was 125 minutes, and blood loss was minimal. The patient was discharged from the hospital on the second postoperative day.
Seminal vesicular cysts associated with ipsilateral renal agenesis are exceedingly rare. Seminal vesicular cysts are usually asymptomatic, but occasionally cause perineal pain, post-ejaculatory pain, hematospermia, infertility, and voiding symptoms [1,2]. Existing treatment methods for symptomatic seminal vesicular cysts include transrectal aspiration, transurethral unroofing, transurethral resection of the ejaculatory duct, transurethral endoscopic examination and aspiration, open surgery [3], and trans-seminal vesiculoscopic fenestration [4]. However, the first four of these methods may be associated with a risk of cyst recurrence and infection [3]. As a result, the current treatment of choice remains operative excision, although the evolution of surgical techniques and instruments has enabled successful laparoscopic cyst excision [1,2]. We performed and report here a laparoendoscopic single-site surgery (LESS) on a seminal vesicular cyst associated with irritable voiding symptom and intractable hematospermia. This study was approved by the institutional review board of Yonsei Severance hospital in Korea.
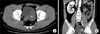
A 49-year-old man presented with a 1-year history of voiding symptoms (frequency, nocturia, and reduced force of urinary stream) and intractable recurrent hematospermia. A digital rectal examination revealed a large, mobile, non-tender, soft cystic lesion in the area of the left seminal vesicle. A pelvic computed tomography (CT) scan showed a cystic lesion, measuring 68×41×38 cm, situated on the seminal vesicle and ipsilateral renal agenesis. No and other abnormalities were visible on the CT scan (Fig. 1). Routine blood and urinary laboratory studies were normal. According to the diagnosis of a symptomatic seminal vesicular cyst, we recommended excision of the cyst. After deciding on surgical excision of the seminal vesicular cyst, we decided to perform LESS to excise the cyst to obtain better cosmesis. The patient provided informed consent to undergo the surgery.
While under general anesthesia, the patient was placed in the Trendelenburg position, padded, and secured to the operating table. For transperitoneal LESS, a 3 cm skin incision was made at the umbilicus. We used an extra small Alexis wound retractor® (Applied Medical, Rancho Santa Margarita, CA, USA) and a surgical glove as the homemade single-port device. The first, second, third, and fifth glove fingers were secured, with sutures and a rubber band, to the ends of four channels of a multichannel trocar with respective diameters of three 12 mm trocars (Laport, Sejong, Seoul, Korea) and one 5 mm trocar. Created as such, this device can provide a single port similar to that of a commercial multichannel trocar, whereby the wound retractor stabilizes the device in the umbilical incision. The inner ring of the wound retractor on the single-port device was inserted at the umbilicus. The peritoneal cavity was insufflated with CO2 gas and 12 mmHg, and a 10 mm 30° rigid laparoscope (Stryker, Kalamazoo, MI) with an integrated camera head was used. The LESS technique was performed as described previously [5]. An incision was made in the retrovesical peritoneum and the cyst was easily visualized. The left vas deferens was located and dissected medially to the seminal vesicle. The peritoneal reflection was dissected, developing the space between the bladder and the rectum, and then the dilated seminal vesicle was exposed (Fig. 2). The cyst was drained by aspiration and circumferentially dissected. The cyst was dissected downward to its base and excised by use of the LigaSure vessel sealing system (Valleylab, Boulder, CO, USA). The peritoneum was reapproximated by using an intracorporeal suturing technique and laparoscopic clips.
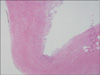
LESS was completed successfully with no additional ports. The total operative time was 125 minutes, and blood loss was minimal. The patient was discharged from the hospital on the second postoperative day. There were no complications during his postoperative care. The final pathologic diagnosis was consistent with an inflamed seminal vesicular cyst (Fig. 3). The postoperative 6-month follow-up CT scan showed complete excision of the seminal vesicular cyst (Fig. 4). The patient has had no voiding symptoms or recurrent hemospermia.
Congenital anomalies of the seminal vesicle are exceedingly rare, but when they occur, they are commonly associated with anomalies of the urinary and reproductive systems [1]. Seminal vesicular cysts occur in less than 0.005% of the general population and are usually associated with ipsilateral renal agenesis or with ipsilateral ectopic ureteral insertion [3]. Most cases of congenital seminal vesicular cysts are asymptomatic and do not require treatment. However, they do rarely cause symptoms and signs, including perineal pelvic pain, post-ejaculatory pain, hematospermia, infertility, and voiding problems [2,5]. Surgical treatment should be considered when constant and intractable symptoms are present.
Abdominopelvic and transrectal ultrasound is the initial diagnostic tool for long-standing pelvic pain and suspicious physical findings [6]. A CT scan can be used as a second diagnostic tool to detect concurrent renal agenesis and further define any pathological pelvic processes. Additional studies may include intravenous pyelogram (IVP), pelvic magnetic resonance imaging (MRI), and seminovesiculography. Cystoscopy may identify an absent ipsilateral hemitrigone, intravesical cyst protrusion, and any other anatomial abnormality of the bladder [1].
The current treatment of choice for seminal vesicular cysts is surgical excision. Conventional open surgery is considered a definitive treatment. However, it is associated with significant morbidity, such as bladder wall laceration and ureteral injury [6]. Recently, many medical centers have reported successful laparoscopic excisions of seminal vesicular cysts [1,3,6]. The laparoscopic approach is minimally invasive and can provide an excellent direct retrovesical view of the deep seminal vesicle [7]. LESS is an evolving technique for minimally invasive surgery that has been applied in certain urological procedures [8]. LESS has been applied to simple and radical nephrectomy, nephroureterectomy, ureterolithotomy, ureterectomy, and partial cystectomy. However, there have been no previous reports on LESS for seminal vesicular cyst excision. Most of the initial difficulties with these procedures were the results of poorly adapted instruments and platforms that disrupted soft tissue handling and caused instrument clashing. These difficulties caused a steep learning curve for surgeons. Cumulative experience has allowed surgeons to overcome many of these difficulties, and operative times for LESS are now similar to those for traditional laparoscopic surgeries [9]. As described here, we successfully performed LESS for excision of a symptomatic seminal vesicular cyst.
Conventional laparoscopic excision of seminal vesicular cysts is the common treatment modality. Recently, LESS has been tried as a new method of management in urologic surgery. Retrospective analysis has not demonstrated an advantage of LESS compared with standard laparoscopy, although prospective randomized trials are necessary to further determine the advantages and disadvantages of this technique [10]. We believe that an adequately powered prospective randomized comparison between LESS and standard laparoscopy will demonstrate superior cosmetic results and faster recovery with LESS than with the standard laparoscopic surgery. In this study, we evaluated the feasibility and effectiveness of the LESS approach for a symptomatic seminal vesicular cyst. We conclude that the LESS approach can be performed for excision of a symptomatic seminal vesicular cyst.
Figures and Tables
References
1. Cherullo EE, Meraney AM, Bernstein LH, Einstein DM, Thomas AJ, Gill IS. Laparoscopic management of congenital seminal vesicle cysts associated with ipsilateral renal agenesis. J Urol. 2002. 167:1263–1267.
2. Selli C, Cavalleri S, De Maria M, Iafrate M, Giannarini G. Robot-assisted removal of a large seminal vesicle cyst with ipsilateral renal agenesis associated with an ectopic ureter and a Müllerian cyst of the vas deferens. Urology. 2008. 71:1226.
3. McDougall EM, Afane JS, Dunn MD, Shalhav AL, Clayman RV. Laparoscopic management of retrovesical cystic disease: Washington University experience and review of the literature. J Endourol. 2001. 15:815–819.
4. Han WK, Lee SR, Rha KH, Kim JH, Yang SC. Transutricular seminal vesiculoscopy in hematospermia: technical considerations and outcomes. Urology. 2009. 73:1377–1382.
5. Jeon HG, Jeong W, Oh CK, Lorenzo EI, Ham WS, Rha KH, et al. Initial experience with 50 laparoendoscopic single site surgeries using a homemade, single port device at a single center. J Urol. 2010. 183:1866–1871.
6. Moudouni SM, Tligui M, Doublet JD, Tchaia K, Haab F, Gattegno B, et al. Laparoscopic excision of seminal vesicle cyst revealed by obstruction urinary symptoms. Int J Urol. 2006. 13:311–314.
7. Seo IY, Kim HS, Rim JS. Congenital seminal vesicle cyst associated with ipsilateral renal agenesis. Yonsei Med J. 2009. 50:560–563.
8. Irwin BH, Rao PP, Stein RJ, Desai MM. Laparoendoscopic single site surgery in urology. Urol Clin North Am. 2009. 36:223–235.
9. Seo IY, Lee JW, Rim JS. Laparoendoscopic single-site radical nephrectomy: a comparison with conventional laparoscopy. J Endourol. 2011. 25:465–469.
10. Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: Where have we been and where are we heading? Nat Clin Pract Urol. 2008. 5:561–568.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download