Abstract
Purpose
The aim of this study was to evaluate the effect of desmopressin combined with anticholinergics on daytime frequency and urgency in female patients with overactive bladder (OAB).
Materials and Methods
We included 68 female patients with OAB. Patients were randomly assigned to receive 5 mg of solifenacin (group I) or 5 mg of solifenacin and 0.2 mg of desmopressin (group II) for 2 weeks. A pre/post-treatment 3-day voiding diary and the Urinary Distress Inventory (UDI-6) and Incontinence Impact Questionnaire (IIQ-7) were used to assess changes in voiding symptoms and quality of life (QoL); results were compared between the two groups.
Results
Groups I and II included 31 and 37 patients, respectively. Time to first void was 12 min later in group II (105 min vs. 117 min), but this difference was not statistically significant. However, time to the second and third voids (203 min vs. 255 min, 312 min vs. 368 min) and the first urgency episode (212 min vs. 255 min) were significantly longer in group II. Compared with group I, patients in group II showed significant improvement in QoL scores. When improvement after treatment was defined as increase in time to first void of greater than 10% after 2 weeks of treatment, desmopressin with anticholinergics was more effective in patients over the age of 65 years and with more than 150 ml of voided volume.
Overactive bladder (OAB) is a symptom syndrome that is defined as urgency, with or without urge incontinence, usually with frequency and nocturia, and is known to have a significant impact on quality of life (QoL) [1-5]. Traditionally, anticholinergic drugs have been widely used for the treatment of OAB. However, their effectiveness is known to be 60% to 70% [6]. Additionally, they lack selectivity for the bladder, and effects on other organ systems may result in side effects, including dry mouth, blurred vision, constipation, and dizziness, which limit their usefulness [7].
Desmopressin is a synthetic vasopressin analogue with a pronounced antidiuretic effect that is used widely for the treatment of primary nocturnal enuresis and nocturnal polyuria [8,9].
Several recent clinical trials have reported promising results showing improvement of symptoms of daytime frequency and urgency in patients with OAB with desmopressin through decreases in renal urine production and increases in bladder filling time [10,11]. However, there have been no reports concerning the effect of desmopressin combined with anticholinergics. Therefore, we performed this study to evaluate the effect of desmopressin combined with anticholinergics on daytime frequency and urgency in female patients with OAB.
Between July 2008 and June 2009, patients were recruited at one tertiary urologic institution. Eligible patients were females 18 years and older with OAB syndrome who had at least four voids in the first 8 hours of the day after rising, excluding the first morning void.
Patients with abnormal renal function or serum electrolytes, significant pelvic organ prolapse, stress urinary incontinence, urinary tract infection, significant postvoid residual (>150 ml), or a history of medication for treatment of OAB within 30 days were excluded.
The study was conducted in accordance with ethical principles that have their origins in the Declaration of Helsinki, and written informed consent was obtained from all patients before recruitment into the study.
Patients were randomly assigned to receive 5 mg of solifenacin (group I) or 5 mg of solifenacin and 0.2 mg of desmopressin (group II) for 2 weeks. Patients were instructed to take the tablets after the first morning void.
The primary efficacy end point was evaluation of the effectiveness of desmopressin in increasing the time to each of the first OAB symptom episodes (frequency and urgency). The secondary efficacy end points were evaluation of the effectiveness of desmopressin on QoL, in decreasing the average number of OAB symptoms (frequency and urgency) during the first 8 hours of the day following treatment, and outcome predictors of desmopressin with anticholinergics. Efficacy measures included 3-day voiding diary variables, the Urogenital Distress Inventory (UDI-6), and the Incontinence Impact Questionnaire (IIQ-7), which were completed by patients at baseline and at week 2 and were assessed as the change from baseline. Safety assessments including body weight, serum sodium monitoring, and adverse event reports were recorded at baseline and week 2. Scores on the UDI-6 and IIQ-7 were calculated on a scale from 0 to 100 [12]. A score of 0 indicated that the patient was not bothered at all by a particular symptom and a score of 100 implied the most severe degree of dissatisfaction with a particular symptom.
SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Student's t-test, Mann-Whitney U test, and univariate logistic regression analysis were used for statistical assessment of results and a value of p-value <0.05 was considered statistically significant.
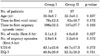
A total of 84 patients were randomly assigned to 2 groups, and 68 (81%) of 84 patients completed the study. Groups I and II had 31 and 37 patients, respectively. Mean patient age was 54.2±7.3 years and baseline clinical characteristics were similar among the groups (Table 1).
Time to first void was 12 min later in group II (105 min vs. 117 min) than in group I; however, this difference was not statistically significant (Student's t-test, p>0.05) (Fig. 1). However, time to the second and third voids (203 min vs. 255 min, 312 min vs. 368 min) and time to the first urgency episode (212 min vs. 255 min) were significantly longer in group II (Student's t-test, p<0.05) (Fig. 1, 2).
Significant decreases were observed in the numbers of voids (4.5 vs. 3.2) and urgency episodes (2.6 vs. 1.7) during the first 8 hours following treatment in group II compared with group I (Mann-Whitney U test, p<0.05) (Fig. 3). Compared with group I, patients in group II showed significant improvement in QoL scores as measured by the UDI-6 and IIQ-7 (Student's t-test, p<0.05) (Fig. 4).
When improvement after treatment was defined as an increase in time to first void of greater than 10% after 2 weeks of treatment, desmopressin with anticholinergics was more effective in patients over the age of 65 years (odds ratio [OR]=1.2, 95% confidence interval [CI]: 1.00-1.16, p<0.05) (Table 2) and with more than 150 ml of voided volume (OR=1.3, 95% CI: 1.13-1.59, p<0.01) (Table 2) in the univariate regression analysis for determination of predictive factors influencing improvement.
OAB is a symptom syndrome consisting of urgency, with or without urgency incontinence, usually with frequency and nocturia [1], and is a common and distressing condition known to have an adverse effect on QoL [2-5]. First-line therapy for OAB includes conservative treatment in the form of lifestyle intervention, pelvic floor exercises, and bladder training. These offer better results when combined with anticholinergics, which are the first-line medical therapy for OAB. However, anticholinergic medication is associated with typical side effects, including dry mouth, constipation, and blurred vision. Compliance with anticholinergic medication is also a significant problem. In a questionnaire follow-up study of women with OAB, only 5.5% were cured of their OAB symptoms and only 18.2% of women continued drug therapy for longer than 6 months [7].
For OAB patients who are refractory to anticholinergics, modalities such as botulinum toxin injection, neuromodulation, and various surgical interventions can be attempted. However, these also have side effects and limitations and are not curative. Therefore, discovery of alternative modalities of medical treatment for OAB, which could delay any invasive treatments, is crucial.
Desmopressin (1-desamino-8-D-arginine vasopressin) is a synthetic nonapeptide analogue of antidiuretic hormone that affects renal water reabsorption, leading to decreased urine production. To date, desmopressin has been used in the treatment of disorders such as diabetes insipidus, primary nocturnal enuresis, and nocturia with a polyuric background.
Well-controlled trials have been performed to evaluate the safety, efficacy, and tolerability of desmopressin in the treatment of patients with nocturia [13-16]. Duration of the period from bedtime until the first nocturnal void (first sleep period) is one of the frequently used efficacy end points in clinical trials for evaluation of the efficacy of desmopressin in patients with nocturia; findings from previously reported studies have shown an increase in the first sleep period of 1.5 to 2.2 hours [17].
Some recent studies have reported the efficacy of desmopressin in patients with OAB [10,11]. The rationale for use of desmopressin in the treatment of OAB patients is that through a decrease in urine production, desmopressin will increase the time taken to reach functional bladder capacity between daytime voids, thereby reducing frequency and urgency and benefiting adults suffering from OAB. This is very similar to the rationale for use of desmopressin in nocturia patients; therefore, we used the time to the first OAB symptom episode (micturition and urgency) as the primary end point, because in previous desmopressin trials, the concept of time to the first nocturnal void was used and this was increased by use of desmopressin, resulting in a greater number of hours of undisturbed sleep [14,15].
Robinson et al administered 40 µg intranasal desmopressin to 64 women with urinary incontinence lasting over 10 days [11]. Results showed that patients taking desmopressin had a significantly higher mean incidence of periods with no leakage during the first 4 and 8 hours after taking desmopressin. This study was the first to explore the concept of antidiuresis as a strategy for management of daytime OAB symptoms in women and the results were very encouraging; however, it did not look at the effect on other OAB symptoms, such as frequency and urgency.
Recently, in a double-blind placebo-controlled trial that evaluated the efficacy of desmopressin in the treatment of female patients with OAB, desmopressin induced a significant increase in the time to the first urgency episode, with a significant reduction in the mean numbers of urgency episodes, compared to placebo, and subjective improvement was observed in frequency and urgency as well as overall QoL [10].
Currently, anticholinergics are the primary treatment for OAB; therefore, unlike previous studies [10,11] concerning the efficacy of desmopressin in patients with OAB, which compared the desmopressin group and the placebo group, our study was designed to address the issue of pharmacological antidiuresis in OAB patients who take anticholinergic medication.
Like the previous studies, we analyzed the changes in OAB symptoms during the first 8 hours of the day following medication because it is known that desmopressin is most effective during this period.
In our study, desmopressin did not induce a significant increase in the time to the first frequency episode; however, the time to the first urgency episode increased and the numbers of frequency and urgency episodes showed a significant decrease in the desmopressin with anticholinergics group. In addition, QoL as measured by the UDI-6 and IIQ-7 showed significant improvement in the desmopressin with anticholinergics group. These results are similar to those of the previous study [10]. In the future, antidiuresis using desmopressin could have potential for use in the treatment of OAB.
The effects of desmopressin in our patients were probably due to the decreased urine volume in the daytime. However, we did not analyze the changes in urine volume because measurement of urinary output was incomplete in most of our patients, and this may be one drawback of the study. In addition, the 2-week period of our study was too short to conclude that combined therapy is more effective than anticholinergics alone on a long-term basis, because the effect of anticholinergics could be gradually increased up to 2 to 3 months. Therefore, larger long-term studies will need to be conducted to prove the concept that reduction in urine volume production helps in OAB patients and to determine the long-term effect of combined therapy.
There have been no reports concerning the predictive factors for the effect of desmopressin with anticholinergics in OAB patients. Therefore, we performed subanalysis of the desmopressin with anticholinergics group to evaluate the outcome predictors of desmopressin in OAB patients. Age (>65 years) and voided volume (>150 ml) showed a significant association with improvement of OAB symptoms after desmopressin medication.
However, these results had some drawbacks, because it is not known how many increases in time to first void is needed to improve QoL, and the number of patients in the desmopressin with anticholinergics group was small. Therefore, the outcome predictors of desmopressin with anticholinergics in OAB patients should be explored further in a larger confirmatory trial.
Hyponatremia is the only serious potential adverse event associated with the use of desmopressin [18-20]. In the present study, desmopressin was well tolerated by the majority of patients. No significant hyponatremia was reported in any patient. However, significant hyponatremia occurred in 4% to 6% of patients in the published trials [21,22], particularly in patients over the age of 65 years. Therefore, precautions should be taken in older patients, including close monitoring of prodromal symptoms, such as headache and weight increase, and avoidance of excessive fluid intake.
Desmopressin combined with anticholinergics was more effective than anticholinergics alone in the treatment of female patients with OAB. Therefore, desmopressin combined with anticholinergics could be considered as a novel, feasible method for relief of symptoms in female patients with OAB, and larger long-term studies will need to be conducted of the use of desmopressin in patients with OAB on a long-term basis.
Figures and Tables
FIG. 1
Time to first, second, and third voids in each group after treatment (a: p=0.012, b: p=0.007).

FIG. 3
Numbers of micturition and urgency episodes in each group after treatment (a: p=0.02, b: p=0.016).
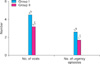
FIG. 4
Scores on the Urogenital Distress Inventory (UDI-6) and Incontinence Impact Questionnaire (IIQ-7) in each group after treatment (a: p=0.023, b: p=0.014).

References
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.
2. Komaroff AL, Fagioli LR, Doolittle TH, Gandek B, Gleit MA, Guerriero RT, et al. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Am J Med. 1996. 101:281–290.
3. Kelleher CJ, Reese PR, Pleil AM, Okano GJ. Health-related quality of life of patients receiving extended-release tolterodine for overactive bladder. Am J Manag Care. 2002. 8:19 Suppl. S608–S615.
4. Liberman JN, Hunt TL, Stewart WF, Wein A, Zhou Z, Herzog AR, et al. Health-related quality of life among adults with symptoms of overactive bladder: results from a U.S. community-based survey. Urology. 2001. 57:1044–1050.
5. Song HD, Cho SY, Lee KC, Cho IR. The risk factors for increased post-voiding residual urine volume after long-term anticholinergic therapy in patients with benign prostatic hyperplasia and overactive bladder. Korean J Urol. 2009. 50:982–988.
6. Lee KS, Lee YS. Overactive bladder. Korean J Urol. 2007. 48:1191–1208.
7. Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A medium-term analysis of the subjective efficacy of treatment for women with detrusor instability and low bladder compliance. Br J Obstet Gynaecol. 1997. 104:988–993.
8. Andersson KE. Current concepts in the treatment of disorders of micturition. Drugs. 1988. 35:477–494.
9. Nevéus T, Läckgren G, Tuvemo T, Olsson U, Stenberg A. Desmopressin resistant enuresis: pathogenetic and therapeutic considerations. J Urol. 1999. 162:2136–2140.
10. Hashim H, Malmberg L, Graugaard-Jensen C, Abrams P. Desmopressin, as a "designer-drug," in the treatment of overactive bladder syndrome. Neurourol Urodyn. 2009. 28:40–46.
11. Robinson D, Cardozo L, Akeson M, Hvistendahl G, Riis A, Norgaard JP. Antidiuresis: a new concept in managing female daytime urinary incontinence. BJU Int. 2004. 93:996–1000.
12. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Continence Program for Women Research Group. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Neurourol Urodyn. 1995. 14:131–139.
13. Asplund R, Sundberg B, Bengtsson P. Oral desmopressin for nocturnal polyuria in elderly subjects: a double-blind, placebo-controlled randomized exploratory study. BJU Int. 1999. 83:591–595.
14. Mattiasson A, Abrams P, Van Kerrebroeck P, Walter S, Weiss J. Efficacy of desmopressin in the treatment of nocturia: a double-blind placebo-controlled study in men. BJU Int. 2002. 89:855–862.
15. Lose G, Lalos O, Freeman RM, van Kerrebroeck P. Efficacy of desmopressin (Minirin) in the treatment of nocturia: a double-blind placebo-controlled study in women. Am J Obstet Gynecol. 2003. 189:1106–1113.
16. van Kerrebroeck P, Rezapour M, Cortesse A, Thüroff J, Riis A, Nørgaard JP. Desmopressin in the treatment of nocturia: a double-blind, placebo-controlled study. Eur Urol. 2007. 52:221–229.
17. Committee for Establishment of the Clinical Guidelines for Nocturia of the Neurogenic Bladder Society. Clinical guidelines for nocturia. Int J Urol. 2010. 17:397–409.
18. Rembratt A, Riis A, Norgaard JP. Desmopressin treatment in nocturia; an analysis of risk factors for hyponatremia. Neurourol Urodyn. 2006. 25:105–109.
19. Rembratt A, Graugaard-Jensen C, Senderovitz T, Norgaard JP, Djurhus JC. Pharmacokinetics and pharmacodynamics of desmopressin administered orally versus intravenously at daytime versus night-time in healthy men aged 55-70 years. Eur J Clin Pharmacol. 2004. 60:397–402.
20. Weatherall M. The risk of hyponatremia in older adults using desmopressin for nocturia: a systematic review and meta-analysis. Neurourol Urodyn. 2004. 23:302–305.
21. Mattiasson A, Abrams P, van Kerrebroeck P, Walters S, Weiss J. Efficacy of desmopressin in the treatment of nocturia: a double-blind placebo-controlled study in men. BJU Int. 2002. 89:855–862.
22. Lose G, Lalos O, Freeman RM, van Kerrebroeck P. Efficacy of desmopressin (Minirin) in the treatment of nocturia: a double-blind placebo-controlled study in women. Am J Obstet Gynecol. 2003. 189:1106–1113.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download