1. Trabulsi EJ, Guillonneau B. Laparoscopic radical prostatectomy. J Urol. 2005. 173:1072–1079.
2. Tooher R, Swindle P, Woo H, Miller J, Maddern G. Laparoscopic radical prostatectomy for localized prostate cancer: a systematic review of comparative studies. J Urol. 2006. 175:2011–2017.
3. Touijer K, Eastham JA, Secin FP, Romero Otero J, Serio A, Stasi J, et al. Comprehensive prospective comparative analysis of outcomes between open and laparoscopic radical prostatectomy conducted in 2003 to 2005. J Urol. 2008. 179:1811–1817.
4. Lepor H. Open versus laparoscopic radical prostatectomy. Rev Urol. 2005. 7:115–127.
5. Ghavamian R, Knoll A, Boczko J, Melman A. Comparison of operative and functional outcomes of laparoscopic radical prostatectomy and radical retropubic prostatectomy: single surgeon experience. Urology. 2006. 67:1241–1246.
6. Guazzoni G, Cestari A, Naspro R, Riva M, Centemero A, Zanoni M, et al. Intra-and peri-operative outcomes comparing radical retropubic and laparoscopic radical prostatectomy: results from a prospective, randomized, single-surgeon study. Eur Urol. 2006. 50:98–104.
7. Erdogru T, Teber D, Frede T, Marrero R, Hammady A, Seemann O, et al. Comparison of transperitoneal and extraperitoneal laparoscopic radical prostatectomy using match-pair analysis. Eur Urol. 2004. 46:312–319.
8. Hsu El, Hong EK, Lepor H. Influence of body weight and prostate volume on intraoperative, perioperative, and postoperative outcomes after radical retropubic prostatectomy. Urology. 2003. 61:601–606.
9. Chang SS, Duong DT, Wells N, Cole EE, Smith JA Jr, Cookson MS. Predicting blood loss and transfusion requirements during radical prostatectomy: the significant negative impact of increasing body mass index. J Urol. 2004. 171:1861–1865.
10. Freedland SJ, Aronson WJ, Kane CJ, Presti JC Jr, Amling CL, Elashoff D, et al. Impact of obesity on biochemical control after radical prostatectomy for clinically localized prostate cancer: a report by the Shared Equal Access Regional Cancer Hospital database study group. J Clin Oncol. 2004. 22:446–453.
11. Freedland SJ, Grubb KA, Yiu SK, Nielsen ME, Mangold LA, Isaacs WB, et al. Obesity and capsular incision at the time of open retropubic radical prostatectomy. J Urol. 2005. 174:1798–1801.
12. Ahlering TE, Eichel L, Edwards R, Skarecky DW. Impact of obesity on clinical outcomes in robotic prostatectomy. Urology. 2005. 65:740–744.
13. Zorn KC, Orvieto MA, Mikhail AA, Gofrit ON, Lin S, Schaeffer AJ, et al. Effect of prostate weight on operative and postoperative outcomes of robotic-assisted laparoscopic prostatectomy. Urology. 2007. 69:300–305.
14. Rassweiler J, Schulze M, Teber D, Marrero R, Seemann O, Rumpelt J, et al. Laparoscopic radical prostatectomy with the Heilbronn technique: oncological results in the first 500 patients. J Urol. 2005. 173:761–764.
15. Guillonneau B, Rozet F, Cathelineau X, Lay F, Barret E, Doublet JD, et al. Preoperative complications of laparoscopic radical prostatectomy: the Montsouris 3-year experience. J Urol. 2002. 167:51–56.
16. Guillonneau B, el-Fettouh H, Baumert H, Cathelineau X, Doublet JD, Fromont G, et al. Laparoscopic radical prostatectomy: oncological evaluation after 1,000 cases a Montsouris Institute. J Urol. 2003. 169:1261–1266.
17. Ferguson GG, Ames CD, Weld KJ, Yan Y, Venkatesh R, Landman J. Prospective evaluation of learning curve for laparoscopic radical prostatectomy: identification of factors improving operative times. Urology. 2005. 66:840–844.
18. Brown JA, Rodin DM, Lee B, Dahl DM. Laparoscopic radical prostatectomy and body mass index: an assessment of 151 sequential cases. J Urol. 2005. 173:442–445.
19. Castle EP, Atug F, Woods M, Thomas R, Davis R. Impact of body mass index on outcomes after robot assisted radical prostatectomy. World J Urol. 2008. 26:91–95.
20. Rassweiler J, Sentker L, Seemann O, Hatzinger M, Rumpelt HJ. Laparoscopic radical prostatectomy with the Heilbronn technique: an analysis of the first 180 cases. J Urol. 2001. 166:2101–2108.
21. EL-Feel A, Davis JW, Deger S, Roigas J, Wille AH, Schnorr D, et al. Laparoscopic radical prostatectomy--an analysis of factors affecting operating time. Urology. 2003. 62:314–318.
22. Chang CM, Moon D, Gianduzzo TR, Eden CG. The impact of prostate size in laparoscopic radical prostatectomy. Eur Urol. 2005. 48:285–290.
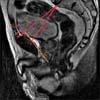
23. Kim JS, Im CM, Kwon DD, Park K, Ryu SB. The factor affecting radical retropubic prostatectomy: the bony pelvic shape imaged by magnetic resonance imaging. Korean J Urol. 2008. 49:320–324.
24. Hong SK, Chang IH, Han BK, Yu JH, Han JH, Jeong SJ, et al. Impact of variations in bony pelvic dimensions on performing radical retropubic prostatectomy. Urology. 2007. 69:907–911.
25. Hong SK, Lee ST, Kim SS, Min KE, Hwang IS, Kim M, et al. Effect of bony pelvic dimensions measured by preoperative magnetic resonance imaging on performing robot-assisted laparoscopic prostatectomy. BJU Int. 2009. 104:664–668.
26. Emerson RE, Koch MO, Jones TD, Daggy JK, Juliar BE, Cheng L. The influence of extent of surgical margin positivity on prostate specific antigen recurrence. J Clin Pathol. 2005. 58:1028–1032.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download