Abstract
Sarcoidosis is an idiopathic, multisystem disease that rarely involves the genitourinary tract. Here we present an unusual case of testicular sarcoidosis with extensive lymphadenopathy that mimicked a metastatic testicular tumor. A 27-year-old male presented with a palpable right testicular mass accompanied by multiple palpable inguinal lymph nodes. The scrotal ultrasound showed a hypoechoic lesion at the inferior portion of the right testis. Extensive enlarged lymph nodes were noted in multiple areas on the abdominal computed tomography. Preoperative testicular tumor markers were within the normal range. Exploration of the right testis with a frozen section analysis of the right testicular mass and of a palpable right inguinal lymph node showed granulomatous inflammation. The testis was salvaged and the final pathological diagnosis was sarcoidosis. Treatment with high-dose corticosteroids resulted in complete resolution of the intratesticular mass and a significant decrease in the extent of the lymphadenopathy.
Sarcoidosis is an idiopathic, multisystem disease characterized by epitheloid, non-caseating granulomas, primarily and most frequently involving the lungs. Sarcoidosis involving the male reproductive tract has rarely been reported and most typically presents with a bilateral testicular or epididymal mass accompanied by hilar lymphadenopathy [1]. To our knowledge, sarcoidosis involving the testis has not been reported in the Korean literature. Here we present an unusual case of extensive systemic sarcoidosis with testicular involvement that mimicked a metastatic testicular tumor.
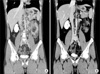
A 27-year-old male visited our clinic with a palpable right testicular mass that had developed three months earlier. A physical examination revealed the right testis to be of normal size and shape, with a hard, 1 cm nodule at the inferior pole. Multiple, elastic, nontender nodules were palpated in the inguinal area bilaterally. Scrotal ultrasonography revealed an ill-defined, irregular, hypoechoic lesion on the inferior pole of the right testis with surrounding increased vascularity and parenchymal deformity (Fig. 1). The left testis and epididymis were normal, except for the identification of an incidental varicocele. The chest radiograph was normal. A disseminated malignancy involving the testis was suspected and abdominal computed tomography (CT) was therefore performed. The abdominal CT showed extensive lymphadenopathy involving the cardiophrenic, mediastinal, retroperitoneal, pelvic, and inguinal lymph nodes (Fig. 2A). In addition, peritoneal infiltration and enhancing nodules of the omentum, gastrosplenic ligament, mesentery, and antero-inferior portion of the right testis were noted. Testicular tumor markers such as α-fetoprotein, β-human chorionic gonadotropin, and lactic dehydrogenase were within normal ranges.
Exploration of the right testis was undertaken through an inguinal incision. The spermatic cord was occluded with an elastic band and the testis was delivered through the wound. A 1 cm mass at the lower pole of the testis was readily identified and incised. The cut surface was glistening and white. Two small pieces of the tissue were sent for frozen biopsy; the results showed granulomatous inflammation without evidence of malignancy. The biopsy site was repaired and the testis was repositioned in the scrotum. An enlarged right superficial inguinal node was excised. The permanent sections of the testicular mass and the node revealed non-caseating granulomatous inflammation (Fig. 3). Tuberculosis was excluded by a negative polymerase chain reaction for tuberculosis. The final diagnosis was consistent with sarcoidosis.
High-dose corticosteroid therapy was started on the third postoperative week with 60 mg of oral prednisolone daily. The daily dose was reduced at monthly intervals to 40, 20, and 10 mg, and the treatment was discontinued at the end of the fourth month. At the end of the treatment, the testicular mass resolved. On the follow-up CT scan taken 4 months after the start of the corticosteroid therapy, the lymphadenopathy had significantly decreased (Fig. 2B). The patient was followed carefully without any further treatment.
Sarcoidosis is a systemic disease of unknown cause, most likely related to disordered immunity [2]. In 80% to 90% of cases, the findings are localized to the chest. A bilateral hilar lymphadenopathy on chest radiographs is usually incidentally detected. Sarcoidosis can involve any organ, but male genitourinary involvement is very unusual. Kodama et al reviewed 60 cases of sarcoidosis involving the male reproductive tract and found that the epididymis was the most frequently involved organ, followed by the testis, in 28 patients [1]. Most patients were 20 to 40 years of age and about half of the patients presented with scrotal discomfort or pain and constitutional symptoms such as fever and fatigue. Physical examination frequently revealed a nontender, elastic, firm nodule that involved the testis or epididymis, which may be indistinguishable from testicular cancer, often leading to an orchiectomy in one-third of cases. There are some reports of testicular tumors co-existing with sarcoidosis [3,4]. In addition, a retrospective review from the Mayo Clinic demonstrated a strong association between the two conditions with an approximately 100-fold increase in sarcoidosis in men with a history of treated testicular cancer [5]. Thus, orchiectomy is usually indicated in patients presenting with a unilateral intrascrotal mass, even in cases of known systemic sarcoidosis. On the other hand, some have advocated for organ preservation after surgical exploration, reserving orchiectomy for the patients in whom no alternatives are available or in whom a malignancy is suspected [6].
The case presented here was unique in that the patient presented with a unilateral testicular mass and multiple, palpable inguinal lymph nodes. This is unusual for an apparently small, confined tumor. Therefore, a preoperative CT scan was performed, revealing extensive systemic lymphadenopathy. A radical orchiectomy would have been the appropriate treatment for metastatic testicular cancer. However, the presence of extensive lymphadenopathy was disproportionate to the size of the testicular lesion. Therefore, simultaneous biopsy of both the testicular mass and inguinal lymph nodes provided the information needed to make the correct diagnosis, and an orchiectomy was not needed in this young male patient.
Use of steroid treatment for sarcoidosis is usually limited to symptomatic cases due to the associated side effects and the propensity for spontaneous remission over a period of up to 3 years [1]. Although the patient reported here was asymptomatic after the testicular biopsy, the very extensive associated lymphadenopathy led to the decision to start steroid therapy. The usual starting dose of oral prednisolone is 40 mg or 60 mg daily depending on the severity of the disease, and the drug is tapered and discontinued after complete resolution of the disease [7,8]. Steroid therapy in cases of such extensive sarcoidosis may be justified.
A young male presenting with a unilateral testicular mass and unusual features of sarcoidosis, such as extensive inguinal lymphadenopathy, should undergo further imaging studies to rule out systemic disease. Even in the absence of hilar lymphadenopathy on standard chest radiographs, sarcoidosis should be considered as a possible diagnosis. This case illustrates salvage of the testis and high-dose corticosteroid therapy for extensive testicular sarcoidosis as effective patient management.
Figures and Tables
FIG. 1
Scrotal ultrasound showing ill-defined, irregular, hypoechoic lesion at the inferior portion of the right testis (arrow).

FIG. 2
A 3D coronal image computed tomography scan of the abdomen after administration of intravenous contrast medium. (A) Extensive enlarged lymph nodes were seen in the retroperitoneal space. (B) Four months after the start of high-dose corticosteroid therapy, multiple, extensive retroperitoneal lymph nodes had considerably decreased in size.
References
1. Kodama K, Hasegawa T, Egawa M, Tomosugi N, Mukai A, Namiki M. Bilateral epididymal sarcoidosis presenting without radiographic evidence of intrathoracic lesion: review of sarcoidosis involving the male reproductive tract. Int J Urol. 2004. 11:345–348.
2. Reineks EZ, MacLennan GT. Sarcoidosis of the testis and epididymis. J Urol. 2008. 179:1147.
3. Geller RA, Kuremskey DA, Copeland JS, Stept R. Sarcoidosis and testicular neoplasm: an unusual association. J Urol. 1977. 118:487–488.
4. Blacher EJ, Maynard JF. Seminoma and sarcoidosis: an unusual association. Urology. 1985. 26:288–289.
5. Rayson D, Burch PA, Richardson RL. Sarcoidosis and testicular carcinoma. Cancer. 1998. 83:337–343.
6. Massarweh NN, Bhalani VK, Shaw KK, Crawford B, Lang E, Davis R. Testicular presentation of sarcoidosis and organ preservation: case report and review of management strategies. Urology. 2006. 67:200.
7. Miyazaki E, Tsuda T, Mochizuki A, Sugisaki K, Ando M, Matsumoto T, et al. Sarcoidosis presenting as bilateral hydronephrosis. Intern Med. 1996. 35:579–582.
8. Datta SN, Freeman A, Amerasinghe CN, Rosenbaum TP. A case of scrotal sarcoidosis that mimicked tuberculosis. Nat Clin Pract Urol. 2007. 4:227–230.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download