Abstract
Purpose
We evaluated the long-term effects of loxoprofen on nocturia in patients with benign prostatic hyperplasia (BPH).
Materials and Methods
Between January 2006 and December 2008, 40 BPH patients with 2 or more episodes of nocturia received an alpha-blocker, 5-alpha reductase inhibitor, and a single dose of 60 mg of loxoprofen at night before sleep for 12 months (Group I). During the same period, 38 BPH patients selected as the control group received an alpha-blocker and 5-alpha reductase inhibitor (Group II). Patients were reevaluated after 3, 6, and 12 months of treatment by the number of nocturia episodes and side effects.
Results
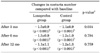
After 3 months of treatment, the number of nocturia episodes decreased significantly compared with baseline in both group I and group II (1.9±0.7, 2.1±0.7, respectively, p<0.05). The degree of decrease in nocturia was significantly different between the groups (-1.5±0.9, -1.1±0.9, respectively, p=0.034). After 6 and 12 months, the number of nocturia episodes decreased significantly compared with baseline in both group I and group II (p<0.05), but the degree of decrease was not significantly different between the groups (p>0.05). After 6 and 12 months of treatment in group I, treatment-emergent adverse events, including 5 cases of gastric discomfort (12.5%), 3 cases of leg edema (7.5%), and 1 case of decreased urine volume (2.5%), occurred in 9 of the 40 (22.5%) patients.
Nocturia in patients with benign prostatic hyperplasia (BPH) is one of the most uncomfortable symptoms of the disease. It greatly affects quality of life by deteriorating the quality of sleep and disturbing activities during the day [1,2].
Nocturia is relieved in only 25% to 39% of BPH patients treated with an alpha-blocker or 5-alpha reductase inhibitor (5ARI), and nocturia of at least two times persists in 38% of patients who undergo transurethral resection of the prostate [3-5]. In addition, using drugs such as anticholinergics, hypnotics, or antidiuretics in combination with the above-mentioned therapies in order to reduce nocturia is not effective in many cases.
Loxoprofen sodium (loxoprofen), a nonsteroidal anti-inflammatory drug (NSAID), is a nonselective cyclooxygenase (COX) inhibitor. There are reports indicating that short-term use of loxoprofen can reduce the number of episodes of nocturia [6-11].
However, no studies have assessed the long-term effects of loxoprofen on nocturia. We thus conducted a retrospective study to assess the effect of long-term use of loxoprofen on nocturia in patients with BPH.
The hospital records of patients with BPH who visited our hospital for lower urinary tract symptoms (LUTS) from January 2008 to December 2008 were analyzed retrospectively. Among them, we chose patients who complained of continued nocturia of two times or more even after the use of an alpha-blocker and 5ARI for 3 months or longer. Among the patients who were able to be followed up for 12 months, 40 patients received an alpha-blocker and 5ARI as well as loxoprofen 60 mg before sleep (loxoprofen group) and 38 patients received only an alpha-blocker and 5ARI (control group). We compared the number of nocturia episodes in the two groups before loxoprofen administration and the number of episodes of nocturia and the International Prostate Symptom Score (IPSS) after treatment for 3, 6, and 12 months. Adverse events were also examined for each period.
We excluded patients who had a history of undergoing treatment or operation for BPH, acute urinary retention, urinary tract infection, bladder stone, urethral stricture, or neurogenic bladder as well as patients who had taken or were taking drugs such as anticholinergics, cholinergics, or diuretics that can affect voiding symptoms.
Differences in the number of episodes of nocturia by period between the two groups were analyzed by unpaired t-tests, and differences between before and after treatment in each group were analyzed by paired t-tests. The results were judged to be statistically significant when the p-value was smaller than 0.05. The statistics program used in this study was SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA).
There were no significant differences between the two groups at the time of loxoprofen administration in age, prostate-specific antigen (PSA), prostate volume, IPSS, or number of episodes of nocturia (Table 1).
The number of episodes of nocturia in the two groups at 3 months after treatment was 1.9±0.7 and 2.1±0.7, respectively, and thus was significantly reduced after treatment in both groups (p<0.05). The degree of reduction in nocturia in the two groups was -1.5±0.9 times and -1.1±0.9 times, respectively. Thus, the number of episodes was reduced more in the loxoprofen group (p=0.034). The number of episodes of nocturia in the two groups at 6 and 12 months after treatment was significantly reduced compared with before treatment (p<0.05), but there was no significant difference in the degree of reduction between the two groups (p>0.05) (Table 2, Fig. 1).
The adverse events found in the loxoprofen group were gastric discomfort in four patients (10.0%) and decreased urine output in one patient (2.5%) at 6 months after treatment and gastric discomfort in one patient (2.5%) and lower leg edema in three patients (7.5%) at 12 months after treatment. In the control group, on the other hand, gastric discomfort was found in one patient (2.6%) at 3 months after treatment, and gastric discomfort occurred in one patient (2.6%) and lower leg edema in one patient (2.6%) at 6 months after treatment (Table 3).
Although the most frequent cause of LUTS in males is lower urinary tract obstruction by BPH, in addition to the obstruction, many factors such as dysfunctional detrusor, sensory disturbance, and polyuria work as mechanisms of LUTS [12].
Combination therapy (alpha-blocker+5ARI) is widely used as a drug treatment for LUTS in BPH patients. If nocturia persists even with combination therapy, however, other drugs such as anticholinergics, antidiuretics, and hypnotics are often added.
Loxoprofen, an NSAID, is a nonselective COX inhibitor that suppresses prostaglandin (PG) synthesis [6,7]. PGs are formed in the lower urinary tract and show diverse effects on the kidney, the bladder, the ureter, and the sympathetic nerve system. Among the many PGs, prostaglandin E (PGE) and prostaglandin F (PGF) are known to increase the contractility of the detrusor [13,14].
Loxoprofen's effect on LUTS can be considered to have four different mechanisms. First, loxoprofen reduces blood flow from the kidney to the glomeruli, thereby reducing urine production [15]. Second, it suppresses PGF, which reduces the detrusor's contractility, thereby reducing the desire to void [16,17]. Third, it suppresses afferent or efferent nerve pathways to raise the threshold of the sense of urination of the central nervous system [18,19]. Last, it affects the sleep cycle of the brain to induce sufficient sleep [20,21].
In a study of loxoprofen and nocturia, Okada et al reported that nocturia was reduced by approximately 1.6 times when loxoprofen was taken before sleep for 2 weeks [8]. Saito et al had patients take loxoprofen before sleep for 1 week and reported the improvement of nocturia by approximately two times [9]. Chang et al reported that when loxoprofen had been administered before sleep for 2 weeks to nocturia patients who had not shown any effect of anticholinergics and hypnotics, the number of nocturia episodes was reduced in approximately 74.7% of the patients [10]. Araki et al reported that in the case of BPH patients who had not shown any effect of anticholinergics, hypnotics, tricyclic antidepressants, or antidiuretic hormone, the number of nocturia episodes was reduced in approximately 74.2% when loxoprofen was administered before sleep for 2 weeks [11]. However, none of these studies were conducted for longer than 2 weeks, and until now no study had been conducted on changes in nocturia after the administration of loxoprofen for 1 month or longer. In the present study, BPH patients with refractory nocturia with no past history of use of other drugs were followed up for a long period of time of 12 months with the administration of an alpha-blocker, 5ARI, and loxoprofen 60 mg one time before sleep every day. Our results suggest that the number of episodes of nocturia was reduced more in the loxoprofen group than in the control group. This study can be said to be quite meaningful because it is the first study to evaluate the long-term effect of loxoprofen on nocturia.
However, although the number of nocturia episodes decreased more in the loxoprofen group than in the control group at 3 months after loxoprofen administration, the decrease in the number of nocturia episodes became similar between the two groups after 6 months. This may be because the long-term use of 5ARI reduced the volume of the prostate, thereby improving the LUTS and affecting the number of episodes of nocturia. It is also assumed that the effect of loxoprofen might have been reduced after 3 months in the loxoprofen group. More studies should be performed to understand the mechanism and causes of the reduced effect of loxoprofen after its long-term use.
In a study of adverse events resulting from loxoprofen, Waikakul and Waikakul reported that adverse events occurred in 8.4% of 1,206 patients aged 56 years on average [22]. Among the adverse events, gastric discomfort occurred the most frequently. In our study, no adverse event appeared until 3 months after the administration of loxoprofen. When loxoprofen had been administered for longer than 6 months, six cases of gastric discomfort (12.5%), three cases of leg edema (7.5%), and one case of decreased urine volume (2.5%) were noted. But, all of these complications were mild and did not indicate a necessity to stop the administration of loxoprofen. However, because the long-term use of loxoprofen in older people may involve relatively high risks of side effects such as gastric discomfort and renal failure, and because these adverse events in older people may be fatal, long-term use of loxoprofen should be considered carefully.
The present study was conducted on patients who had not used drugs such as anticholinergics, hypnotics, and antidiuretics that are commonly used in the treatment of nocturia. By excluding drugs commonly used in the treatment of nocturia and using loxoprofen for 3 months, we could show that loxoprofen was helpful in the rapid improvement of nocturia. However, this was a retrospective study in a small number of patients. Therefore, prospective research on a larger scale is necessary to prove the exact effect of loxoprofen on nocturia. Furthermore, additional research on the extent of reduction in nocturia and whether patients' quality of life is improved by the administration of the drug should be performed.
We evaluated the long-term effect of loxoprofen on nocturia for the first time. Among BPH patients with refractory nocturia, the number of nocturia episodes was reduced more in the loxoprofen group than in the control group after 3 months of loxoprofen treatment. Loxoprofen can be considered as one of the treatment options for rapid improvement in nocturia in BPH patients. It is recommended that loxoprofen be used for short periods of time in older patients considering the side-effects of long-term use of loxoprofen. Because our study was conducted on a small number of patients, the long-term effects and side-effects of loxoprofen should be studied further through large-scale studies on larger numbers of patients.
Figures and Tables
 | FIG. 1Degree of decrease in the number of episodes of nocturia compared with baseline after 3, 6, and 12 months of treatment in both groups. a: statistical significance between groups. |
References
1. Middelkoop HA, Smilde-van den Doel DA, Neven AK, Kamphuisen HA, Springer CP. Subjective sleep characteristics of 1,485 males and females aged 50-93: effects of sex and age, and factors related to self-evaluated quality of sleep. J Gerontol A Biol Sci Med Sci. 1996. 51:M108–M115.
2. Asplund R, Aberg H. Health of the elderly with regard to sleep and nocturnal micturition. Scand J Prim Health Care. 1992. 10:98–104.
3. Johnson TM 2nd, Jones K, Williford WO, Kutner MH, Issa MM, Lepor H. Changes in nocturia from medical treatment of benign prostatic hyperplasia: secondary analysis of the Department of Veterans Affairs Cooperative Study Trial. J Urol. 2003. 170:145–148.
4. Bruskewitz RC, Larsen EH, Madsen PO, Dørflinger T. 3-year followup of urinary symptoms after transurethral resection of the prostate. J Urol. 1986. 136:613–615.
5. Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. N Engl J Med. 1995. 332:75–79.
6. Matsuda K, Tanaka Y, Ushiyama S, Ohnishi K, Yamazaki M. Inhibition of prostaglandin synthesis by sodium 2-[4-(2-oxocyclopentylmethyl) phenyl] propionate dihydrate (CS-600), a new anti-inflammatory drugs, and its active metabolite in vitro and in vivo. Biochem Pharmacol. 1984. 33:2473–2478.
7. Sugimoto M, Kojima T, Asami M, Iizuka Y, Matsuda K. Inhibition of prostaglandin production in the inflammatory tissue by loxoprofen-Na, an anti-inflammatory prodrug. Biochem Pharmacol. 1991. 42:2363–2368.
8. Okada S, Watanabe H, Kojima Y, Yanai Y, Sasaki S, Kohri K. Loxoprofen sodium treatment for elderly men with refractory nocturia: effect on night-time urine production. Int J Urol. 2008. 15:462–464.
9. Saito M, Kawatani M, Kinoshita Y, Satoh K, Miyagawa I. Effectiveness of an anti-inflammatory drug, loxoprofen, for patients with nocturia. Int J Urol. 2005. 12:779–782.
10. Chang HS, Kim BK, Sohn JC, Park CH, Kim CI. Effectiveness of loxoprofen sodium on nocturia in patients with benign prostatic hyperplasia. Korean J Urol. 2007. 48:195–198.
11. Araki T, Yokoyama T, Kumon H. Effectiveness of a nonsteroidal anti-inflammatory drug for nocturia on patients with benign prostatic hyperplasia: a prospective non-randomized study of loxoprofen sodium 60 mg once daily before sleeping. Acta Med Okayama. 2004. 58:45–49.
12. Lee JG. Pathophysiology of male lower urinary tract symptoms. Korean J Urol. 2005. 46:887–896.
13. Presti JC Jr. Indomethacin and symptomatic relief of benign prostatic hyperplasia. JAMA. 1995. 273:347.
14. Maggi CA. Prostanoids as local modulators of reflex micturition. Pharmacol Res. 1992. 25:13–20.
15. Wen SF. Nephrotoxicities of nonsteroidal anti-inflammatory drugs. J Formos Med Assoc. 1997. 96:157–171.
16. Abrams PH, Feneley RC. The actions of prostaglandins on the smooth muscle of the human urinary tract in vitro. Br J Urol. 1975. 47:909–915.
17. Andersson KE, Ek A, Persson CG. Effects of prostaglandins on the isolated human bladder and urethra. Acta Physiol Scand. 1977. 100:165–171.
18. Andersson KE. Treatment of overactive bladder: other drug mechanisms. Urology. 2000. 55:5A Suppl. 51–57.
19. Palea S, Toson G, Pietra C, Trist DG, Artibani W, Romano O, et al. Pharmacological characterization of thromboxane and prostanoid receptors in human isolated urinary bladder. Br J Pharmacol. 1998. 124:865–872.
20. Urade Y, Hayaishi O. Prostaglandin D2 and sleep regulation. Biochim Biophys Acta. 1999. 1436:606–615.
21. Yoshida Y, Matsumura H, Nakajima T, Mandai M, Urakami T, Kuroda K, et al. Prostaglandin E (EP) receptor subtypes and sleep: promotion by EP4 and inhibition by EP1/EP2. Neuroreport. 2000. 11:2127–2131.
22. Waikakul S, Waikakul W. A post marketing survey on the side-effects of loxoprofen. J Med Assoc Thai. 1999. 82:721–726.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download