Abstract
Purpose
The effect of neoadjuvant hormonal therapy (NHT) on radical retropubic prostatectomy (RRP) for prostate cancer is various and remains a controversy for urologists. We conducted this study to comparatively evaluate whether NHT before RRP is indicated and beneficial in the aspects of postoperative complications, positive surgical margin, and biochemical recurrence.
Materials and Methods
Between September 2006 and December 2009, 69 men were scheduled for RRP as a treatment for clinically localized and locally advanced prostate cancer and were divided into two groups. Group 1 (n=31, 44.9%) was treated with RRP only, and group 2 (n=38, 55.1%) underwent RRP with preoperative NHT. We evaluated clinical parameters, surgical parameters, and the positive margin rate in surgical specimens and the biochemical recurrence rate.
Results
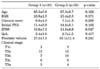
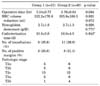
There were no statistical differences in age, body mass index (BMI), preoperative biopsy Gleason score, initial serum prostate-specific antigen (PSA) levels, International Prostate Symptom Score (IPSS), or quality of life (QoL) between the two groups (p>0.05). We also observed no differences in the transfusion rate, mean catheterization time, or positive margin rate (p>0.05). However, the mean operative time was significantly higher in the RRP with preoperative NHT group than in the other group (p=0.034). There was no significant difference in the biochemical recurrence rate during the last follow-up according to NHT (p=0.102) or positive surgical margin (p=0.473).
Prostate cancer is a major health public problem in men and the second leading cause of cancer death and the most common malignancy diagnosed in the United States. A total of 217,730 new prostate cancer cases and 32,050 deaths from prostate cancer are projected to occur in the United States in 2010 [1]. There are many management options for the early stage of prostate cancer, such as watchful waiting, radical prostatectomy, radiotherapy, and hormonal therapy, according to patients' performance status, patients' demands, and the doctor-patient relationship. However, the choice of management for localized prostate cancer has been radical prostatectomy for the complete removal of cancer cells [2]. Prostate cancer is frequently hormone dependent, and therefore anti-androgen therapy has been an important aspect of treatment for patients with prostate cancer. The goal of neoadjuvant hormonal therapy (NHT) before radical prostatectomy is to reduce the positive margin rate and the disease recurrence rate, but whether these goals are met remains controversial. Many arguments suggest that the apparent down-staging results from difficulty with the pathological evaluation of the neoadjuvantly treated prostatectomy specimen [3,4]. Song and Chang showed that most uro-oncologists in Korea perform hormonal treatment for patients with locally advanced or minimally metastatic prostate cancer and perform NHT before radical prostatectomy in 55% of cases [5]. In addition, many Koreans tend to hesitate to choose an operation for cancer treatment. Similarly, there were many cases in our hospital in which surgery was delayed because of patient demands. NHT before radical retropubic prostatectomy (RRP) was started as a result of patient desire to delay operation in our hospital. Therefore, we conducted this study to comparatively evaluate whether NHT before RRP is indicated and beneficial.
Between September 2006 and December 2009, we retrospectively analyzed the medical records of 69 prostate cancer patients who were treated with RRP in our hospital. All patients were suspected of having prostate cancer on the basis of positive results on a digital rectal examination, serum prostate-specific antigen (PSA) levels, and the results of transrectal ultrasound (TRUS). All patients underwent TRUS-guided prostate biopsy, and prostate cancer was confirmed by pathology. A total of 31 patients (group 1, 44.9%) underwent RRP only, and 38 patients (group 2, 55.1%) were treated with RRP and a mean of 3 months of NHT. NHT was started to delay RRP due to patient demands. NHT comprised a combined androgen blockade with luteinizing hormone-releasing hormone analogue (goserelin acetate, Zoladex®) injections monthly and antiandrogen (bicalutamide 50 mg, Casodex®) daily. We evaluated patient age, body mass index (BMI), preoperative biopsy Gleason score, initial serum PSA levels, International Prostate Symptom Score (IPSS), quality of life (QoL), TRUS-guided prostate volume, and clinical stage. Clinical stage was established by computer tomography, magnetic resonance imaging, and bone scanning. All patients were younger than 75 years of age and had a serum PSA of less than 50 ng/ml. Exclusion criteria included prior treatment with radiation therapy, concomitant use of medications with antiandrogenic activity, prior history of cancer, or severe renal or hepatic impairment. RRP with pelvic lymphadenectomies was performed according to the standard method. Pelvic lymph node dissection was routinely performed during radical prostatectomy. All of the histological slides were sent to the pathologist in our hospital to standardize histopathological examination. We recorded all patients' postoperative pathologic stage. The stage and tumor grade were assessed by use of the 2009 TNM staging system. The operative time, blood loss, catheterization time, transfusion rate, intraoperative and postoperative complications, positive margin rate, and biochemical recurrence rate were compared among the two groups. Follow-up evaluations measured serum PSA every 3 months for 1 year postoperatively and every 6 months thereafter. Biochemical recurrence was defined as a serum PSA level of 0.2 ng/ml or greater on two consecutive evaluations.
SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The independent-sample t-test was used to compare different group variables, and the chi-square test was used to compare nominal data. Kaplan-Meier curves were used to present survival until biochemical recurrence in the 2 treatment groups. p-values less than 0.05 were considered statistically significant.
All patients undergoing NHT showed good tolerance to goserelin acetate and bicalutamide. No patients experienced severe hepatic dysfunction, renal failure, gastrointestinal reactions, or cardiovascular effects. Mean patient age (±SD) was 65.3±5.8 and 67.3±5.7 years in the two groups (p=0.162). There were no statistical differences in patient BMI, Gleason score of prostate biopsy, initial serum PSA levels, IPSS, QoL, or mean TRUS-guided prostate volume between the two groups. The patients' characteristics at the time of diagnosis are presented in Table 1. The preoperative clinical stage was compared between the two groups, and the two groups were found to be equally balanced for clinical stage. Also, there were no cases that extended to the seminal vesicle on magnetic resonance imaging.
There were no statistical differences in postoperative parameters, such as red blood cell volume reduction, hemoglobin decrement, catheterization time, transfusion rate, or positive margin rate, except for operative time. Also, the postoperative pathologic stages were compared between the two groups (Table 2). The two groups were also equally balanced for pathologic stage. Pelvic lymph node dissection showed no lymph node metastasis in any of the patients. Operative time was 3.34±0.77 and 3.76±0.84 hours in the two groups. Operative time was longer for the men who received NHT than for those who had not received NHT, and the difference between the two groups was significant (p=0.034). Also, in the Pearson's correlation analysis, operative time was positively correlated with cycles of NHT (r=0.28, p<0.019).
Fig. 1 shows the proportion of men without PSA failure during the follow-up period among men treated by RRP alone and among those treated by RRP with preoperative NHT. During the follow-up period, PSA recurrence-free survival was higher among men who had not received NHT than among those who had received NHT. The mean biochemical recurrence period was 32±3 months in the non-NHT group and was 24±3 months in the NHT group. However, there was no significant difference in the biochemical recurrence rate at the last follow-up according to NHT (log-rank test, p=0.102) or positive margin rate (logrank test, p=0.473).
Some postoperative complications were recorded: one anastomotic leakage in group 1 and one in group 2. There were no anastomotic strictures or rectovesical fistulas. No patients had rectal injuries, and there was no mortality in this series.
Of the management options for prostate cancer, radical prostatectomy and radiotherapy are the most widely accepted treatments for patients with early stage disease who require intervention. The main curative form of treatment for localized prostate cancer is radical prostatectomy [6]. It is reasonable to offer radical prostatectomy for the cure of localized prostate cancer. However, for nearly 66% of men undergoing prostatectomy, the preoperative clinical stage underestimates the extent of disease, and the positive margin rate may be as high as 30% to 60% [7]. The first use of gonadotropin-releasing hormone agonists in prostate cancer was for the palliation of metastatic disease [8]. The rationale for NHT evolved from the need to decrease the high positive margin rate following radical prostatectomy and to reduce the clinical recurrence rate. The development of safe, potent, and reversible agents for NHT provided a well-tolerated method for inducing prostate cancer cell death and tumor regression before radical prostatectomy. There is no consensus in the medical literature, however, as to whether radical prostatectomy after NHT is of greater, equal, of lesser difficulty than radical prostatectomy in patients who have not received NHT [9].
The role of NHT before radical prostatectomy remains controversial. According to Monfette et al, an advantage of hormonal treatment is a decrease in blood loss and operative difficulty after hormonal treatment [10]. This point of view states that NHT decreases the operative parameters and may make the operation easier. However, Soloway et al found that NHT makes the operation more difficult because of intense periprostatic reaction together with seminal vesicle adhesions, but that this had no effect on operative time or intraoperative bleeding [11]. This point of view states that NHT before radical prostatectomy may make the operation more difficult.
In our series, we compared the effect of prolonged NHT and no NHT on the outcome of operative parameters and found no effect on operative parameters except for operative time. Mean operative time was 3.34±0.77 and 3.76±0.84 hours in the two groups. There was a significant difference between the two groups (p=0.034). According to Macfarlane et al, NHT has no effect on operative parameters [3]. After 3 months of neoadjuvant treatment, 18 patients with clinical stage B2 or C prostate cancer had an average estimated blood loss of 1,238 ml and an average operative time of 183 minutes [3]. At the same time, a historical control group of 20 patients with pathological stage B2 disease had an average blood loss of 1,296 ml and an average operative time of 171 minutes, which were similar results. Goldenberg et al randomly assigned 192 patients to surgery alone (n=91) or a 12-week course of cyproterone acetate (n=101) [12]. There were no significant differences in surgical difficulty, intraoperative blood loss, or the number of patients requiring transfusion. Schulman et al compared 400 patients with prostate cancer who were randomly assigned to direct surgery (n=209) or to NHT for 3 months (n=191) before radical prostatectomy [13]. The mean duration of surgery was 159 and 163 minutes, and mean blood loss was 1,150 and 1,082 ml, in the direct surgery and NHT before surgery groups, respectively. Meyer et al found similar blood loss and shorter operative times in 292 patients undergoing more than 3 months of NHT than in 388 patients treated with radical prostatectomy alone [14]. Similarly, Gleave et al reported a mean blood loss of 826 versus 761 ml in the 3- and 8-month groups, respectively, and no major intraoperative morbidity [15].
The positive surgical margin rate is an important independent prognostic factor, and the presence of a positive surgical margin was associated with the greatest relative risk. Prostate cancer is curable only when treated at an early stage, when the tumor is still localized to the prostate gland [16]. In fact, most clinical studies show decreases in the positive margin rate up to 50% after 3 months of NHT [17]. Gao et al compared 31 patients with prostate cancer who underwent radical prostatectomy; of these, 12 patients underwent preoperative hormonal deprivation [18]. There was a higher positive surgical margin rate and extracapsular extension and greater seminal vesicle invasion in the direct radical prostatectomy group than in the NHT group before radical prostatectomy (p<0.05), but there were no significant differences in operative time or blood loss between the two groups. The mean operative time was 3.2±0.4 and 3.8±0.7 hours, and the mean blood loss was 760±431 ml and 771±397 ml, in the direct surgery and NHT groups, respectively.
Recently, laparoscopic radical prostatectomy (LRP) has emerged as a treatment modality for localized prostate cancer that seeks to combine the benefits of a minimally invasive approach. Some studies of NHT on the outcome of LRP have been conducted. Androgen deprivation before LRP may increase the subjective technical difficulty but it does not have any major impact on the outcome of LRP and shows no difference in the positive surgical margin rate [19-21]. In our series, there was also no difference in the positive margin rate (p=0.642). In addition, we observed that patients who received NHT for about 3 month before RRP had no statistically significant survival advantage compared with those treated by RRP alone.
In conclusion, our study showed a difference in the effect of NHT before RRP on operative time, which was higher because of the slightly greater technical difficulty of RRP. Also, according to Pearson's correlation analysis, a prolonged NHT cycle can increase the operative time (r=0.28, p<0.019). It is our opinion that NHT before RRP should not be performed for several reasons. First, we found that RRP was more difficult to execute because of the periprostatic fibrosis that occurs in response to the apoptosis caused by NHT. Second, estimated blood loss, transfusion rate, postoperative complications, positive margin rate, and the biochemical recurrence rate appeared to be equivalent in the two groups. Third, patients with prostate cancer who undergo long-term NHT are at greater risk of developing dyslipidemia, insulin resistance, and metabolic syndrome [22]. These metabolic and physiological changes are a direct result of the induced higher risk of cardiovascular morbidity and diabetes mellitus [23-25]. Therefore, understanding the impact of the use of NHT in localized prostate cancer patients is important, and the consequences of NHT are worthy of further clinical research.
A limitation of our study is that the sample size of both groups was small, and this was a retrospective analysis with a short postoperative follow-up period, which allows for potential selection bias. Further large, prospective investigations and long-term follow-up will be required to fully evaluate the efficacy results.
Preoperative NHT may increase the technical difficulty of RRP, but our results do not allow us to reach any major conclusions. NHT is associated with significant side effects, such as hot flushes and gynecomastia, metabolic syndrome, and cardiovascular morbidity, and has cost implications. The decision to use hormone therapy should, therefore, be made at a local level, between the patient and the clinician and should take into account the clinical benefits, toxicity, and cost. We suggest that more research is needed to guide the choice, the duration, and the schedule of NHT and the impact of long-term hormone therapy on toxicity and the patient's QoL.
Figures and Tables
FIG. 1
Kaplan-Meier curves for prostate-specific antigen (PSA) recurrence free survival until PSA failure according to treatment regimen. Biochemical recurrence rate does not show any significant difference between 2 arms. log-rank test, p=0.102.

References
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010. 60:277–300.
2. Jani AB, Hellman S. Early prostate cancer: clinical decision-making. Lancet. 2003. 361:1045–1053.
3. Macfarlane MT, Abi-Aad A, Stein A, Danella J, Belldegrun A, deKernion JB. Neoadjuvant hormonal deprivation in patients with locally advanced prostate cancer. J Urol. 1993. 150:132–134.
4. Paulson DF. Neoadjuvant androgen-deprivation therapy prior to radical prostatectomy: con. Urology. 1996. 48:539–540.
5. Song J, Chang K. Current status of hormonal therapy for prostate cancer in Korea: a national survey of Korean uro-oncologists. Korean J Urol Oncol. 2003. 1:175–180.
6. Sriprasad S, Feneley MR, Thompson PM. History of prostate cancer treatment. Surg Oncol. 2009. 18:185–191.
7. Hurtado-coll A, Goldenberg SL, Klotz L, Gleave ME. Preoperative neoadjuvant androgen withdrawal therapy in prostate cancer: the Canadian experience. Urology. 2002. 60:3 Suppl 1. 45–51.
8. Fair WR, Aprikian AG, Cohen D, Sogani P, Reuter V. Use of neoadjuvant androgen deprivation therapy in clinically localized prostate cancer. Clin Invest Med. 1993. 16:516–522.
9. Civantos F, Sadek S, Öbek C, Lai S, Soloway M. Neoadjuvant hormonal therapy prior to radical prostatectomy. Mol Urol. 1999. 3:201–204.
10. Monfette G, Dupont A, Labrie F. Labrie F, editor. Temporary combination therapy with flutamide and tryptex as adjuvant to radical prostatectomy for the treatment of early stage prostate cancer. Early stage prostate cancer: diagnosis and choice of therapy. 1989. New York: Elsevier Science;41–51.
11. Soloway MS, Sharifi R, Wajsman Z, McLeod D, Wood DP Jr, Puras-Baez A. The Lupron Depot Neoadjuvant Prostate Cancer Study Group. Randomized prospective study comparing radical prostatectomy alone versus radical prostatectomy preceded by androgen blockade in clinical stage B2 (T2bNxM0) prostate cancer. J Urol. 1995. 154:424–428.
12. Goldenberg SL, Klotz LH, Srigley J, Jewett MA, Mador D, Fradet Y, et al. Canadian Urologic Oncology Group. Randomized, prospective, controlled study comparing radical prostatectomy alone and neoadjuvant androgen withdrawal in the treatment of localized prostate cancer. J Urol. 1996. 156:873–877.
13. Schulman CC, Debruyne FM, Forster G, Selvaggi FP, Zlotta AR, Witjes WP. European Study Group on Neoadjuvant Treatment of Prostate Cancer. 4-year follow-up results of a European prospective randomized study on neoadjuvant hormonal therapy prior to radical prostatectomy in T2-3 N0M0 prostate cancer. Eur Urol. 2000. 38:706–713.
14. Meyer F, Moore L, Bairati I, Lacombe L, Têtu B, Fradet Y. Neoadjuvant hormonal therapy before radical prostatectomy and risk of prostate specific antigen failure. J Urol. 1999. 162:2024–2028.
15. Gleave ME, Goldenberg SL, Chin JL, Warner J, Saad F, Klotz LH, et al. Randomized comparative study of 3 versus 8-month neoadjuvant hormonal therapy before radical prostatectomy: biochemical and pathological effects. J Urol. 2001. 166:500–506.
16. Pendleton J, Pisters LL, Nakamura K, Anai S, Rosser CJ. Neoadjuvant therapy before radical prostatectomy: Where have we been? Where are we going? Urol Oncol. 2007. 25:11–18.
17. Schulman CC. Neoadjuvant androgen blockade prior to prostatectomy: a retrospective study and critical review. Prostate Suppl. 1994. 5:9–14.
18. Gao X, Zhou T, Tang YJ, Lu X, Sun YH. Neoadjuvant hormonal deprivation for patients undergoing radical prostatectomy. Asian J Androl. 2009. 11:127–130.
19. Pu XY, Wang XH, Wu YL, Wang HP. Comparative study of the impact of 3-versus 8-month neoadjuvant hormonal therapy on outcome of laparoscopic radical prostatectomy. J Cancer Res Clin Oncol. 2007. 133:555–562.
20. Maldonado-Valadez R, Teber D, Erdogru T, Safi KC, Frede T, Rassweiler J. The impact of neoadjuvant hormonal therapy on the outcome of laparoscopic radical prostatectomy: a matched pair analysis. J Urol. 2006. 175:2092–2096.
21. Brown JA, Garlitz C, Strup SE, Hubosky SG, Gomella L. Laparoscopic radical prostatectomy after neoadjuvant hormonal therapy: an apparently safe and effective procedure. J Laparoendosc Adv Surg Tech A. 2004. 14:335–338.
22. Hakimian P, Blute M Jr, Kashanian J, Chan S, Silver D, Shabsigh R. Metabolic and cardiovascular effects of androgen deprivation therapy. BJU Int. 2008. 102:1509–1514.
23. Nanda A, Chen MH, Braccioforte MH, Moran BJ, D'Amico AV. Hormonal therapy use for prostate cancer and mortality in men with coronary artery disease-induced congestive heart failure or myocardial infarction. JAMA. 2009. 302:866–873.
24. D'Amico AV, Denham JW, Crook J, Chen MH, Goldhaber SZ, Lamb DS, et al. Influence of androgen suppression therapy for prostate cancer on the frequency and timing of fatal myocardial infarctions. J Clin Oncol. 2007. 25:2420–2425.
25. Keating NL, O'Malley AJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J Clin Oncol. 2006. 24:4448–4456.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download