Abstract
The use of graft materials in bladder mucosa has been examined in animal models, but debate exists over which materials are effective. Intestine has been used as a substitute in augmentation cystoplasty for patients with neuropathic bladder, but serious adverse effects of the operation have occurred in some instances. We report a case of a successful repair of an enterovesical fistula by use of bovine pericardium. The patient has remained well for 2.5 years. We suggest that bovine pericardium may be a suitable option as a bladder substitute.
Many experimental trials of organic materials as bladder wall substitutes have been performed in animal models, but the results have been variable [1-3]. In cases of intractable neuropathic bladder, urologists often attempt augmentation cystoplasty with intestine only as the last option. However, this has led to complications in many cases [4]. We treated a case of enterovesical fistula with the use of a bovine pericardium (BP) substitute. In this case, the patient had a past history of several operations and radiation treatment. In the operative field, after the fistula site was removed, the bladder wall defect was too large to repair and the mucosa was crumbled. Intestinal adhesion was very severe and the state of the intestine was very poor. Therefore, cystoplasty using intestine was ruled out as an option. Instead, we used BP owing to its high strength and minimal infection rate in other reported abdominal and urologic surgeries [5-8]. We are not aware of any previous reports of successful use of graft material as a human bladder wall substitute. Here we report this case of successful enterovesical fistula repair using BP with a brief review of the literature.
A 67-year-old woman visited our clinic complaining of fecal material in her urine 2 days previously. She had undergone a radical hysterectomy and radiation therapy 23 years previously owing to cervical cancer. She had a history of choledochojejunostomy 13 years ago, and suffered from radiation cystitis and recurrent acute pyelonephritis. She had initially attended our clinic 10 years previously complaining of intractable daytime frequency, urgency, urge incontinence, and suprapubic pain. At that time, she complained of voiding at 5- to 10-minute intervals in the daytime and 15 to 20 times overnight. Cystoscopy and urodynamic study were performed to find the cause of her voiding symptoms. Her bladder capacity was about 50 cc and she felt severe pain with instillation above 50 cc. Under the diagnosis of a contracted bladder due to radiation therapy, she was offered augmentation cystoplasty about 10 years ago, but she refused any operative treatment. To control her voiding symptoms, she took anticholinergic medication for several months but her voiding symptoms did not improve. She therefore kept a Foley catheter to relieve the uncontrolled voiding symptoms and had changed the urethral Foley catheter once a month for 10 years at a local clinic. To identify the cause of this recurrent acute pyelonephritis, she underwent voiding cystoureterography and was diagnosed as having grade II vesicoureteral reflux. After that, she had taken prophylactic antibiotic medication.
Physical examination showed mild tenderness of the lower abdomen. On urinalysis, many white and red blood cells were observed, and Escherichia coli was cultured in the urine sample. Her blood urea nitrogen/creatinine level was 30/2.6 mg/dl. Cystoscopy revealed yellow debris resembling fecal material floating in the bladder and a red ulcerative lesion at the dome of the bladder. The bladder mucosa was pale and edematous but no fistula was observed. Abdominal computed tomography revealed bilateral renal cortical thinning, hydroureteronephrosis, and wall thickening of the proximal ureter and pelvis. In addition, adhesion between the anterosuperior aspect of the bladder wall and the terminal ileum was observed. The cause of the elevated nitrogen/creatinine level was thought to be decreased renal function due to chronic vesicoureteral reflux.
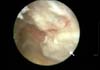
Under the presumptive diagnosis of an enterovesical fistula, cystography was performed. In the cystography, the dye instilled into the bladder was seen to enter the terminal ileum (Fig. 1). Under the diagnosis of an enterovesical fistula, cystoplasty was planned. In the field of the operation, severe adhesion of the bladder wall to the pelvic wall was seen, and the bladder wall was in a crumbling state. Adhesion of the intestine was very severe, and it was very difficult to dissect the fistula site. A general surgeon resected the fistula site and anastomosed the colon. Thereafter, the defect of the dome site of the bladder wall was identified and measured at 2.4×2 cm (Fig. 2A). We tried to anastomose the defect, but it was too large to repair, and the bladder wall had no elasticity. Therefore, it was impossible to close the defect, and augmentation cystoplasty using the intestine was contraindicated because of the poor state of the intestine due to the previous radiation therapy. Therefore, we decided to repair the bladder wall defect with BP (Supple Peri-Guard®, Synovis®). In the operating room, we explained to the patient's son the state of the patient's bladder and intestine and about the uncertain safety of BP and possible complications after operation with BP. He agreed to the operation using BP and we started the operation. We tailored the BP to the size of the defect and closed the site with Vicryl 3-0 (Fig. 2B). After the operation, a 16 Fr Foley catheter was inserted into the bladder. When we performed cystography in postoperative weeks 3 and 6, dye leakage was seen, but by postoperative week 8 it was no longer observed, although vesicoureteral reflux and contracted bladder remained. We tried to persuade the patient to remove the Foley catheter and to undertake self-voiding. However, the patient was worried about the recurrence of severe voiding difficulty including frequency and urgency and did not permit the removal of the Foley catheter. The patient retained the urethral Foley catheter when she was discharged and we changed it every month. Six months after the operation, we again performed a cystoscopy and the BP was intact. At postoperative year 1, we removed the catheter. We persuaded the patient to undertake self-voiding and prescribed tolterodine 4 mg to control frequency. After administration of tolterodine for three days, she complained of abdominal distension and pain. Under the diagnosis of functional bowel obstruction due to the side effect of the anticholinergic action of tolterodine, conservative management was done for the bowel obstruction. The patient recovered without complications. After that, she refused further administration of anticholinergics because of the expected side effect of the drug. Her frequency problems still remained, so she wanted to restore the urethral Foley catheter to relieve the voiding symptoms and to change it every month instead of self-voiding with medication. The patient was followed every month in our clinic. Her follow-up blood urea/nitrogen level was 29/2.1 mg/dl. Cystoscopy was performed postoperatively 2.5 years later. The BP observed at the dome of the bladder wall remained intact (Fig. 3).
The causes of enterovesical fistulas are diverticular diseases, colon cancer, Crohn's disease, radiation, and trauma [4]. In the present case, the patient had a history of radiation, several laparotomies, and maintenance of a chronic indwelling urethral catheter. It is possible that multiple factors of this kind contributed to the development of the enterovesical fistula as in a similar case reported previously by Hawary et al [9]. Our patient's loss of bladder wall was very severe after resection of the fistula site, and her bladder capacity was too small. Moreover, her intestine was in a bad state owing to her previous radiation history, so we could not use it as a substitute for the bladder wall.
When there is a severe loss of bladder wall or a marked decrease of bladder contractility, urologists generally use intestine as a substitute for the bladder mucosal wall. However, such augmentation cystoplasty is associated with metabolic acidosis, recurrent urinary tract infection, calculus, and risk of cancer [4]. Researchers have studied the use of biodegradable substitutes for the bladder mucosa, one of which is BP. Natural biomaterials can serve as scaffolds for cell attachment, migration, and proliferation. Also, these have the desired shape and strength [10].
The Supple Peri-Guard® used in this case is BP composed of biocompatible multi-directional collagen fibers cross-linked with glutaraldehyde. Supple Peri-Guard® is usually used as a prosthesis for surgical repair of soft tissue deficiencies including the abdominal and thoracic wall, gastric bindings, muscle flap reinforcement, and hernias. Although BP is biocompatible, it can cause some adverse reactions, including calcification, infection, rejection, adhesion, erosion, and allergic reactions.
BP has been used for a long time in cardiovascular surgery, and there is evidence of its safety and of few long-term morphological changes. BP has also been used as a graft material in a variety of operations, and successful outcomes have been reported [5-7]. Limpert et al reported the use of BP in a complex abdominal wall reconstruction of a failed ventral hernia repair in which prosthetic mesh had failed or was contraindicated [5]. The hernia recurrence was 19% and BP's high strength, minimal infection rate, and low cost allowed its use in the reconstruction of complex abdominal defects.
In ophthalmologic surgery, BP was successfully used to treat a large corneal perforation secondary to alkali injury [6]. Tracheal reconstruction with a BP patch after iatrogenic membranous tracheal wall rupture has also been reported [7]. BP has also been used in urologic surgery, in an experimental study of the application of urethroplasty, and good results were reported [8]. However, there have been only a few experimental studies of bladder substitution with the use of BP, and the results were variable [1-3]. In experiments in animal models, BP acted as a scaffold for regeneration of the bladder mucosa [1,2].
In one experimental study comparing the effectiveness of several biodegradable materials for bladder augmentation in a minipig model, the BP patch graft failed to be incorporated into the bladder mucosa [3]. However, there have been no previous reports of the use of BP as a graft material for bladder substitution.
To our knowledge, this is the first report of a successful cystoplasty using BP in the human bladder without any complications. Our results suggest that BP is a candidate graft material for bladder substitution. However, further study is needed to identify the safety and effectiveness of BP as a graft material for bladder substitution.
Figures and Tables
FIG. 1
Cystography revealed a fistula tract between the contracted urinary bladder and the terminal ileum.

References
1. Novick AC, Straffon RA, Koshino I, Banowsky LH, Levin H, Kambic H. Experimental bladder substitution using a biodegradable graft of natural tissue. J Biomed Mater Res. 1978. 12:125–147.
2. Kambic H, Kay R, Chen JF, Matsushita M, Harasaki H, Zilber S. Biodegradable pericardial implants for bladder augmentation: a 2.5-year study in dogs. J Urol. 1992. 148:539–543.
3. Portis AJ, Elbahnasy AM, Shalhav AL, Brewer A, Humphrey P, McDougall EM, et al. Laparoscopic augmentation cystoplasty with different biodegradable grafts in an animal model. J Urol. 2000. 164:1405–1411.
4. Venn S, Mundy T. Bladder reconstruction: urothelial augmentation, trauma, fistula. Curr Opin Urol. 2002. 12:201–203.
5. Limpert JN, Desai AR, Kumpf AL, Fallucco MA, Aridge DL. Repair of abdominal wall defects with bovine pericardium. Am J Surg. 2009. 198:e60–e65.
6. Khanna R, Mokhtar E. Bovine pericardium in treating large corneal perforation secondary to alkali injury: a case report. Indian J Ophthalmol. 2008. 56:429–430.
7. Barbetakis N, Samanidis G, Paliouras D, Lafaras C, Bischiniotis T, Tsilikas C. Intraoperative tracheal reconstruction with bovine pericardial patch following iatrogenic rupture. Patient Saf Surg. 2008. 2:4.
8. Ayyildiz A, Celebi B, Akgül KT, Nuhoğlu B, Caydere M, Germiyanoğlu C. A comparison of free skin graft, fascia lata, alloderm, bovine pericardium and primary repair in urethrocutaneous fistulas without diversion: an experimental study. Pediatr Surg Int. 2006. 22:809–814.
9. Hawary A, Clarke L, Taylor A, Duffy P. Enterovesical fistula: a rare complication of urethral catheterization. Adv Urol. 2009. 591204.
10. Lai PH, Chang Y, Liang HC, Chen SC, Wei HJ, Sung HW. Peritoneal regeneration induced by an acellular bovine pericardial patch in the repair of abdominal wall defects. J Surg Res. 2005. 127:85–92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download